A Case Report of Beckwith-Weidemann Syndrome: An Overgrowth Anomaly
Monika Jindal1, Santosh Minhas2, Monika Sharma3, Jaspreet Singh4
1 Professor, Department of Obstetrics and Gynaecology, Maharishi Markandeshwar Medical College and Hospital, Solan, Himachal Pradesh, India.
2 Professor and Head, Department of Obstetrics and Gynaecology, Maharishi Markandeshwar Medical College and Hospital, Solan, Himachal Pradesh, India.
3 Associate Professor, Department of Radiodiagnosis, Maharishi Markandeshwar Medical College and Hospital, Solan, Himachal Pradesh, India.
4 Senior Resident, Department of Radiodiagnosis, Maharishi Markandeshwar Medical College and Hospital, Solan, Himachal Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Monika Jindal, Professor, Department of Obstetrics and Gynaecology, Maharishi Markandeshwar Medical College, Kumarhatti, Solan, Himachal Pradesh, India.
E-mail: monikajindal@rocketmail.com
Beckwith-Wiedemann Syndrome (BWS) is an overgrowth anomaly of congenital origin that has low prevalence. However, among the congenital anomalies of overgrowth, it has high prevalence. Typical features are macroglossia, macrosomia, omphalocele and anterior abdominal wall defects. Though Genetic, but it’s mechanism of occurrence is not clear. Many researchers have found correlation between methodology of Assisted Reproductive Techniques and BWS. Future research for the improvement of the prenatal diagnostic techniques would help the multidisciplinary team to treat these congenital diseases. In the present case, the diagnosis of BWS was made by ultrasound conducted in Radiology Department after filling Preconception and Prenatal Diagnostic Techniques (PCPNDT) form in the institute at gestation of 29+6 weeks and after two days of diagnosis, unfortunately patient reported to our hospital emergency with intrauterine foetal demise.
Congenital, Foetus, Genetic disorder, Ultrasonography
Case Report
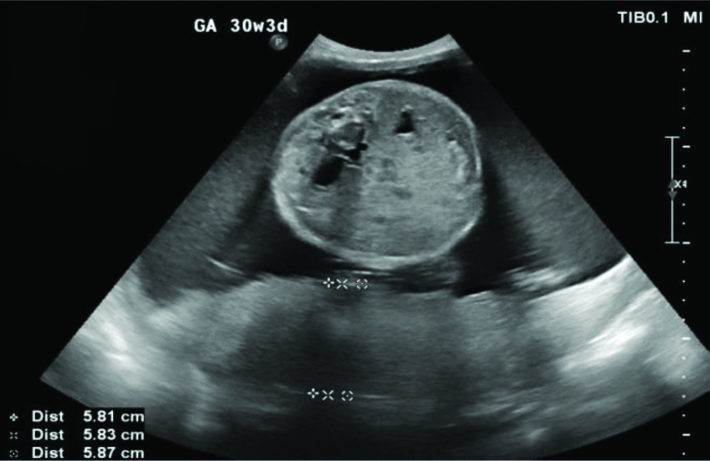
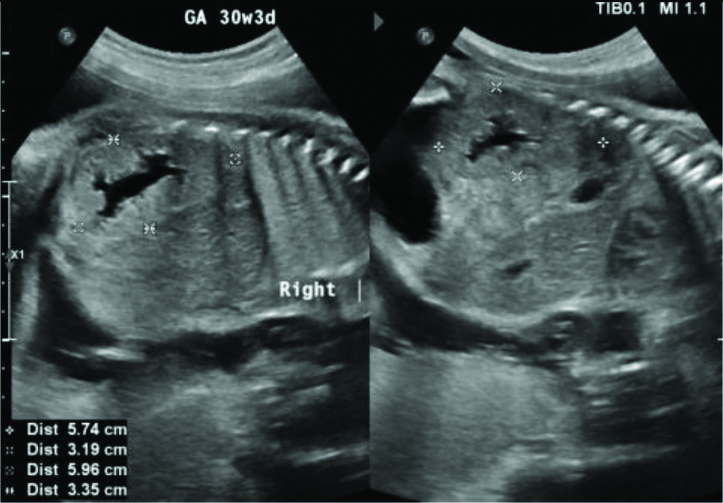
A 28-year-old primigravida, married (non-consanguineous) since 5 years, booked case of Obstetrics and Gynaecology Department at MMMCH, Solan reported in May 2020 in emergency. Patient had spontaneous conception and was normotensive, nondiabetic, euthyroid, Rh negative. Indirect Coomb’s Test (ICT) was negative. Patient had no significant medical, family, past or personal history. Anomaly scan done at gestation of 18+1 weeks was reported normal by radiology Department of our institute. Patient had a history of admission at 21+4 weeks of gestation for Upper Respiratory Tract Infection (URTI), managed medically. Due to Corona pandemic lockdown, she reported to hospital late for her routine Absolute Neutrophil Count (ANC) at 29+6 weeks of gestation and got her USG done, as advised by her treating consultant, because on abdominal examination her uterine fundal height was greater than duration of amenorrhoea and has clinical evidence of polyhydramnios. USG showed single live intrauterine foetus with mean ultrasound gestational age of 31week 6 days in cephalic presentation with polyhydraminos (AFI- 28-29 cm), placentomegaly (5.8 cm in maximum thickness) as shown in [Table/Fig-1] with short lower limbs. Bilateral foetal kidneys were enlarged with dilated pelvicalyceal systems (AP transverse diameter of right renal pelvis- 11.7 mm and left kidney- 11.9 mm) as shown in [Table/Fig-2]. Hepatomegaly along with macroglossia [Table/Fig-3,4] was appreciated and prenatal diagnosis of BWS was considered as per the ultrasound findings. Other differential diagnosis of diabetic foetopathy was also given by radiology department. She was called for routine follow-up after 2 weeks and prophylactic anti-D were given as patient was Rh –ve with ICT negative, but she reported to hospital after three days with the complaint of absent foetal movements since one day.
Trans-abdominal ultrasound shows enlarged placenta, measuring 5.8 cm in maximum thickness.
Trans-abdominal ultrasound shows enlarged foetal kidneys bilaterally with dilated pelvicalyceal systems.
Trans-abdominal ultrasound shows Macroglossia and tongue protruding out of the mouth in face profile view.

Trans-abdominal ultrasound shows foetal spleen is enlarged, measuring 3.7 cm.

On per abdominal examination fundal height was 34 weeks, cephalic presentation, liquor excess, uterus was relaxed, foetal heart beat was not localised by stethoscope and findings were again confirmed by USG and the diagnosis of Intrauterine Fetal Demise (IUFD) was given. On per vaginal examination, cervix was 2 cm dilated, soft, mid position, 10-20% effaced, membranes present, presenting part high up. Bishop score was 4. After explaining prognosis and taking informed consent, pregnancy was terminated. After delivery, foetal weight was 2.2 kg, large for given gestational age. On gross examination of foetus, macroglossia was present, abdomen was mildly distended. Patches of peeling of skin were present [Table/Fig-5]. No other gross congenital abnormality was present with HC-26 cm, Chest Circumference-25 cm, Abdominal Circumference 26 cm. All body openings were patent. Placenta weight was 1 kg, cord was oedematous with length 45 cm. Placenta was sent for gistopathological examination. Histopathology of placental specimen revealed features of mature placenta and ischaemia. Foetal autopsy was refused by parents and cord blood could not be sent for further genetic evaluation as we don’t have in-house facility for same and patient was not able to afford it due to financial constraints.
Postdelivery foetus showing features of BWS as seen on antenatal ultrasound with edematous umbilical cord.

Discussion
Beckwith-Wiedemann Syndrome (BWS)- a syndrome of overgrowth is also known as Exomphalos- Macroglossia-Gigantism Syndrome. BWS occurs due to disturbed balance of genes located at 11p15 that are organised in 2 separate domains. Domain 1 has paternally expressed Insulin-like Growth Factor (IGF2) along with genes and transcripts controlling expressions of IGF2. Domain 2 has many imprinted genes like CDKNIC and KCNQ10T1 (L1T1) [1]. The diagnosis of BWS is based upon a characteristic clinical picture, not on any specific diagnostic test. Demonstration of any genetic abnormality depends upon sophisticated techniques those are beyond the scope of standard labs [2]. It presents with larger birth weights, after birth Gigantism, large tongue, face and cranium abnormalities, anomalies like hernia and omphalocele related to umbilicus, anomalies of earlobe, capillary facial flame nevus, hypoglycaemia, cardiac defects and occasionally hepatomegaly, hemi-hypertrophy and certain embryonic tumours [1-3]. Excess of IGF-II (encoded by IGF 2) may contribute towards BWS and its incidence is 1 in 13,700 births [4].
As per Elliott M et al., criteria either 3 major or 2 major and 3 minor findings contribute to BWS. Major features being: 1) Anterior abdominal wall defects; 2) Large Tongue; 3) Overgrowth in ante and post-natal period and minor findings are: 1) Ear pit; 2) Nevus flammeus; 3) Neonatal hypoglycaemia; 4) Nephromegaly; 5) Hemi- hyperplasia [5].
Children born through in-vitro fertilisation have increased chance (3-4 folds) of developing BWS. IVF procedures are thought to be turning on or off the genes [6]. But this was not found in the present case, the patient conceived spontaneously. In 1963, Beckwith described a syndrome characterised by Omphalocele, Macroglossia and Visceromegaly and almost at same time Wiedmann also described similar clinical picture in three siblings [7]. Majority cases are sporadic and only 15% are familial [8]. Patients with familial history can be linked with autosomal dominant transmission of genes of parent-of-origin [9].
These patients of BWS can be diagnosed antenatally as well as postnatally by examination clinically and/or genetically by molecular diagnosis. Antenatal diagnosis is made by USG that shows excessive liquor, increased growth between 25-36 weeks of gestation, that may or may not be associated with Omphalocele. This alerts the physician towards the possible diagnosis of BWS [9]. Similar findings were observed in the present case. Macroglossia (a prominent feature) is observed in >90% of BWS cases [10]. Isolated hemi hypertrophy is associated with higher risk for cancer [11,12]. At birth there is relatively high incidence of prematurity. Infant mortality rate is expected to be as high as 21%, [9] but in the present case there was intrauterine death and the baby had macroglossia (a common and prominent feature of BWS).
BWS spectrum varies from Classic or Typical BWS, Atypical BWS to Isolated lateralised overgrowth. Some new-born with BWS may have hypoglycaemia or hyperinsulinemia because of excessive growth and secretion of insulin by the pancreas. Fortunately, affected individuals who could survive the infant age, are generally healthy. Mental growth may be normal or may have mild to moderate mental retardation [1]. These patients have more risk of cancers like Embryonic Tumours (6.5%), Wilms tumour, Hepatoblastoma, Neuroblastoma and Rhabdomyosarcoma during childhood [4]. A 6 monthly USG and Alfa-Feto-Protein (AFP) are advised to rule out Wilms tumour and Hepatoblastoma.
With advancement in technology, diagnosis of BWS can be made with increased certainty [13] and ultrasound is found to be an useful tool for diagnosis in prenatal period, as on one hand, diagnosis during prenatal time prepares and motivates the parents to have a periodic follow up because of the possibility of tumour development, and genetic counselling in future pregnancies and on other hand it permits us to plan treatment options needed for the management of abnormalities present in the child, like omphalocele/umbilical hernia.
Artificial Reproductive Technique (ART) has been found to be having correlation with epigenetic syndromes like BWS and Angelman syndrome. A retrospective case control study conducted in Australia found a risk of 1 in 4000 of BWS in the in-vitro population which was several times higher than their general population [14]. Another study showed three to four times more risk in conceptions by invitro [15]. No specific technique of ART was found to be more closely associated with BWS [11]. The treatment of BWS is directed toward the specific symptoms apparent in each individual and requiring coordinated efforts of multidisciplinary team. Current research orientation is towards the improvement of the multispeciality medical team to treat the disorders with which these children are born.
Conclusion(s)
Children born with BWS normally have heights according to their parent’s heights and do well. Though have more chances of childhood cancer, most of them do not develop cancer and majority who develop cancer have successful treatment. Children with BWS usually have no significant delays when compared with the siblings. However, speech problems seen in some could be associated with large tongue or auditory loss. Better treatment modalities have significantly reduced the infant mortality rate linked to BWS.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 01, 2020
Manual Googling: Nov 27, 2020
iThenticate Software: Dec 28, 2020 (23%)
[1]. Jones KL, Early overgrowth with associated defects. IN; Jones KL, editorSmith’s Recognizable Patterns of Human Malformation 2006 6th edPhiladelphiaElsevier Saunders:174-75. [Google Scholar]
[2]. Frasier SD, Tall stature and excessive growth syndromes. In: FimaLifshitz, editorPaediatric Endocrinology 2003 4th edNew YorkMarcel Dekker Inc:140 [Google Scholar]
[3]. Cohen MM, Beckwith-Weidemann syndrome- Historical, clinicopathological and etiopathogenesis perspectivesPediatr Dev Path 1999 8:287-304.10.1007/s10024-005-1154-916010495 [Google Scholar] [CrossRef] [PubMed]
[4]. Pinchas C, Melanie S, Hyperpituitarism, tall stature and overgrowth syndromes. In Behrman RE, Kliegman RM, Jenson HB, Stanton BF, editorsNelson Textbook of Paediatrics 2007 18th edPhiladelphiaElsevier Saunders:2303-07. [Google Scholar]
[5]. Elliott M, Bayly R, Cole T, Temple IK, Maher ER, Clinical features and natural history of Beckwith-Wiedemann syndrome: Presentation of 74 new casesClinical Genetics 1994 46(2):168-74.10.1111/j.1399-0004.1994.tb04219.x7820926 [Google Scholar] [CrossRef] [PubMed]
[6]. DeBaun MR, Tucker MA, Risk of cancer during the first four years of life in children from the Beckwith Wiedemann Syndrome RegistryThe Journal of Pediatrics 1998 132(3 pt1):398-400.10.1016/S0022-3476(98)70008-3 [Google Scholar] [CrossRef]
[7]. Weidemann HR, Tumours and hemihypertrophy associated with Wiedemann-Beckwith syndromeEur J Pediatr 1983 141:12910.1007/BF00496807 [Google Scholar] [CrossRef]
[8]. Mohan KR, Simalti AK, Kanitkar M, Cases of Beckwith-Wiedman SyndromeMed J Armed Forces India 2009 65(2):182-83.Epub 2011 Jul 2110.1016/S0377-1237(09)80142-1 [Google Scholar] [CrossRef]
[9]. Shuman C, Beckwith JB, Weksberg R, Beckwith-Wiedemann Syndrome. 2000 Mar 3 [updated 2016 Aug 11]. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K, Amemiya A, editorsGeneReviews® [Internet] 1993-2020 Seattle (WA)University of Washington, SeattlePMID: 20301568 [Google Scholar]
[10]. Maher ER, Brueton LA SC, Beckwith Wiedemann syndrome and assisted reproductive technologyJournal of Medical Genetics 2003 40:62-64.10.1136/jmg.40.1.6212525545 [Google Scholar] [CrossRef] [PubMed]
[11]. Chang AS, Moley KH, Wrangler M, Feinberg AP, Debaun MR, Association between Beckwith Wiedemann syndrome and assisted reproductive technology: A case series of 19 patientsFertility and Sterility 2005 83(2):349-54.10.1016/j.fertnstert.2004.07.96415705373 [Google Scholar] [CrossRef] [PubMed]
[12]. Choyke PL, Siegel MJ, Craft AW, Green DM, Debaun MR, Screening for Wilms tumour in children with Beckwith Wiedemann Syndrome or idiopathic hemihypertrophyMedical and Paediatric Oncology 1999 32(3):196-200.10.1002/(SICI)1096-911X(199903)32:3<196::AID-MPO6>3.0.CO;2-9 [Google Scholar] [CrossRef]
[13]. Reish O, Lerer I, Amiel A, Heyman E, Herman A, Dolfin T, Wiedemann- Beckwith syndrome: Further prenatal characterisation of the conditionAm J Med Genet 2002 107(3):209-13.10.1002/ajmg.1014311807901 [Google Scholar] [CrossRef] [PubMed]
[14]. Halliday J, Oke K, Breheny S, Algar E, Amor DJ, Beckwith-Wiedemann syndrome and IVF: A Case control studyAmerican Journal of Human Genetics 2004 75(3):526-28.10.1086/42390215284956 [Google Scholar] [CrossRef] [PubMed]
[15]. Gosden R, Trasler J, Lucifero D, Faddy M, Rare congenital disorders, imprinted genes, and assisted reproductive technologyLancet 2003 361(9373):1975-77.10.1016/S0140-6736(03)13592-1 [Google Scholar] [CrossRef]