CASE REPORT
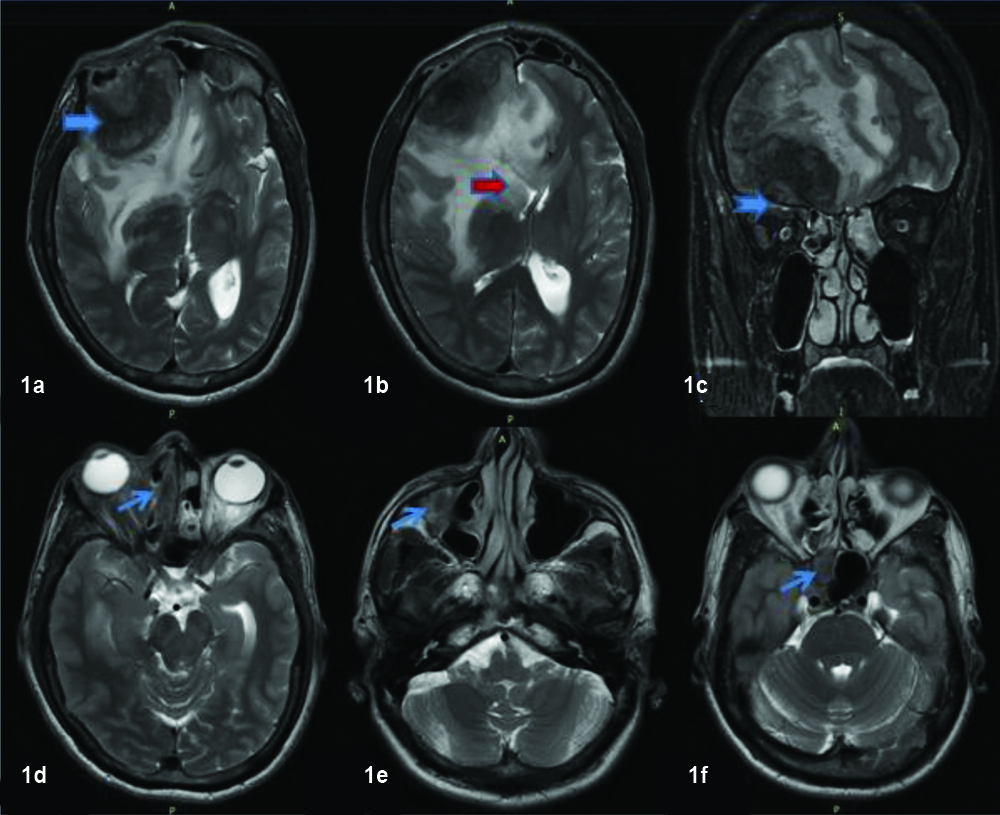
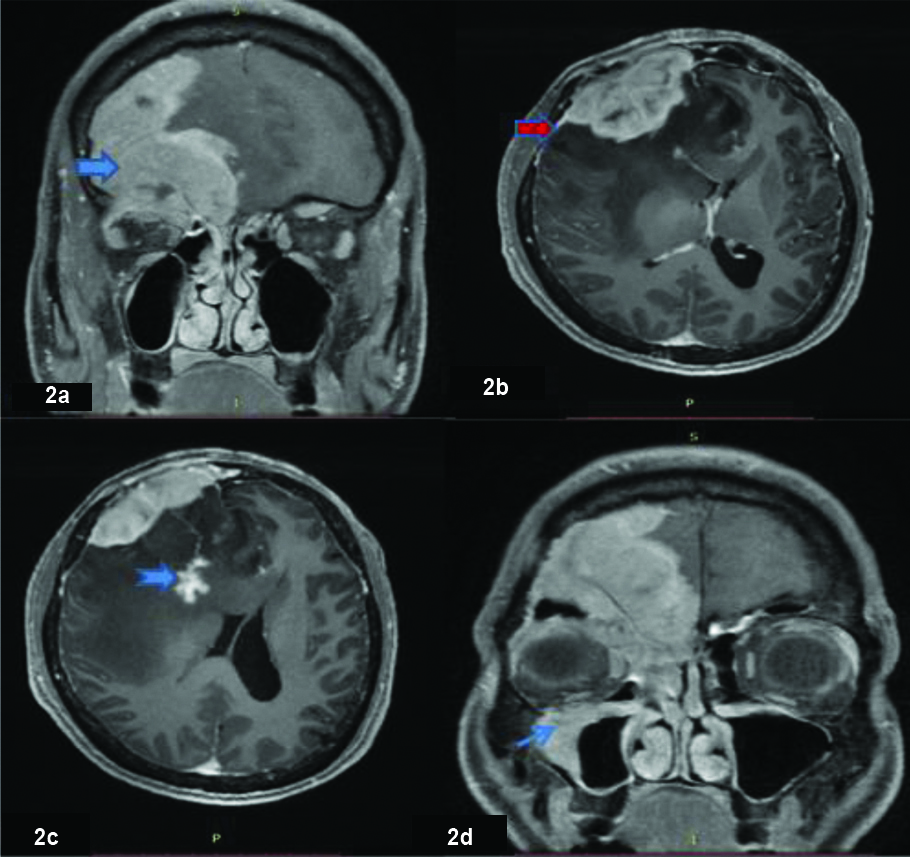
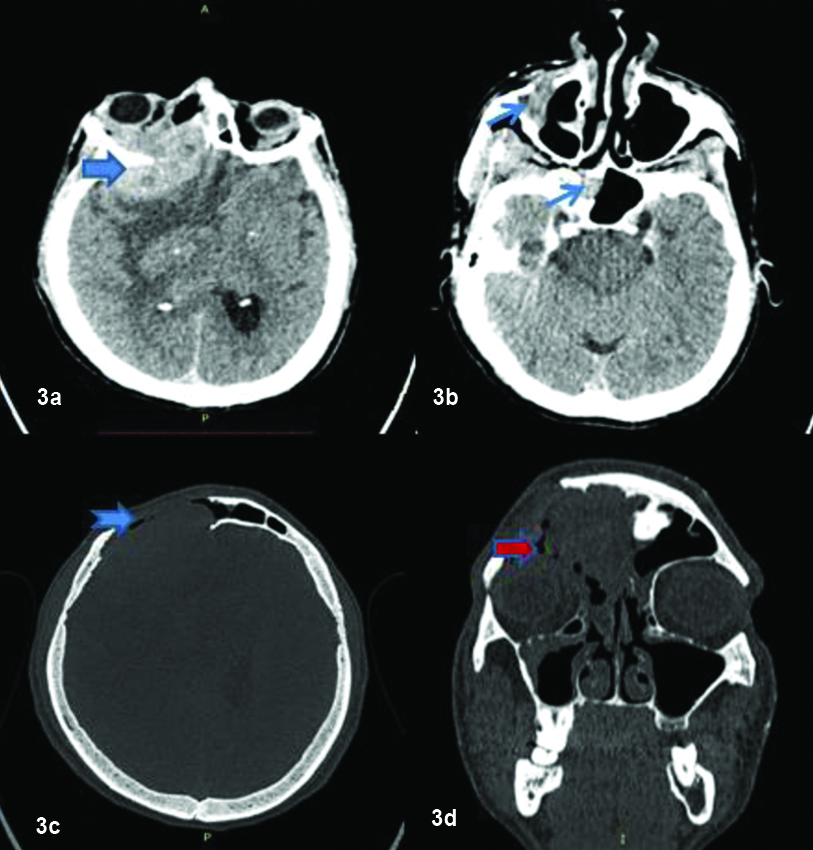
A 46-year-old male came to the Neurology Outpatient Department with history of unresponsiveness and seizure like episode lasting approx five minutes. There was history of three similar episodes in last six months. No history of tongue bite or blurring of vision in each of the episodes. There was no history of intake of medication or antiepileptics. Family history was unremarkable. On general examination, patient was anaemic. Local examination showed right eye proptosis with no obvious signs of periorbital inflammation. Neurological examination was normal with no focal neurological deficits. Rest of the systemic examination including cardiovascular and respiratory systems was within normal limits. He was referred to Radiology Department for MRI of brain to rule out underlying space occupying lesion in brain or orbit. On plain scans, MRI revealed a fairly large T2 hypointense extra-axial mass lesion along right frontal convexity [Table/Fig-1a] with associated osseous erosion. The lesion was seen to cause mass effect in the form of effacement of regional sulci and right lateral ventricle with shift of midline structures to left by 6 mm suggestive of subfalcine herniation [Table/Fig-1b]. Intraorbital extension of the lesion was seen into superior intraconal compartment resulting in proptosis of right eye [Table/Fig-1c]. A finding was reported on right sided pansinusitis involving frontal, ethmoid, maxillary and sphenoid sinuses with T2 hypointensities [Table/Fig-1d,e,f]. Contrast was administered for further characterization of the lesion. Postgadolinium study showed homogeneous enhancement of the lesion [Table/Fig-2a] along with enhancement of adjacent dura was also seen mimicking a dural tail sign [Table/Fig-2b]. Patchy enhancement also seen within the right frontal lobe white matter [Table/Fig-2c]. Sinuisitis components also showed post contrast enhancement [Table/Fig-2d]. For better assessment of bone involvement, Computed Tomography (CT) of brain and face was done. Correlative CT showed hyperattenuating extraxial mass lesion in right frontal region [Table/Fig-3a] along with right maxillary sinusitis [Table/Fig-3b]. Extensive osseous destruction of right frontal calvarium [Table/Fig-3c] and roof of right orbit [Table/Fig-3d] was seen. With the above MRI and CT constellation of findings, provisional imaging diagnosis of an agressive neoplastic process of dura-like invasive meningioma or small round cell tumour like lymphoma were raised and correlation with tissue sampling was suggested.
Axial and coronal T2 weighted images showing extraxial T2 hypointense lesion along the right frontal convexity (thick arrows) with disproportionate vasogenic edema and mass effect (Red arrows). Intraorbital extension (Notched arrows) seen with mild proptosis of right eye. Concomitant involvement of right ethmoid, maxillary and sphenoid sinuses seen with similar T2 hypointense lesions (thin arrows).
Postcontrast T1 weighted images showing enhancement of intracranial and intraoribital portions of the lesion with associated osseous erosions (thick arrow). Focal dural enhancement resembling dural tail seen (red arrow) along with enhancing lesion in right frontal lobe (Notched arrow). Also, shown enhancement of right maxillary sinusitis (Thin arrow).
CT images showing extensive osseous erosions of frontal calvarium (notched arrow) and orbit (red arrow) with associated hypderdense soft tissue component (thick arrow) along with right maxillary and sphenoid sinusitis (thin arrows).
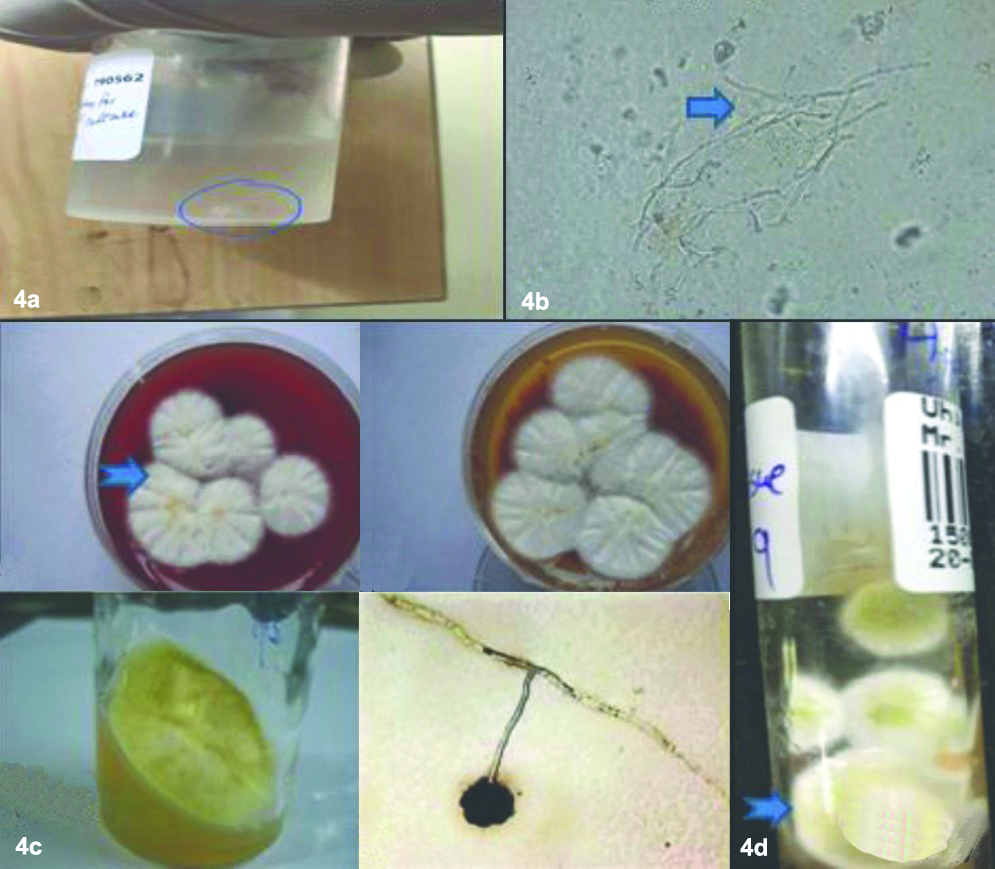
Subsequently, patient got admitted and underwent right fronto-temporal craniotomy for biopsy and tissue diagnosis. Histopathology of the right frontal lesion revelaed fibrocollagenous tissue [Table/Fig-4a,4b] showing dense granulomatous inflammatory infiltrate composed of lymphocytes, plasma cells, neutrophils and eosinophils. Many multinucleated giant cells were seen along with large areas of necrosis. Further micorbiological assessment with Periodic Acid-Schiff (PAS) and Gomori Methenamine Silver (GMS) stained sections highlighted acute angle branching septate hyphae of a fungus morphologically resembling Aspergillus fumigatus [Table/Fig-4b,c,d]. Ziehl Neelson (ZN) staining did not highlight acid fast bacilli. There was no evidence of malignant cells.
Isolate from biopsy specimen shows a fleshy white tissue (4A) which on low power KOH mount revealed septate hyaline fungal hyphae (thick arrow). Culture on blood and Mac agar showed yellowish green colored spores with powdery white growth at the base (Notched arrows) consistent with Aspergillus fumigatus species.
Retrospectively, the MRI images were again reviewed. Final diagnosis of invasive sino cranial aspergillosis infection with cerebritis of right frontal lobe was made.
Patient was started on intravenous voriconazole for 14 days and also underwent FESS with endoscopic clearance of sinuses. Patient showed good treatment response and was discharged on 15th day with oral voriconazole. Follow-up imging after two months showed complete resolution of sinus disease with no new lesions. Currently, patient is on follow-up with no new symptoms.
Discussion
Sinonasal fungal infections can either invasive or noninvasive. The presentation and clinical course of these infections is primarily determined by the immune status of the host varying from asymptomatic to life-threatening complications [1]. Karthikeyan P et al., in their study on incidence and presentation of fungal sinusitis in chronic rhinosinusitis patients found the incidence of sinonasal mycotic infections to be about 10% in these patients. They also concluded that all aspergillus infections were observed in immunocompetent patients and mucormycosis in immunocompromised patients and that endocopic sinus surgery followed by antifungal therapy plays a major role in the treatment of fungal sinusitis [2].
Among Aspergillosis species, Aspergillus fumigatus (90%) is the most common fungal pathogen followed by Aspergillus Niger and Aspergillus Flavus with maxillary sinus being the commonly involved sinus [3].
Invasive aspergillosis comprises of 5% of intracranial fungal infections [4]. Aspergillus infection in immunocompetent patients has been described in the tropical and subtropical area like Indian subcontinent. This can be attributed to hot and dry weather with abundance of Aspergillus spores, poor nutritional status, injudicious use of steroids and antitubercular drugs [5,6]. CNS infection occurs by different routes such as haematogenous dissemination from the lungs, direct extension from adjacent paranasal sinuses, middle ear cavity and orbits or from post surgical procedures [7].
Cranial aspergillosis often masquerades tumours such as meningioma owing to mass-like characteristics and intense contrast enhancement on MRI especially in immunocompetent individuals. In the present case report, we describe the imaging features of invasive aspergillosis in immunocompetent individual with emphasis on imaging features to distinguish this from meningioma.
The radiological appearance of CNS aspergillosis basically depends upon the clinical presentation and patient’s immune status. Our case was a CNS aspergillosis of sinonasal origin. A similar study by Siddiqui AA et al., of 20 CNS aspergillosis cases in immunocompetent individuals, showed that all of the patients had paranasal sinus involvement wherein they showed mucosal hyperenhancement as was seen in our case [8].
In immunocompromised individuals, hematogeneous spread from lungs is common resulting in ring enhancing lesions viz., abscess, meningitis, meningoencephalitis like features. Moreover, vasculitis is more common resulting in hemorrhage, mycotic aneurysms and small infarcts. Bone destruction and cavernous sinus involvement are unncommon features in these patients [9].
In contrast, CNS Aspergillosis in immunocompetent usually spreads from adjacent paranasal sinuses and present as enhancing intra or extra-axial masses with associated focal pachymeningeal thickening. They can cause skull base osteomyelitis due to direct invasion of the cranium from paranasal sinuses or may appear as granulomatous mass at the skull base [10,11]. Cavernous sinus extension and Internal Carotid Artery (ICA) encasement is frequent due to concomitant sinus disease in these individuals resulting in major territorial infarcts [12].
In the present case report, the extra-axial mass showed profound hypointensity on T2 weighted images. This appearance was also seen in the study done by Kumar D et al., [13], wherein the T2 hypointense signal correlates with the presence of paramagnetic elements like iron, manganese, magnesium, zinc that are essential for hyphal growth of the fungi but may also be related to blood breakdown products [14,15]. CT appearance of fungal sinusitis is nonspecific. But mostly appears hyperdense as seen in our case due to the calcium salts and metal ions deposited in necrotic areas [16]. Other features like sinus disease and areas of bony destruction can also be appreciated on CT.
Lesion enhancement in fungal sinusitis on MRI correlates with the immunocompetence level [7]. In this case, the patient was immunocompetent and lesion showed solid homogeneous enhancement. Similar pattern of enhancement was seen in study by Kumar D et al., along with dural enhancement seen adjacent to infected paranasal sinuses [12].
In such scenarios, intracranial fungal infections often mimic neoplasia as seen in this case. Among the neoplasms, most common differential considerations include metastases, meningioma, lymphoma, aggressive sinonasal tumour and neurogenic tumours (schwannomas). Based on the clinical presentation and imaging features, a differential diagnosis of invasive meningioma or small round cell tumour like lymphoma were considered.
Meningioma can mimic an intracranial aspergilloma. Both appear hyperdense on CT with adjacent hyperostosis or lytic destruction of calvarium. Both pathologies enhance homogeneously. Fungal granulomas present as enhancing masses sometimes with enhancement of the adjacent to the dura producing “dural tail sign” [17]. However, there are few differentiating features which help in making an accurate diagnosis.
Firstly, majority of meningiomas are isointense to gray matter on T1 and T2 weighted images whereas aspergillomas appear profoundly hypointense on T2 weighted images as seen in our case. However, fibrous and psammomatous meningioma can have a lower T2 signal like aspergilloma, but these subgroups of meningioma do not show homogenous, avid contrast enhancement [18].
Secondly, adjacent and concomitant sinus involvement with similar T2 hypointense appearance within the sinus and enhancement is a feature of invasive fungal sinusitis rather than meningioma. Widespread bony destruction is a feature of apergilloma rather than hyperostosis which is a feature of meningioma. Also, cavernous sinus invasion and large arterial territory infarcts are additional imaging features which favour fungal aetiology.
Sharma R et al., in their case report of two cases listed radiological features differentiating fungal granuloma from meningioma including MR spectroscopy. Presence of a lipid peak is suggestive of fungal aetiology and increased choline (3.2 ppm), decreased creatine (3.0 ppm) along with alanine peak at 1.48 ppm is characteristic of a meningioma [19].
Small round cell tumours like lymphoma can also mimic invasive fungal infection. Both appear hyperdense on CT and hypointense on T2 weighted images with homogeneous postcontrast homogeneous enhancement. Concomitant paranasal sinus involvement favours fungal infection whereas elevated lipid peaks and high Cho/Cr ratios on MR spectroscopy with diffusion restriction are helpful in differentiating lymphoma from CNS aspergilloma [20].
Commonly recommended treatment of aspergillosis includes surgical debridement along with antifungal therapy. Although intracranial aspergillosis is difficult to treat inspite of agressive surgeries, immunocompetent individuals have better outcome. Patient in this case report underwent surgical clearance along with intravenous voriconazole. He was discharged on oral voriconazole tablets with complete resolution of disease on follow-up imaging after two months. He is currently asymmptomatic and completely recovered.
So, early diagnosis and prompt treatment is of paramount importance. Careful evaluation of MRI signal intensity, anatomical location, enhancement pattern, concomitant sinonasal and orbital extension, and angio-aggressive nature of the mass with high index of suspicion can help to diagnose CNS aspergillosis in these patients.
To summarise, this case report highlights the importance to look for imaging clues like profound T2 hypointensity, associated sinus disease, cavernous sinus and ICA invasion to make an accurate diagnosis of fungal infection in immunocompetent individuals.
Conclusion(s)
Chronic invasive intracranial aspergilloma in an immunocompetent patient is of significant clinical relevance. Early identification is crucial to prevent significant morbidity and mortality. Sino cranial aspergillosis often mimics meningioma on imaging. Careful evaluation of MRI imaging features along with high index of suspicion help to arrive at an accurate diagnosis of CNS aspergillosis in these patients.
[1]. Gavito-Higuera J, Mullins CB, Ramos-Duran L, Sandoval H, Akle N, Figueroa R, Sinonasal fungal infections and complications: A pictorial reviewJ Clin Imaging Sci 2016 6:2310.4103/2156-7514.18401027403401 [Google Scholar] [CrossRef] [PubMed]
[2]. Karthikeyan P, Coumare VN, Incidence and presentation of fungal sinusitis in patient diagnosed with chronic rhinosinusitisIndian J Otolaryngol Head Neck Surg 2010 62(4):381-85.10.1007/s12070-010-0062-022319697 [Google Scholar] [CrossRef] [PubMed]
[3]. Katzenstein AA, Sale SR, Greenberger PA, Allergic aspergillus sinusitis, a newly recognized form of SinusitisJ Allergy Clin Immunol 1983 72:89-93.10.1016/0091-6749(83)90057-X [Google Scholar] [CrossRef]
[4]. Siddiqui AA, Shah AA, Bashir SH, Craniocerebral aspergillosis of sinonasal origin in immunocompetent patients: Clinical spectrum and outcome in 25 casesNeurosurgery 2004 55:602-11.10.1227/01.NEU.0000134597.94269.4815335427 [Google Scholar] [CrossRef] [PubMed]
[5]. Mohandas S, Ahuja GK, Sood VP, Virmani V, Aspergillosis of the central nervous systemJ Neurol Sci 1978 38(2):229-33.10.1016/0022-510X(78)90069-2 [Google Scholar] [CrossRef]
[6]. Dubey A, Patwardhan RV, Sampth S, Santosh V, Kolluri S, Nanda A, Intracranial fungal granuloma: Analysis of 40 patients and review of the literatureSurg Neurol 2005 63(3):254-60.10.1016/j.surneu.2004.04.02015734518 [Google Scholar] [CrossRef] [PubMed]
[7]. Ashdown BC, Tien RD, Felsberg GJ, Aspergillosis of the brain and paranasalsinuses in immunocompromised patients: CT and MR imaging findingsAJR Am J Roentgenol 1994 162(1):155-59.10.2214/ajr.162.1.82736558273655 [Google Scholar] [CrossRef] [PubMed]
[8]. Siddiqui AA, Bashir SH, Ali Shah A, Sajjad Z, Ahmed N, Jooma R, Diagnostic MR imaging features of craniocerebral Aspergillosis of sinonasal origin inimmunocompetent patientsActa Neurochir (Wien) 2006 148(2):155-66.10.1007/s00701-005-0659-316283103 [Google Scholar] [CrossRef] [PubMed]
[9]. DeLone DR, Goldstein RA, Petermann G, Salamat MS, Miles JM, Knechtle SJ, Disseminated aspergillosis involving the brain: Distribution and imaging characteristicsAJNR Am J Neuroradiol 1999 20(9):1597-604. [Google Scholar]
[10]. Shankar SK, Mahadevan A, Sundram C, Sarkar C, Chacko G, Lanjewar DN, Pathology of fungal infections in the central nervous system with special reference to the Indian scenarioNeurol India 2007 55:198-215.10.4103/0028-3886.3568017921648 [Google Scholar] [CrossRef] [PubMed]
[11]. Shamim MS, Siddiqui AA, Enam SA, Shah AA, Jooma R, Anwar S, Craniocerebral aspergillosis in immunocompetent host: Surgical perspectiveNeurol India 2007 55:274-81.10.4103/0028-3886.3568917921657 [Google Scholar] [CrossRef] [PubMed]
[12]. Marzolf G, Sabou M, Lannes B, Cotton F, Meyronet D, Galanaud D, Magnetic resonance imaging of cerebral Aspergillosis: Imaging and pathological correlationsPLoS One 2016 11(4):e015247510.1371/journal.pone.015247527097323 [Google Scholar] [CrossRef] [PubMed]
[13]. Kumar D, Nepal P, Singh S, Ramanathan S, Khanna M, Sheoran R, CNS aspergilloma mimicking tumours: Review of CNS aspergillus infection imaging characteristics in the immunocompetent populationJ Neuroradiol 2017 10.1016/j.neurad.2017.11.00129273531 [Google Scholar] [CrossRef] [PubMed]
[14]. Phuttharak W, Hesselink JR, Wixom C, MR features of cerebral aspergillosis in an immunocompetent patient: Correlation with histology and elemental analysisAJNR Am J Neuroradiol 2005 26(4):835-38. [Google Scholar]
[15]. Starkey J, Moritani T, Kirby P, MRI of CNS fungal infections: Review of aspergillosis to histoplasmosis and everything in betweenClin Neuroradiol 2014 24(3):217-30.10.1007/s00062-014-0305-724870817 [Google Scholar] [CrossRef] [PubMed]
[16]. Okamoto K, Furusawa T, Ishikawa K, Quadery FA, Sasai K, Tokiguchi S, Mimics of brain tumour on neuroimaging: Part IIRadiat Med 2004 22(3):135-42. [Google Scholar]
[17]. Omuro AM, Leite CC, Mokhtari K, Delattre JY, Pitfalls in the diagnosis of brain tumoursLancet Neurol 2006 5(11):937-48.10.1016/S1474-4422(06)70597-X [Google Scholar] [CrossRef]
[18]. Liu L, Lu Y, Peng W, Geng D, Wen J, Xiong J, Imaging features of intracranial psammomatous meningiomaJ Neuroradiol Oct 2017 10.1016/j.neurad.2017.06.00328689601 [Google Scholar] [CrossRef] [PubMed]
[19]. Sharma R, Garg K, Phalak M, Tandon V, Kumari K, Suri V, Aspergilloma masquerading as meningioma: An experience of two cases and review of literatureNeurol India 2019 67:1133-36.10.4103/0028-3886.26624431512657 [Google Scholar] [CrossRef] [PubMed]
[20]. Slone HW, Blake JJ, Shah R, Guttikonda S, Bourekas EC, CT and MRI findings of intracranial lymphomaAJR Am J Roentgenol 2005 184(5):1679-85.10.2214/ajr.184.5.0184167915855138 [Google Scholar] [CrossRef] [PubMed]