Chronic periodontitis is defined as an inflammatory disease that affects the supporting tissues of the teeth. Specific bacteria within the plaque biofilm initiate chronic periodontitis. It progresses due to an abnormal inflammatory-immune response and releases excess proteolytic enzymes and reactive oxygen species [1]. Inflammation is a natural defense mechanism against pathogens, and it is associated with many pathogenic diseases [2]. Many chronic diseases linked with higher production of Reactive Oxygen Species (ROS) result in oxidative stress and variety of protein oxidations [3]. In periodontitis, there is an over production of reactive oxygen species which cannot be balanced by the antioxidant defense system and this leads to tissue damage [4]. Several researches are being done by measuring the biomarkers as a reflection of patient health status or intervention outcomes [5-8]. Although blood is considered as the gold standard body fluid for evaluation of systemic processes, saliva samples are less invasive and more convenient [9]. The wide range of molecules in serum and saliva aids in providing useful data for diagnosis and treatment procedures [10].
Sialic acid contains nine carbon acidic monosaccharides and attached to the surface of soluble proteins and cells [11]. Sialic acid encompassed in the cell surface of the pathogen aids them to abstain the innate immune response of the host [12]. An upsurge in the levels of sialic acid is considered as a garrison against elevated oxidative stress in inflammatory diseases. Hence, when sialic acid in saliva and serum exhilarates it may have a vigilant role in periodontitis [13].
Nitric oxide has a short half-life and is produced by a group of isoenzymes known as Nitric Oxide Synthases (NOS) [14]. The NOS exist as three distinct isoforms, which are endothelial NOS (eNOS), neural NOS (nNOS) and inducible NOS (iNOS). Pro-inflammatory stimuli results in the expression of iNOS which produces enormous amount of NO for sustained time periods [15]. Tissue injury in inflammation involves the induction of iNOS by certain cytokines or endotoxins, which leads to the production of large quantities of NO [16]. A previous study found that in periodontal lesions, the polymorphonuclear leukocytes and macrophages via iNOS pathways resulted in an increased NO production [17].
The beneficial effect of nonsurgical periodontal therapy on some key local markers, systemic oxidative stress markers and systemic inflammatory markers independently has been reported in previous studies [18-21].
Therefore, the aim of this study was to estimate and compare the serum and salivary concentration of sialic acid and nitric oxide in patients with generalised chronic periodontitis at baseline and 90 days after nonsurgical periodontal therapy.
Materials and Methods
This study was a case-control as well as an interventional study. The subjects for this study were recruited from the out-patient department of Periodontology, Meenakshi Ammal Dental College and Hospital, Chennai and it was conducted from April 2017 to October 2018. The power of the study with 100 subjects was calculated to be 95% using the sampling software: G POWER Version 3.1.9.2. Study participants were selected based on the inclusion and exclusion criteria. The study was approved by the “Institutional Review Board”, MAHER-Deemed to be University, Chennai (MADC/IRB/2017/223).
Inclusion criteria: Inclusion criteria were subjects within the age group of 30 to 60 years. Controls were subjects with clinically healthy periodontium with probing depth less than or equal to 3 mm with no evident attachment loss. Test group included subjects having generalised chronic periodontitis with greater than 30% sites involved and clinical attachment loss greater than or equal to 3 mm. The patients were categorised as chronic periodontitis cases according to the AAP 1999 classification [22]. Subjects with greater than or equal to 10 natural teeth excluding third molars were selected.
Exclusion criteria: Exclusion criteria included subjects who had systemic disorders such as nutritional deficiencies, endocrine, haematologic, immunodeficiency and cardiovascular disorders, those who had undergone long term steroid or antibiotic therapy and those who had received periodontal treatment in the past six months. Subjects with history of smoking, tobacco chewing, alcohol consumption and also pregnant or lactating women were excluded.
The control group included 50 periodontally and systemically healthy volunteers and the test group included 50 generalised chronic periodontitis subjects. The periodontal parameters and collection of blood and saliva was done at baseline for both control and the test groups. An intervention of nonsurgical periodontal therapy which included full mouth scaling, root planing and oral hygiene instructions was performed only for the test group. The oral hygiene instructions included recommendation of brushing the teeth twice daily, cleaning between the teeth using interdental cleaning aids, advising to have a healthy diet that limits sugary beverages and snacks and to visit dentist regularly for prevention and treatment of oral diseases. Appropriate brushing techniques were taught.
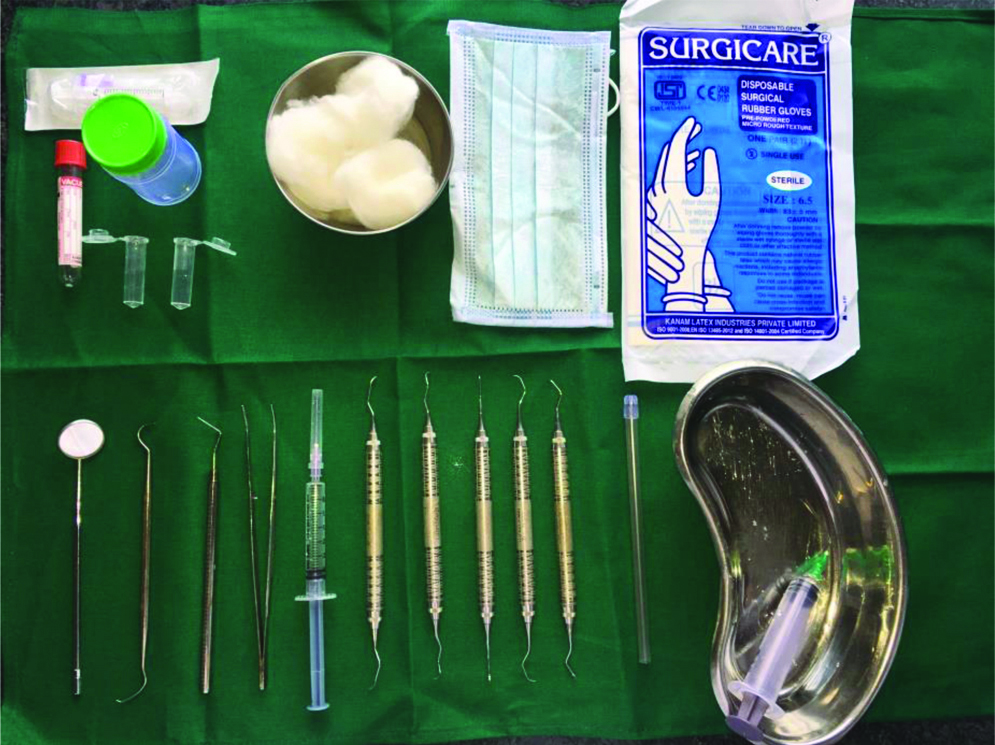
The SRP was completed in three visits. During the first visit full mouth scaling was done followed by subgingival scaling and root planing using Gracey curettes during the next two visits. At 90 days after completion of nonsurgical periodontal therapy recording of the periodontal parameters and collection of blood and saliva was done. [Table/Fig-1] shows the armamentarium used for nonsurgical periodontal therapy.
Armamentarium used for nonsurgical periodontal therapy and serum and saliva sample collection.
Periodontal Examination
Periodontal parameters such as plaque index (Silness and Loe, 1964) [23], probing pocket depth and CAL were assessed for both groups. Plaque index was measured at four sites around each tooth after air drying and the average scores were obtained. Probing pocket depth and CAL was measured using Williams periodontal probe. Probing pocket depth was measured at six sites (mesio-buccal, midbuccal, disto-buccal, mesio-lingual, mid-lingual and disto- lingual). The probe was inserted parallel to the long axis of the tooth from the gingival margin to the base of the pocket and the probing pocket depth was measured to the nearest millimetre at the gingival margin. The pocket depth for the deepest probing site was recorded for each individual tooth. The CALs in all the individual tooth were also recorded.
Blood Sample Collection
A 5 mL of venous blood from median cubital vein situated over cubital fossa was collected from each participant using non anti-coagulated blood tube. After one hour clotting at room temperature, serum was separated from blood by centrifuging at 3500 rpm for 15 minutes at 4oC. Then, the serum was immediately transferred to Eppendorf tube and stored at -70°C until the time of assay.
Saliva Sample Collection
Unstimulated 5 mL whole saliva sample was collected in the morning, two hours after the last meal according to the circadian rhythm. The subjects were asked to rinse thoroughly with distilled water, were advised to refrain from talking and asked to drop down the head and not to cough up mucus. A plastic container was given to the subjects and they were asked to expectorate into it after letting maximum saliva to pool in the floor of their mouth. The saliva samples were transported to the laboratory for estimation within 24 hours using standard gel coolant pack in order to maintain the temperature between 2oC to 4oC.
Serum and Salivary Sialic Acid and Nitric Oxide Analysis
Serum and salivary sialic acid levels were detected for each patient by combined modification of the thiobarbituric acid method of Aminoff and the method of Skoza L and Mohos S [24,25]. Serum and salivary nitric oxide levels were determined using Griess reaction [26].
a) Combined Modification of the Thiobarbituric Acid Method of Aminoff [24] and the Method of Skoza L and Mohos S [25].
The reagents used in this procedure were periodate, thiobarbituric acid and sodium arsenite. In an eppendorf tube 100 μL of the sample was taken to which 70 μL of periodate reagent was added. It was then mixed by pulse-vortexing for 15 seconds. The mixture was incubated at 37°C for 30 minutes. The reaction was terminated by the addition of 70 μL sodium arsenite and then 140 μL of thiobarbituric acid was added and vortexed. The mixture was heated in a boiling water bath for eight minutes. The sample was then cooled to room temperature and transferred from the eppendorf tube to the 96 well ELISA plate. Finally, 560 μL of Dimethyl Sulphoxide (DMSO) was added to the solution and it was measured using ELISA plate reader at 549 nm.
b) Griess reaction [26]
In an eppendorf tube, 250 μL of the sample and 250 μL of griess reagent were added and vortexed. The mixture was then transferred to a 96 well ELISA plate. To obtain standard curves sodium nitrite in distilled water at concentration of 10, 20, 30, 40, 50 μL were also included. It was incubated at room temperature for 15 minutes. This produced a purple azo-dye as an end product. The optical density was measured using an ELISA plate reader at 570 nm.
The patients were explained about the study and written informed consent was obtained from those who agreed to participate in this study.
Statistical Analysis
The collected data were analysed with IBM Statistical Package for the Social Sciences (SPSS) software Version 23.0. Descriptive statistics was used through mean and standard deviation. The tests of normality with Shapiro-Wilk and Kolmogorov-Smirnov tests were done which revealed that all variables follow normal distribution. The mean values between groups were compared using Independent t-test. Paired t-test was applied to compare mean values between two time points. Karl Pearson correlation coefficients were calculated to assess the linear relationship between variables. The probability value 0.05 was considered as significant level.
Results
The mean age for the control group was 45.74±8.51 years and that for the test group was 43.98±7.88 years. The mean plaque index, probing pocket depth and CAL in control and test group were 0.578±0.091 and 2.63±0.087; 1.76±0.190 mm and 6.78±0.313 mm; 1.76±0.190 mm and 7.33±0.445 mm and the differences were statistically significant at baseline between the test and control groups p<0.001. The mean differences being -2.05 for plaque index, -5.01 mm for probing pocket depth, -5.56 mm for CAL [Table/Fig-2].
Baseline values-comparison of mean values at baseline between the test and control groups.
| Variables | Group | N | Mean | Std. Dev | p-value |
|---|
| Age (in years) | Control | 50 | 45.74 | 8.516 | 0.286 |
| Test | 50 | 43.98 | 7.883 |
| 100 | 44.86 | |
| Plaque index | Control | 50 | 0.57760 | 0.090566 | p<0.001** |
| Test | 50 | 2.630 | 0.087575 |
| 100 | 1.603 | |
| Probing depth | Control | 50 | 1.769 | 0.190298 | p<0.001** |
| Test | 50 | 6.788 | 0.313064 |
| 100 | 4.278 | |
| Clinical attachment level | Control | 50 | 1.769 | 0.190298 | p<0.001** |
| Test | 50 | 7.335 | 0.444497 |
| 100 | 4.552 | |
| Serum sialic acid | Control | 50 | 16.709 | 3.017619 | p<0.001** |
| Test | 50 | 29.224 | 3.174429 |
| 100 | 22.967 | |
| Salivary sialic acid | Control | 50 | 13.968 | 2.260782 | p<0.001** |
| Test | 50 | 25.938 | 4.262847 |
| 100 | 19.9537 | |
| Serum nitric oxide | Control | 50 | 209.185 | 22.883481 | p<0.001** |
| Test | 50 | 338.947 | 32.349382 |
| 100 | 274.066 | |
| Salivary nitric oxide | Control | 50 | 171.681 | 12.025433 | p<0.001** |
| Test | 50 | 250.659 | 22.832417 |
| 100 | 211.170 | |
Test applied: Independent samples t-test; *statistically significant; **statistically highly significant
Similarly, the Serum sialic acid and nitric acid and Salivary sialic acid and nitric acid were levels statistically significant at baseline between the test and control groups p<0.001. The mean differences were -12.515 mg/dL for Serum sialic acid,-11.97 mg/dL for salivary sialic acid, -129.762 μMol/L for serum nitric acid and -78.978 μMol/L for salivary nitric acid, respectively.
[Table/Fig-3] showed that the mean plaque index, probing pocket depth and Clinical Attachment Level (CAL) for the test group at baseline and 90 days after nonsurgical periodontal therapy was 2.63±0.088 and 1.29±0.105; 6.78±0.313 mm and 3.63±0.279 mm; 7.33±0.445 mm and 4.05±0.342 mm, respectively. The mean differences were 1.33; 3.15 mm and 3.28 mm, respectively all with p-value <0.001, which was statistically significant.
Intragroup observations in test group at baseline and 90 post SRP.
| Parameters | Pre-treatment/Baseline Mean±SD | Post-treatment/90 days after nonsurgical periodontal therapy Mean±SD | Mean difference | p-value |
|---|
| Plaque index | 2.63±0.088 | 1.29±0.105 | 1.33 | p<0.001** |
| Probing pocket depth (mm) | 6.78±0.313 | 3.63±0.279 | 3.15 | p<0.001** |
| Clinical attachment level (mm) | 7.33±0.445 | 4.05±0.342 | 3.28 | p<0.001** |
| Serum sialic acid (mg/dL) | 29.22±3.74 | 15.01±2.472 | 14.20 | p<0.001** |
| Salivary sialic acid (mg/dL) | 25.93±4.263 | 13.17±2.225 | 12.76 | p<0.001** |
| Serum nitric oxide (μmol/L) | 338.94±32.349 | 208.86±20.551 | 130.082 | p<0.001** |
| Salivary nitric oxide (μmol/L) | 250.66±22.832 | 168. 65±11.251 | 82.004 | p<0.001** |
Tests applied: Paired samples t-test to compare mean values between baseline and 90 days post SRP for test group; *statistically significant; **statistically highly significant
The mean serum and salivary sialic acid in test group at baseline and 90 days after nonsurgical periodontal therapy was 29.225±3.174 mg/dL and 15.01±2.472 mg/dL; 25.939±4.263 md/dL and 13.179±2.225 mg/dL, respectively. On comparison, the mean difference was 14.20 mg/dL and 12.76 mg/dL with p-value <0.001 which was statistically significant. The mean serum and salivary nitric oxide in test group at baseline and 90 days after nonsurgical periodontal therapy was 338.947±32.349 μMol/L and 208.865±20.551 μMol/L; 250.66±22.832 μMol/L and 168.655±11.251 μMol/L respectively. The mean difference was 130.082 μMol/L and 82.004 μMol/L with p-value <0.001, which was statistically significant.
The overall correlation between plaque index and serum and salivary sialic acid and nitric oxide in control and test group had r-values 0.889, 0.866, 0.919 and 0.912, respectively. The overall correlation between probing pocket depth and serum and salivary sialic acid and nitric oxide in control and test group had r-values 0.902, 0.862, 0.919, 0.895, respectively. The overall correlation between CAL and serum and salivary sialic acid and nitric oxide in control and test group had r-values 0.903, 0.866, 0.917, 0.896 respectively. All the r-values suggested a statistically significant positive correlation with p<0.001 [Table/Fig-4].
Overall correlation between plaque index, probing depth, clinical attachment level and serum and salivary sialic acid and nitric oxide in control and test group.
| Parameters | Plaque index | Probing depth | Clinical attachment level |
|---|
| Serum sialic acid | Correlation coefficient | 0.889 | 0.902 | 0.903 |
| p-value | p<0.001** | p<0.001** | p<0.001** |
| N | 100 | 100 | 100 |
| Salivary sialic acid | Correlation coefficient | 0.866 | 0.862 | 0.866 |
| p-value | p<0.001** | p<0.001** | p<0.001** |
| N | 100 | 100 | 100 |
| Serum nitric oxide | Correlation coefficient | 0.919 | 0.919 | 0.917 |
| p-value | p<0.001** | p<0.001** | p<0.001** |
| N | 100 | 100 | 100 |
| Salivary nitric oxide | Correlation coefficient | 0.912 | 0.895 | 0.896 |
| p-value | p<0.001** | p<0.001** | p<0.001** |
| N | 100 | 100 | 100 |
Test applied: Pearson correlation; *statistically significant; **statistically highly significant
Discussion
In the present study, we ventured to establish, evaluate and compare the role of serum and salivary sialic acid and nitric oxide as biomarkers in periodontitis. The mean differences for plaque index, probing pocket depth and CAL were higher in the test group than in the control group at baseline p<0.001, which were statistically highly significant.
On comparing the test group at baseline and 90 days after nonsurgical periodontal therapy, there was a significant reduction in plaque index and probing pocket depth with a significant gain in the CAL. The mean differences were statistically highly significant, p<0.001.
The current criteria for assessment of periodontal tissues surrounding teeth are based on diagnostic measures, such as periodontal pocket depth, CAL, plaque index, bleeding on probing and radiographic assessment of alveolar bone loss [27]. Passive filtration allows certain hormones, cytokines, metabolites and signal molecules to move into the saliva and this reflects the plasma levels [28]. The presence of several periodontal and other systemic disease markers in the saliva and serum became a topic of extensive research due to the development of nanotechnology and hence even smaller magnitudes of various biomarkers could be identified [28]. Analytical chips available also identify several molecules in a much effortless way [28].
The serum and salivary sialic acid levels were higher in the test group when compared to the control group at baseline with p-value <0.001, which was statistically highly significant again. These results are in accordance with the study conducted by Inasu S et al., who concluded that the serum and salivary sialic acid levels were increased in chronic periodontitis patients than the control group with df 24.375 and 38 respectively and the p-value were <0.001 and 0.622, respectively [29]. In a study done by Rathode S et al., it was concluded that the salivary sialic acid levels in periodontitis group was 1.70±0.46, whereas that in the healthy group was 0.77±0.34 and the p-value was <0.001 [30]. Specific antigen is included in a bacterium with virulence factor and this triggers the release of cytokines from the monocytes which is regulated with sialic acid and this attributes to the increase in serum sialic acid [31]. Jawzaly I et al., in their study demonstrated that the salivary sialic acid in periodontitis group was 156.84±3.9 and that in control group was 96.80±0.32 with p-value <0.01 [32]. They concluded that sialic acid can be used as a biomarker in dentate periodontitis. Oktay S et al., in their study inferred that the serum sialic acid in control group was 60.03±10.62, in chronic gingivitis group it was 80.69±9.09 and that in chronic periodontitis group was 108.65±17.71 [33]. The p-value was <0.001 and it was statistically significant. Elevated levels of sialic acid in saliva and serum may have a protective role in periodontitis and it was considered as a defense molecule against the increased oxidative stress in inflammatory diseases including periodontitis [30].
Intra group comparison revealed that there was a significant reduction in the levels of serum and salivary nitric oxide, 90 days after nonsurgical periodontal therapy. The mean differences being 130.082 and 82.004, respectively, with p<0.001, which was statistically highly significant. The results of this study were in accordance with the study done by Wattamwar PP et al., who assessed serum and saliva samples in patients with chronic periodontitis at baseline and 6 weeks after phase I therapy [34]. The results showed that the mean difference in serum nitric oxide was 6.35±2.36 and that in salivary nitric oxide was 8.72±2.20 with p-value <0.001 which was statistically significant. Parwani SR et al., conducted a similar study where they estimated the salivary nitric oxide levels in gingivitis and periodontitis patients [35]. The nitric oxide levels in gingivitis patients were 430.60±67.97 and that in patients with periodontitis were 537.67±80.06 with the p-value <0.001 which was highly significant.
Increased plaque deposition in chronic periodontitis subjects might activate the inducible NO synthase (iNOS) promoting the conversion of L-arginine into NO and its compounds [36]. Chae HJ et al., related that the presence of nitric oxide is increased in alveolar bone resorption [37] whilst others reported that this molecule may have an effect on the growth and survival of the bacteria implicated in periodontal disease {Kroncke KD et al., (1997) and Allaker RP et al., (2001)} [38,39]. In contradiction to these studies it may also function as a mediator for the control of clastic activity and thereby avoid excessive bone resorption (Stadler J et al., 1993) [40].
Limitation(s)
During the study period, changes in the serum and salivary levels of sialic acid and nitric oxide associated with generic factors such as stress, diet, lifestyle, hygiene or exercise, were assumed to be equivalent between the test and control groups, which was a limitation of the study. Further prospective clinical trials should be conducted to confirm our findings, as well as to better understand the mechanisms by which sialic acid and nitric oxide can modulate periodontal disease.
Conclusion(s)
Within the limitations of this study, it can be inferred that chronic periodontitis could influence the levels of serum and salivary sialic acid and nitric oxide. To conclude, nonsurgical periodontal therapy led to a decrease in the serum and salivary sialic acid and nitric oxide levels in subjects with generalised chronic periodontitis. The results of the current study suggest that serum and salivary sialic acid and nitric oxide hold promise as reliable biochemical markers of the extent of tissue destruction in periodontitis. They encourage us in hoping that these biochemical markers may be used in diagnosis, treatment and prognosis of the periodontal disease.
Test applied: Independent samples t-test; *statistically significant; **statistically highly significant
Tests applied: Paired samples t-test to compare mean values between baseline and 90 days post SRP for test group; *statistically significant; **statistically highly significant
Test applied: Pearson correlation; *statistically significant; **statistically highly significant