The Hirschsprung’s Disease (HD) is a relatively common congenital disorder found one in 5000 live births and is of unknown aetiology. It is characterised by absence of ganglion cells in the submucosa and muscularis propria of the distal colon and rectum. Developmentally, there occurs a defect in the craniocaudal migration of neuroblasts originating from neural crest during 4th to 12th week of gestation which results in functional obstruction of bowel with distal narrow aganglionic segment and consequent dilated proximal colon (megacolon). Short segment disease, also known as classical HD is the most common variant (75 to 80% of cases) and is confined to rectosigmoid region of colon. Long segment disease is relatively uncommon (10 to 20%) where aganglionosis affects more proximal part of sigmoid colon and extends above splenic flexure. In 5% of cases, the entire colon along with a portion of small bowel may be affected (Total bowel aganglionosis).
Neonates with HD usually present with features of distal intestinal obstruction like failure to pass meconium, abdominal distention, failure to establish feeds and bilious or nonbilious vomiting in the first few days of life. In some, the presentation may be delayed and the neonate or infant may present with features of enterocolitis. Some children present at a much later stage of life with chronic constipation. Though radiological imaging like barium enema gives a clue to the diagnosis, rectal biopsy remains the gold standard to establish a definitive diagnosis of HD. Histopathological examination using routine H&E staining confirms the absence of ganglion cells in the meissner’s and myenteric plexuses and the presence of hypertrophied nerve fibres in the submucosa of the aganglionic segment [1]. Calretinin IHC staining has of late is being described as a useful adjunctive technique in detecting the ganglion cells including the small immature ones and the nerve fibres. Absence of expression of calretinin stain in the submucosa and muscularis propria of the affected segment aids in confirming the diagnosis of HD. Calretinin immunoreactivity offers several advantages in the work up of HD, including its simplicity, lack of inter-observer variability, applicability of calretinin to formalin fixed paraffin embedded tissue and better appreciation of the ganglion cells and nerve fibres, particularly in inadequate biopsy samples. It prevents unnecessary surgery by detection of ganglion cells which might be missed by routine H&E staining [2-4]. Hence, this study had been carried out to assess the feasibility of Calretinin IHC as a superior diagnostic and confirmatory tool over the routine H&E studies in HD of both clinically suspected and postoperative cases.
Materials and Methods
This was a prospective study carried out in the Department of Pathology, SCB Medical College, Cuttack, India in collaboration with the Department of Paediatric Surgery, SVPPGIP, Cuttack during the period from August 2016 to July 2018. This study was approved by Institutional Ethics Committee- SCB Medical College and Hospital (IEC/ IRB 779/15.1 2019).
Inclusion criteria: The study included suspected HD patients which were in the age group of 2 days to 2 years 9 months and presented with features of failure to pass meconium within first 24 hours, acute intestinal obstruction, vomiting, abdominal distention, failure to gain weight and spontaneous intestinal perforation. The study also included postsurgical resection biopsies for further management.
Exclusion criteria: Patients unwilling to give consent and with inadequate biopsy samples were excluded from the study.
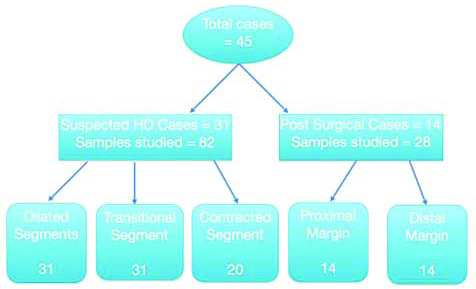
This study was conducted on 31 suspected cases of HD and 14 postoperative cases [Table/Fig-1]. Thirty-one patients with suspected HD were subjected to laparoscopic full thickness rectal biopsy including samples from contracted, transitional and dilated segment of affected parts of colon. In total, 82 formalin fixed tissue samples comprising of 31 each from dilated and transitional segments and 20 from contracted segments were processed and stained with routine haematoxylin and eosin stain. The study also included 14 patients with postsurgical resection with 28 tissue samples, one each from proximal and distal margins. A thorough search was made for the presence/absence of ganglion cells in all the sections. Biopsy sections showing presence of ganglion cells were taken as internal positive control. Subsequently, immunohistochemical staining was done using calretinin. The paraffin wax embedded, four micrometer thick sections of biopsy specimens for each patient were thaw mounted on glass slides. High temperature antigen retrieval using 0.01M citrate retrieval solution (pH 6.0) was done. IHC was carried out using a monoclonal mouse antibody (Path in situ) at a dilution of 1:100. After 30 minutes of incubation, unmasking was carried out in a pH 9 buffer heated up to 120°. Pure Envision dual ink (path in-situ) was applied for 30 minutes. Calretinin staining was analysed qualitatively depending on the granularity of the cytoplasm and nucleus; results interpreted and compared with H&E staining. Antibody was omitted from staining process for negative control.
Flow chart of sample size.
Statistical Analysis
The statistical analysis was carried out using Statistical Package for Social Sciences (SPSS Inc, Chicago IL, version 15.0 for windows). All Quantitative variables were assessed using measures of central location and measure of dispersion. One-way analysis of variance (ANOVA) was used for more than two groups. Qualitative or categorical variables were described as frequencies and proportions. Proportions were compared using the Chi-square test wherever applicable. All statistical tests were two sided and performed at a significant level of p<0.05.
Results
A total number of 45 cases were studied during a span of two years. These included 31 from clinically suspected cases of HD and 14 from post-operative (colostomy) patients. In all suspected cases, a detailed clinical history and presentation including age and sex of the patient was noted. Observations on subtypes of HD and detection of ganglionic and aganglionic segments in calretinin and H&E morphology were recorded.
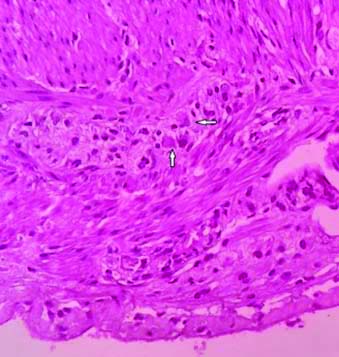
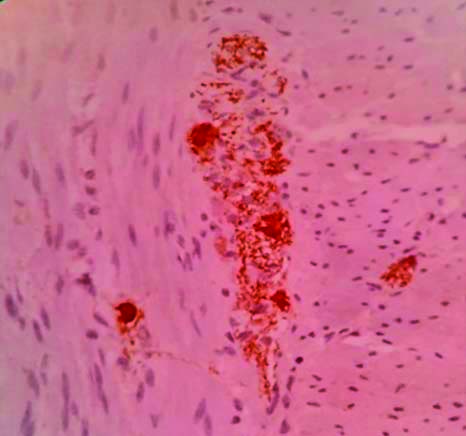
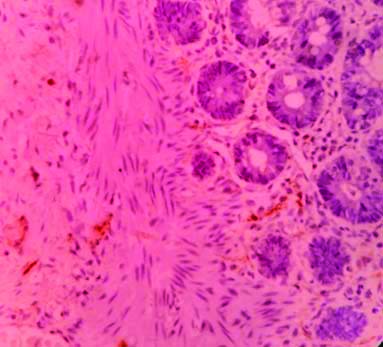
With H&E staining, the ganglion cells were round to oval cell with abundant fibrillary eosinophilic cytoplasm, round to oval nuclei having fine nuclear chromatin and prominent nucleoli [Table/Fig-2]. Calretinin IHC staining revealed intense homogeneous granular cytoplasmic and nuclear pattern of staining in the ganglion cells [Table/Fig-3]. Normal colonic mucosa was taken as control which showed presence of calretinin positive ganglion cells and nerve fibers in muscularis propria and linear nerve fibrils in lamina propria and submucosa [Table/Fig-4]. There was absence of Calretinin staining in aganglionic segments in muscularis propria [Table/Fig-5]. The age of the patients ranged from 2 days to 2 years nine months with mean age of 7.7 months (by weighted average method) and included 29 males (64.44%) and 16 females (35.56%). Most of the subjects i.e. 28 (62.2%) were of less than six months of age, which included 17 (37.7%) males and 11 (24.4%) females. The most common clinical presentation was failure to pass meconium (21 patients, 46.7%) followed by chronic constipation (12, 26.7%), abdominal distention (6, 13.3%) and failure to gain weight (3, 6.7%). Three cases presented with intestinal perforation [Table/Fig-6]. Thirty-one cases of suspected HD included 25 (80.64%) short segment subtype and 6 (19.36%) of long segment subtype. The 25 cases of short segment subtype included 20 (64.52%) males and 5 (16.13%) females and the six cases of long segment subtype included 4 (12.9%) females and 2 (6.45%) males. Short segment HD was more prevalent in males (M-80%, F-20%) and long segment HD was more common in females (M-33.3%, F-66.7%). The subtypes of HD detected from the morphological study of both the staining (H&E and Calretinin IHC) were compared.
Colonic mucosa with ganglion cells H&E (x40).
Calretinin positive staining in ganglion cells & nerve fibres in muscularis propria (x40)
Calretinin negative linear nerve fibrils in the lamina propria & submucosa of normal ganglionic segment (x40).
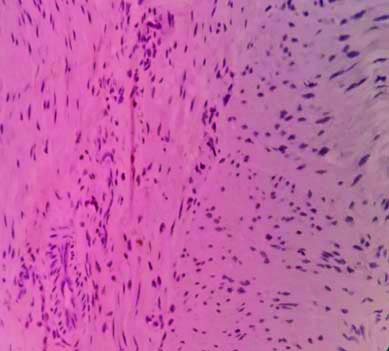
Absence of Calretinin IHC staining pattern in the aganglionic segment in the muscularis propria (x40).
Clinical presentation (n=45).
| Clinical presentation | No. | % |
|---|
| Failure to pass meconium | 21 | 46.7% |
| Chronic constipation | 12 | 26.7% |
| Abdominal distention | 6 | 13.3% |
| Failure to gain weight | 3 | 6.7% |
| Intestinal perforation | 3 | 6.7% |
A total number of 110 samples from 45 cases were examined by H&E and Calretinin stains, which included 31 each from dilated and transitional segments and 20 from constricted segments [Table/Fig-7]. Out of the 20 samples examined from constricted segments, H&E stained slides demonstrated absence of ganglions in 16 sections whereas Calretinin IHC revealed absence of ganglion cells in 14 sections. So Calretinin IHC eliminated over-diagnosis of HD on H&E in two cases. Out of 31 samples from dilated segments, H&E stain demonstrated ganglion cells in 20 biopsies (64.5%) whereas Calretinin IHC detected ganglion cells and calretinin positive nerve fibrils in 26 biopsies (83.9%). Similarly, out of 31 samples from transitional segments, H&E detected aganglionosis in 18 cases compared to 17 cases by Calretinin. Hence, Calretinin could demonstrate presence of ganglion cells in one extra sample. The subtype of total colonic aganglionosis was not observed in either H&E or Calretinin immunostaining. The postsurgical biopsy specimens studied in 14 cases by both H&E and Calretinin IHC revealed absence of ganglion cells in the distal margins in all 14 cases but showed ganglion cells in 8 (57.1%) samples by H&E staining compared to 12 (85.7%) samples in Calretinin IHC in the sutured proximal margin (p-value of 0.49). So, only 2 cases with absence of Calretinin expression required further corrective follow-up resection. So, out of the total 31 samples of clinically suspected HD studied 25 (80.6%) were HD and 6 (19.4%) were non-HD by H&E staining. After applying Calretinin IHC, Calretinin could demonstrate ganglion cells in three cases out of the 25 diagnosed as HD on H&E staining and hence the corrected number of cases of HD and non-HD were 22 and 9, respectively [Table/Fig-8]. So overall, three cases (9.7%) were misdiagnosed as HD by H&E morphology. Comparison between Calretinin IHC and H&E staining showed a sensitivity of 95.4% and a specificity of 55.5%. The positive predictive value was 84% and negative predictive value was 83.3%.
Assessing aganglionosis in clinically involved intestinal segments.
| Test applied | Dilated segment (n=31) | Transitional segment (n=31) | Constricted segment (n=20) |
|---|
| No. | % | No. | % | No. | % |
|---|
| Calretinin | 5 | 16.1 | 17 | 54.8 | 14 | 70 |
| H&E | 11 | 35.4 | 18 | 58.0 | 16 | 80 |
| Chi-Square: 1.5812, p=0.4535 |
Comparison between Calretinin and H&E findings.
| H&E | Calretinin | Total |
|---|
| Disease present | Disease absent |
|---|
| Disease Present HD | 21 | 4 | 25 |
| Disease Absent Non-HD | 1 | 5 | 6 |
| Total | 22 | 9 | 31 |
| Chi-Square: 10.64, p=0.001 |
HD- Hirschsprung’s Disease
Discussion
The HD is a genetically and phenotypically heterogeneous disorder characterised morphologically by aganglionosis in the distal colon or rectum and clinically by functional intestinal obstruction in the neonates and severe constipation in infants and younger children. Though Harald Hirschsprung first described the disease in 1888, the pathological features were not understood until the 1940s, when Whitehouse and Kernohan demonstrated that aganglionosis within the distal colon or rectum was the cause of functional obstruction that prevents propa-gation of peristaltic waves [5,6].
The most striking feature in the distal intestinal segment in HD is the absence of ganglion cells in the myenteric and meissner’s plexuses. It is a common condition of uncertain aetiology with an incidence of 1 in 5000 live births. In 80% cases, aganglionosis is restricted to the rectosigmoid colon (short segment disease); in 15-20%, aganglionosis extends proximal to the sigmoid colon (long segment disease); in 5%, aganglionosis affects entire large intestine and rarely extends to the small bowel [7]. The median age at which children are diagnosed with HD has progressively decreased over the past decades probably due to greater awareness of the disease. In the present study, the patient age ranged from 2 days to 2 year 9 months, with maximum cases (28, 62.2%) being in less than 6 months age group. There is an overwhelming preponderance of HD in the males with a male:female ratio of 3.4:1 in the more common short segment HD [8]. The study also observed a male:female ratio of 4:1 in the short segment HD group. Most often patients are diagnosed in the neonatal period, presenting with features of distended abdomen, delayed passage of meconium (more than 24 hours) and vomiting. When diagnosed later in childhood, the presentation is usually chronic constipation, distention and failure to thrive. In 10% cases, patients present with enterocolitis, fever, septicaemia or even potentially lethal intestinal perforation [9]. In this study, most common clinical presentation was failure to pass meconium in 21 (46.7%) cases, followed by chronic constipation in 12(26.7%) cases. Although intestinal perforation has been reported as a rare presentation in many series, three cases of intestinal perforation were encountered in this study, probably due to delayed reporting of patients to the hospital. Classical HD was encountered in 25 (80.6%) cases which corresponds to the study by Orr JD and Scobie WG, and long segment in 6(19.4%) cases compatible with the study by Kleinhaus S et al., [10,11].
Histopathological examination remains the gold standard of diagnosis which demonstrates the absence of ganglion cells in the narrow segment by H&E or IHC reactions. In this study full-thickness rectal biopsy has been used which is safe and yields a low number of inadequate biopsies [12]. H&E staining though routinely used has got several limitations like inter-observer variability, requiring considerable expertise for a reliable diagnosis, risk of false positive diagnosis in cases of hypoganglionosis and difficulty in diagnosis of ultrashort HD segment of less than 3-4 centimetres length above the anal ring because of physiological aganglionic zone. Calretinin when used as an adjunct to H&E markedly reduces interpretation error, help identifying transition zone and low level rectal biopsy and immature ganglion cells [13]. Enzyme histochemical stain acetylcholinesterase reaction (AchE) allows confirmation of aganglionosis in the affected segments. But these reactions have several limitations like necessity of frozen section processing, equivocal or false positive results and technical challenges [14]. Hamoudi AB et al., evaluated 131 specimens using AchE histochemistry and demonstrated false negative reactions in 29% cases [15]. An alternative is the IHC staining by various neuronal markers like Neuron Specific Enolase (NSE), Neuropeptide Y, S100 protein, calretinin etc., Calretinin, a calcium binding protein, plays an important role in organisation and function of the enteric nervous system. Ganglion cells and the nerve fibres express positive Calretinin staining in the nerve plexuses of normal bowel. Absence of Calretinin staining of the ganglion cell clusters and the fibres of submucosal and myenteric plexuses is considered diagnostic of HD. In 2004, Barshack I et al., studied calretinin IHC in ten large bowel specimens from patients with classic rectosigmoid HD and documented loss of Calretinin expression in aganglionic segments in both myenteric and submucosal nerve plexuses. Both ganglion cells and nerve fibres expressed calretinin in ganglionic segments of HD and in normal controls [2]. Kapur RP et al., demonstrated Calretinin stain to be more diagnostic in cases of HD when compared with Acetylcholineesterase stain with lesser interobserver variability [3].
Kapur RP et al., studied the pattern of Calretinin expression and opined that it is a superior alternative to AchE as an adjunctive diagnostic method [3]. In 2013, Kannaiyan L et al., proposed that Calretinin was extremely useful in diagnosing the suspicious and indeterminate cases of HD [16]. Rakhshani N et al., studied the usefulness of calretinin as a more specific accurate staining method [17]. Calretinin staining exhibited thin fibrillary pattern in majority, but dot granular or small stain aggregates crowding the cytoplasm in other cases. This study adds to the growing evidence that calretinin immunostaining is a valuable diagnostic aid during work up of cases of suspected HD and assists in either confirming or excluding the diagnosis of HD, thus obviating the need for repeat biopsies. Out of the 25 cases diagnosed as HD on the basis of H&E, Calretinin IHC ruled out HD in three cases by expression of positive staining pattern of ganglion cells. So, unnecessary surgery could be avoided in these three cases. On statistical analysis, the chi-square statistic is 10.64 and the p-value is 0.001. As p-value is less than 0.05, it is statistically significant.
On colonic biopsies, both H&E staining and calretinin IHC in the deconstricted segments were compared, where calretinin detected two more cases as non-HD. Also, in dilatted segments, six more cases were diagnosed to be non-HD while comparing both the stains. In the tran-sitional segment, calretinin correctly detected ganglion cells in one more case compared to H&E. Hence, a total number of nine cases were relabelled as non-HD on calretinin stain, thereby avoiding unnecessary surgical operative procedures in them. In this study, calretinin IHC staining was found to be extremely useful in correctly diagnosing the doubtful cases as it could detect the HD cases more accurately than that with H&E staining. The small sample size may be considered as a minor limitation of the present study.
Conclusion(s)
Calretinin immunostainig is a simple, highly sensitive and easily interpretable stain which assists as a reliable adjunctive technique over and above that of H&E staining in the identification of ganglion cells in the intestinal biopsy specimens. It can serve as a valuable and cost effective primary diagnostic tool for demonstrating intestinal aganglionosis and diagnosing cases of HD.
HD- Hirschsprung’s Disease