Ménière’s Disease (MD) is associated with episodic attacks of vertigo, progressive hearing loss and tinnitus, aural fullness, along with vegetative symptoms and gait problems as well as instability [1]. Tinnitus and/or aural fullness must be in attendance be with the affected ear [2]. Symptoms vary between population and time and is mentioned to be a progressive disease presentable by three stages. Regarding the pathophysiology of MD, the hypothesis is rooted on the endolymphatic hydrops for pathological basis of it, where endolymph may be either excessively synthesised or inadequately resorbed, causing expansion of the endolymphatic space [3-6]. Effects on postural control during the change of endolymphatic hydrops could be related to the pressure increase in the labyrinth [7]. Therefore, a more permanent damage to the inner ear balance organ and significant general balance problems are common, especially in the dark.
Conservative symptomatic treatment of vertigo attacks, along with prophylactic treatment and salt-restricted diet as well as caffeine intake decrease are the fundamental parts in MD management. Patients who have vertigo that is not controlled with conservative treatment, are recommended to undergo advanced treatment options [8,9]. Steroid treatment is used for the management of either hearing loss or vertigo, and intratympanic steroid treatment (ITS) could be defined as an initial surgical procedure without systemic adverse effects while cochlear and vestibular functions are not damaged [10]. Some studies reported encouraging results in the control of vertigo attacks, however, the effects on the vestibular system were not objectively registered [11,12]. For this reason, this study was focused on the evaluation of effects of ITS treatment on postural control based on ultrasound-computer-craniocorpography (US-COMP-CCG), which can objectively register the result of standing (Romberg’s) and stepping (Unterberger-Fukuda’s) tests; ultrasound was used to register the movements during both examinations [13].
Materials and Methods
This retrospective case-control study, conducted at Semmelweis University, Department of Otolaryngology and Head and Neck Surgery during the period of January 2018 to March 2020, involved 120 patients data suffering from advanced MD. In the studied group, (group 1) 38 patients were treated with ITS and (group 2) 82 subjects were enrolled as control, to achieve an appropriate number of control subjects for a case-controlled study. The sampling was based on the participants receiving the treatment and categorised into advanced MD, whereas the control group was determined as the double sum of that population. The study was approved by the Regional and Institutional Committee of Science and Research Ethics at Semmelweis University (47/2018).
Inclusion and Exclusion criteria: All patients enrolled in the sample fulfilled the diagnostic criteria for MD [2]. Patients data with probable MD, motion sickness and vestibular migraine were excluded from the study. Bilateral MD with or without autoimmune disease was also excluded. Patient and their data selection was made based on the clinical staging criteria of MD and on the objective staging measurements of US-COMP-CCG (stage I: rare attacks, II: severe and recurring attacks, III: severe constant hearing loss, disabling balance problems, severe attacks) [6,13]. More specifically, patients suffering from stage III were selected and therefore, the administration of ITS (dexamethasone) injection was decided. By this means the gait system could be measured before and after administration. As per the hospital protocol, the test was firstly performed before the first ITS administrated treatment and re-measured two weeks after the last treatment. Determination for an abnormal postural control was based on the standing and stepping test parameters of US-COMP-CCG. Categorisation for abnormal was based on changes in any two out of four parameters for each test.
Intratympanic Steroid Injection Protocol (ITS)
Patients suffering from stage III (advanced) MD were treated with ITS. The usual procedure for intratympanic drug delivery into the inner ear was applied in the hospital as follows:
The patient was held stationary with the treated ear facing toward the ceiling. After confirming intact ear status, lidocaine 10% pump spray is administered for local anaesthesia on the tympanic membrane for approximately five minutes. While the patient tilts the head 45° to the healthy side, a 25-gauge spinal needle was introduced into the anteroinferior portion of the membrane, and 5 mg/mL of dexamethasone was instilled through this site. The patient was instructed to avoid swallowing or moving for 30 minutes, remaining in the same position to facilitate passage of the steroid to the round window membrane. ITS therapy with dexamethasone was determined to be performed up to five total injections, one every day. The decision of number of treatment administration was based on the institution clinical protocol of MD treatment [14].
Ultrasound-Computer-Craniocorpography (US-COMP-CCG)
US-COMP-CCG uses ultrasound markers on head and shoulder, and the numerical data of vestibulospinal tests are measured and analysed by the computer [15]. This is based on a mathematical analysis, and the principle is installed into the ZEBRIS Coordinate Measurement System® (Isny, Germany). The system registers two vestibular tests based on the vestibulospinal reflex: the standing (Romberg’s) and stepping (Unterberger-Fukuda’s) test. The main parameters for evaluating the standing test are the longitudinal and lateral sway in cm, forehead covering area in cm2 and the torticollis angle in degree. The main parameters for evaluating the stepping test are the longitudinal deviation and lateral sway width in cm, the angular deviation and the self-spin in degree. In the standing test, the patient was asked to stand still with their feet together, hands extended out, and eyes closed for a period of roughly one minute. The stepping test was found upon a series of steps on the spot during a period of one minute.
Statistical Analysis
Statistical analysis was performed by using the IBM SPSS V24 software. Because the studied parameters did not show normal distribution, the Mann-Whitney U test was used. For the illustration of the results the Kaplan-Meier curve was included, and a Logistic Regression was used. To analyse the baseline characteristic of the control and treated groups, Mann-Whitney U test and Chi-square test were applied. Boxplots were also included because that is a standardised way of displaying the distribution of the data. The significance level was specified as p<0.05.
Results
Based on the baseline parameters the two groups were appropriate to compare, because there was no statistically significant difference detected between the parameters of the two groups [Table/Fig-1].
Baseline parameters for the two groups (group 1: treated with ITS, group 2: control group). For all US-COMP-CCG parameters mean±SD values were included.
| Parameters | Group 1 | Group 2 | p-value |
|---|
| Gender (male/female) | 16/22 | 33/49 | 0.85a |
| Age (mean±SD) (years) | 55.62±9.46 | 52.08±12.25 | 0.99b |
| Side of MD (right/left) | 22/14 | 43/39 | 0.38a |
| Longitudinal sway (cm) | 8.44±3.32 | 9.62±4.42 | 0.53b |
| Lateral sway (cm) | 6.24±2.62 | 6.17±3.33 | 0.57b |
| Forehead covering area (cm2) | 60.40±47.00 | 104.72±124.73 | 0.28b |
| Torticollis angle (degree) | 8.75±4.60 | 10.14±5.53 | 0.87b |
| Longitudinal deviation (cm) | 63.85±24.22 | 66.63±20.88 | 0.23b |
| Lateral sway width (cm) | 16.35±5.46 | 14.78±4.11 | 0.24b |
| Angular deviation (degree) | 159.81±20.42 | 156.90±20.04 | 0.33b |
| Self-spin (degree) | 41.70±31.30 | 56.94±42.68 | 0.38b |
a: Chi-square test, b: Mann-Whitney U test
All MD patients showed a moderate to severe hearing loss, prolonged and frequent vertigo attacks and instability. Changes in at least two parameters in the standing test were observed in 6/38 patients and in the stepping test, changes were observed in 13/38 patients.
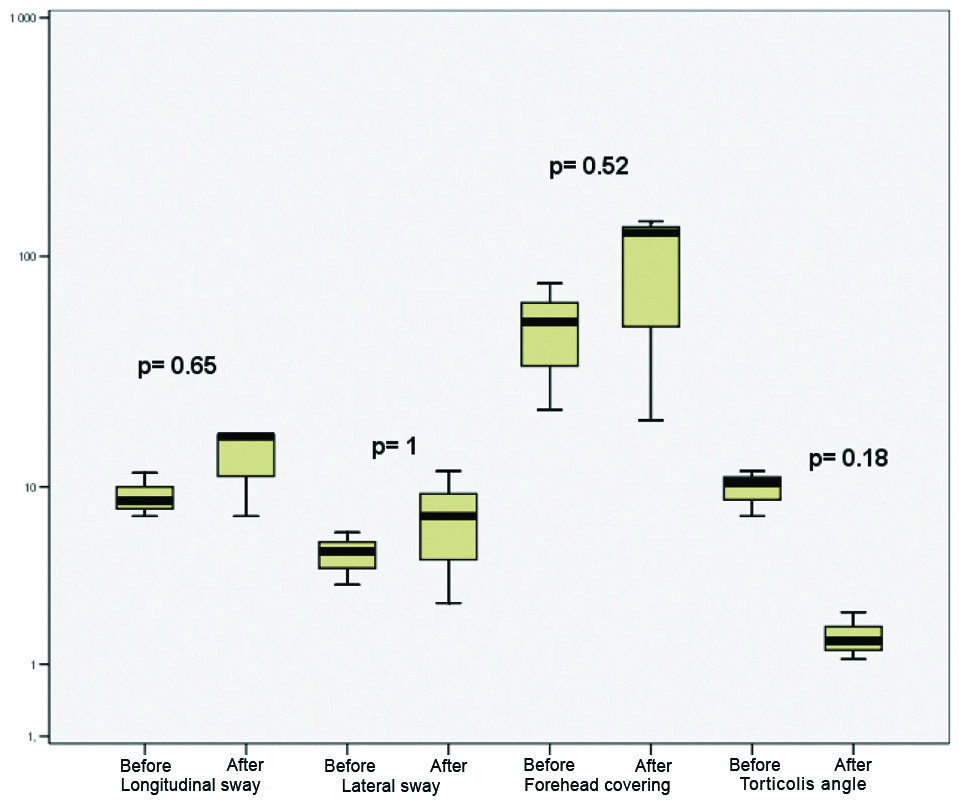
As shown in [Table/Fig-2], based on the boxes, there was no obvious difference between the parameters before and after treatment, and the p-values also indicate no significant difference between the pre- and post-treatment parameters. Based on the analysis, it can be stated that the ITS therapy had no significant effect on the outcome of the standing test.
Boxplot about the parameters of the standing test before and after treatment. Black line: median value, box: the middle 50% of the data, whiskers: upper and lower 25%. The p-values were determined based on the Mann-Whitney U test.
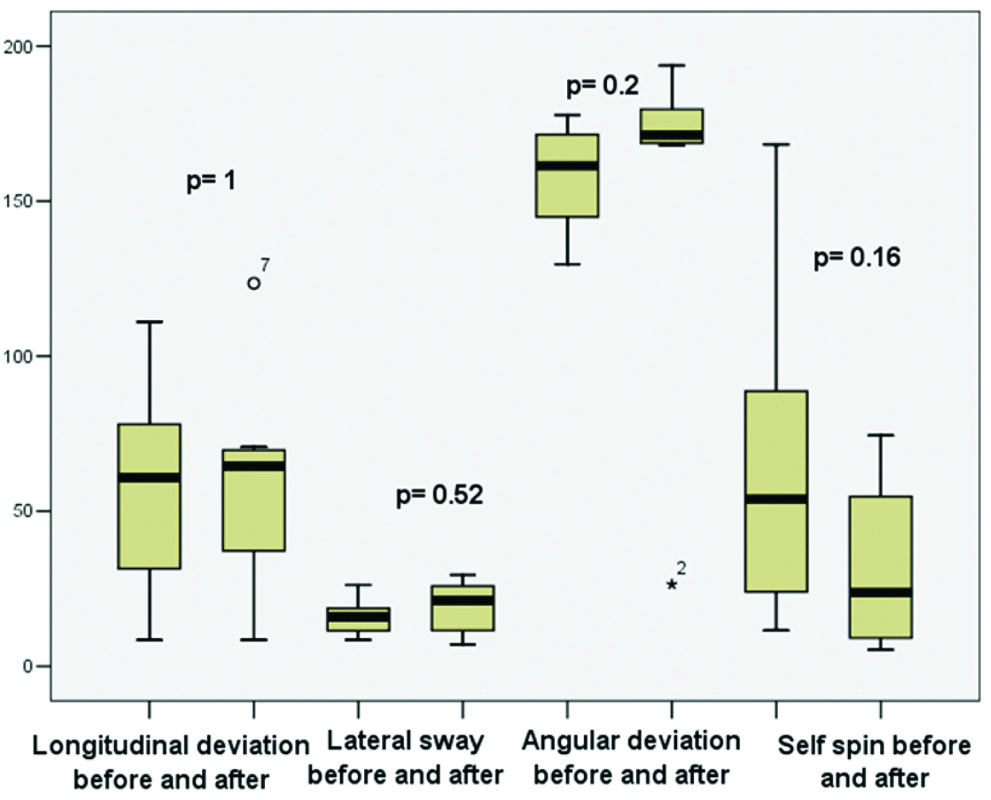
As shown in [Table/Fig-3], in case of the stepping test, no obvious difference between the boxes of pre- and post-treatment values can be detected, and the p-values also do not indicate a statistically significant difference between the parameters. Thus, ITS does not have a significant effect on the outcome of the stepping test.
Boxplot about the parameters of the stepping test before and after treatment. p-values were determined based on the Mann-Whitney U test.
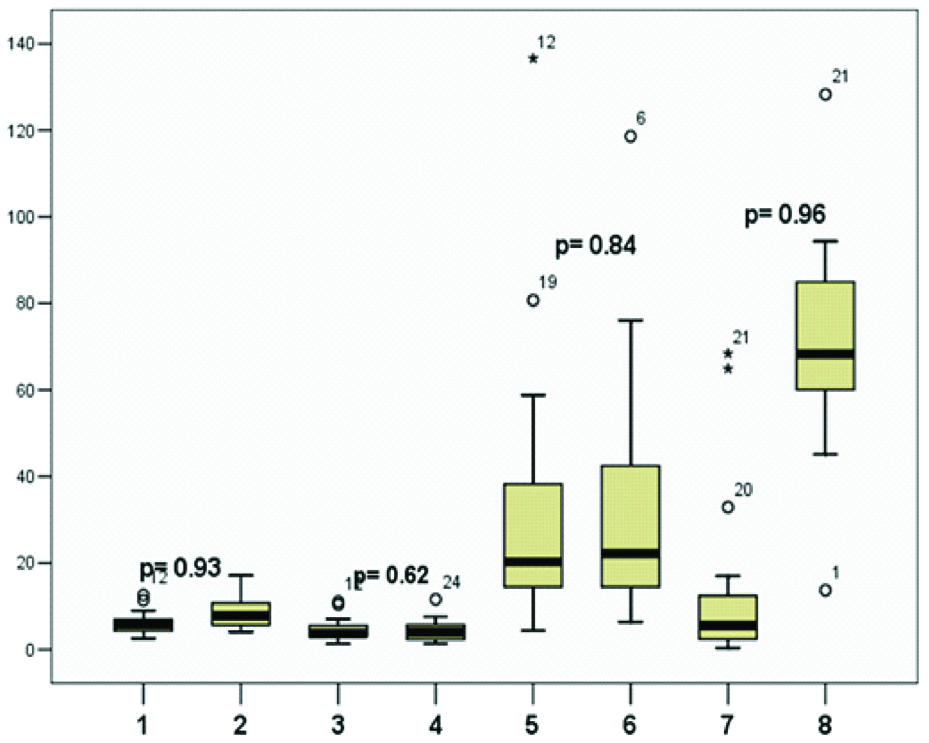
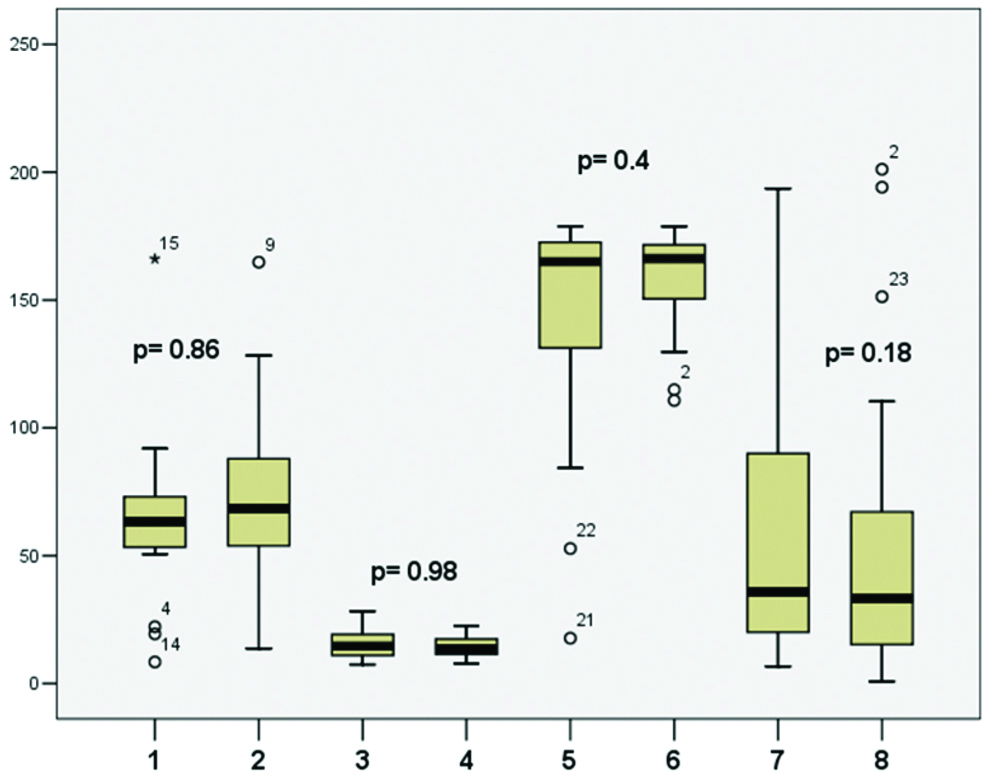
Based on the boxplot [Table/Fig-4], it can be concluded that when parameters of controls and treated MD patients were contrasted, there was no difference between the boxes in most cases, and the difference, if any, was determined not to be statistically significant. The same results came up in the stepping test, shown in [Table/Fig-5], in which the median values and the boxes of parameters did not differ, and based on the p-values no significant difference was detected.
Comparison between the parameters of the standing test of controls and patients treated with ITS. p-values were determined based on the Mann-Whitney U test. 1: Longitudinal sway of treated patients, 2: control, 3: Lateral sway of treated patients, 4: control, 5: Forehead covering area of treated patients, 6: control, 7: Torticollis angle of treated patients, 8: control.
Comparison between the parameters of the stepping test of controls and patients treated with ITS. The p-values were determined based on the Mann-Whitney U test. 1: Longitudinal deviation of treated patients, 2: Control, 3: Lateral sway width of treated patients, 4: Control, 5: Angular deviation of treated patients, 6: Control, 7: Self spin of treated patients, 8: Control.
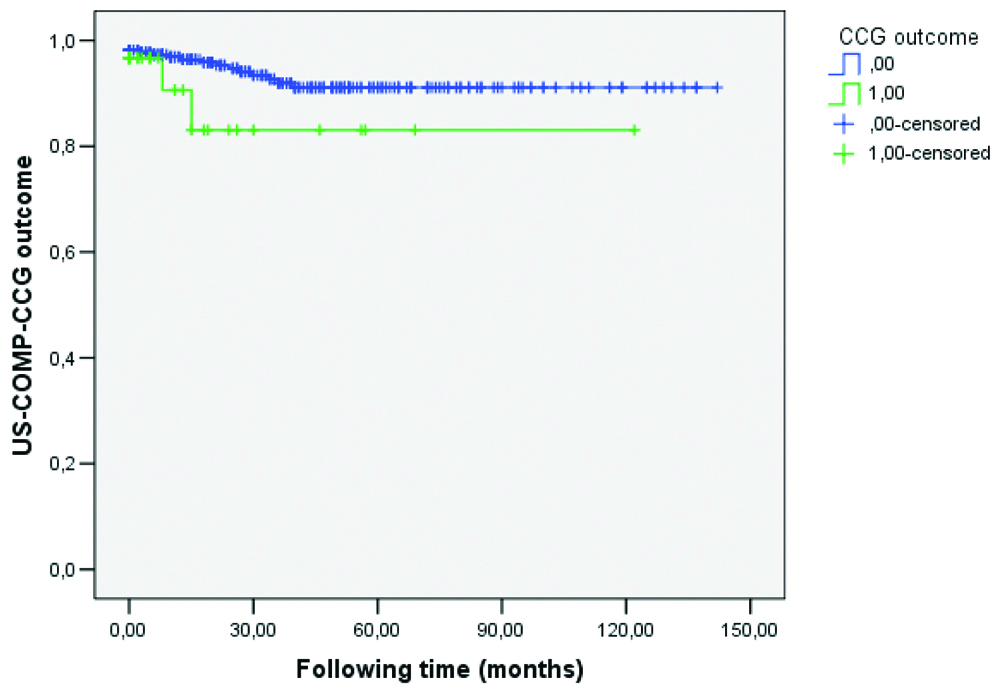
Further analysis was made based on the Kaplan-Meier curve and logistic regression test to strengthen the results and to make the long-term follow-up possible because all of the US-COMP-CGG examinations performed on each patient could be taken into consideration.
Based on the survival-ship curve shown in [Table/Fig-6], there was no visible difference between the two curves (e.g., significantly worsened outcome of US-COMP-CCG of control and patients treated with ITS), and the logistic regression also indicated {p=0.445; Odds ratio: 1.654 (95% CI: 0.166-0.197)} that there was no significant statistical difference between the results of the groups.
The occurrence of worsened US-COMP-CCG parameters before and after ITS treatment. In SPSS, the number of events (i.e., worsening in US-COMP-CCG parameters) that happened at time (following time) was determined as follows: 0, if less than 2 parameters and 1, if more than 2 parameters showed aberration. Blue: not treated, Green: treated.
Discussion
The current study suggests the effect of ITS on the balance system of advanced MD patients. Postural control impairment in MD may well be attributed to the endolymphatic changes and the effect of it to the labyrinth pressure which interferes with the normal endolymphatic dynamics. Based on the detection of labyrinth impairment according to Di Girolamo S et al., an abnormal static craniocorpography response was found in 70% of the patients examined [7]. According to the results of some previously published studies, it can be concluded that the evaluation of vestibulospinal reflex is more sensitive compared to other vestibular tests [7,16].
In a more recent study of Al Saif AA et al., the efficiency of the sideways stepping test was investigated with the conclusion that there was a strong correlation between the stepping test and head-shaking test using video electronystagmography, with high specificity and sensitivity [17]. In a previous study from the index group, in which the potential use of US-COMP-CCG in the staging of MD was investigated, it was concluded that the examination of the vestibulospinal reflex using craniocorpography is a useful method in the staging of MD [13]. Based on the two studies mentioned above, it was decided to use the US-COMP-CCG to examine the possible effects of ITS therapy on the balance system.
Steroid administration is widely used in treatment of MD, and most studies evaluated the treatment effect on the cochlear system and vertigo attacks. An improvement in symptomatic control of hearing loss and tinnitus was observed by a study of Molnár A et al., as well as Memari F et al., suggesting the beneficial nature of this treatment [8,18]. Itoh A and Sakata E first reported on the protocol for an intratympanic injection in 1987 [19]. This treatment protocol resulted in the relief of vertigo in 80% of patients and the reduction of tinnitus in 74% [7].
Based on a systemic review, the effectiveness of the ITS therapy varies from 32.1% to 70% [20], vertigo control at 48.1% [21] and 60.4% [11] at one year and 59.1% [12] or 32.1% [11] at two years was detected. Although in most of the cited studies, objective vestibular tests were not used to detect the potential effects of ITS therapy. For this reason, this study focused on the objective testing after treatment. Based on the testing performance and analysis, no significant differences were found. This may be attributed to the frequency of attacks during the examination period, as well as the presence or absence of other complaints of dizziness. Moreover, ITS treatment alleviates the vertigo spells based on the literature and therefore US-COMP-CCG was nearly always unchanged.
Limitation(s)
This was a retrospective study. First of all, MD is a fluctuating type of disorder, and a fluctuation of the symptoms could never be ruled out which is always a limitation. In the diagnosis of MD, other vestibular tests, just like the caloric test or video-head-impulse test, pure-tone audiometry were also used, but this study focused on the results of US-COMP-CCG, so the results of the other tests were not included.
Conclusion(s)
Whilst ITS treatment can improve hearing impairment, as well as it decreases the vertigo attacks occurrence, it appears to have no effect on postural control. According to our results, there are no changes detected on vestibular function based on US-COMP-CCG post administration of ITS injection. Based on the literature, the effectiveness of ITS therapy is variable, and using objective vestibular tests, no significant change was detected, so further studies are necessary to investigate the potential benefits of the therapy.
a: Chi-square test, b: Mann-Whitney U test