The Total Knee Arthroplasty (TKA) surgeries are on the rise as more and more surgeons have acquired expertise in the procedure and with increase in proportion of aging population, sedentary lifestyle and improved health infrastructure [1]. Postoperative pain after TKA ranges from moderate to severe intensity. This can hinder optimal knee mobilisation leading to delayed rehabilitation and patient dissatisfaction.
Majority of patients undergoing TKA have co-morbidities such as hypertension, diabetes mellitus, coronary artery diseases etc., and unbridled postoperative pain can be detrimental in such patients. Adequate pain relief and proper mobilisation can mitigate the incidence of thromboembolism, central sensitisation and development of chronic pain [2].
Several modalities of analgesia are used for TKA such as opioids, nonopioids, spinal or epidural analgesia, femoral, Sciatic Nerve Blocks (SNB) and local anaesthetic Infiltration between the Popliteal Artery and Capsule of the Knee (IPACK block), a novel regional technique which is awakening recent interest [3]. Multimodal analgesia combining two or more of the above mentioned modalities are recommended and found to be beneficial [4]. Of all these modalities, regional techniques are preferred over the others [5,6].
Ropivacaine is a long acting amide local anaesthetic which has a greater degree of motor and sensory differentiation and hence lower propensity for motor blockade. It also has decreased potential for CNS and cardiac toxicity when compared to Bupivacaine [7]. All these properties and its efficacy make ropivacaine a good choice for postoperative analgesia both in epidural as well as peripheral nerve blocks.
Epidural has the advantage of providing good analgesia and thus enabling early mobilisation and rehabilitation after TKA. Of late, peripheral nerve blockade is gaining popularity especially with the increasing use of ultrasound. Though knee joint is supplied by sciatic nerve as well, Femoral Nerve Block (FNB) without sciatic block is found to be enough to provide adequate analgesia after knee surgeries and can be used as a good alternative to epidural block [8].
The aim of this study was to compare the effects of CEA and CFNB on postoperative analgesia, knee rehabilitation and side-effects after TKA. Primary objective was to assess postoperative analgesia in terms of NRS scores and rescue analgesic requirement. Secondary objectives were to assess early knee rehabilitation indices and incidence of adverse effects in both groups.
Materials and Methods
This was a prospective cohort study which was conducted at the Government Medical College, Kozhikode, Kerala, India, after getting approval from Institutional Research and Ethics Committe (IREC) (GMCKKD/RP 2016/IEC/58).
For sample size calculation, the study by Shanthanna H et al., with average standard deviation 0.53 was considered to get a power of 80% and a confidence interval of 95% using the formula [8]:
Where, Zα=1.96, Zβ=0.84, SD=standard deviation, d=effect size 0.31. From this the sample size (n) needed was found to be 45 in each group.
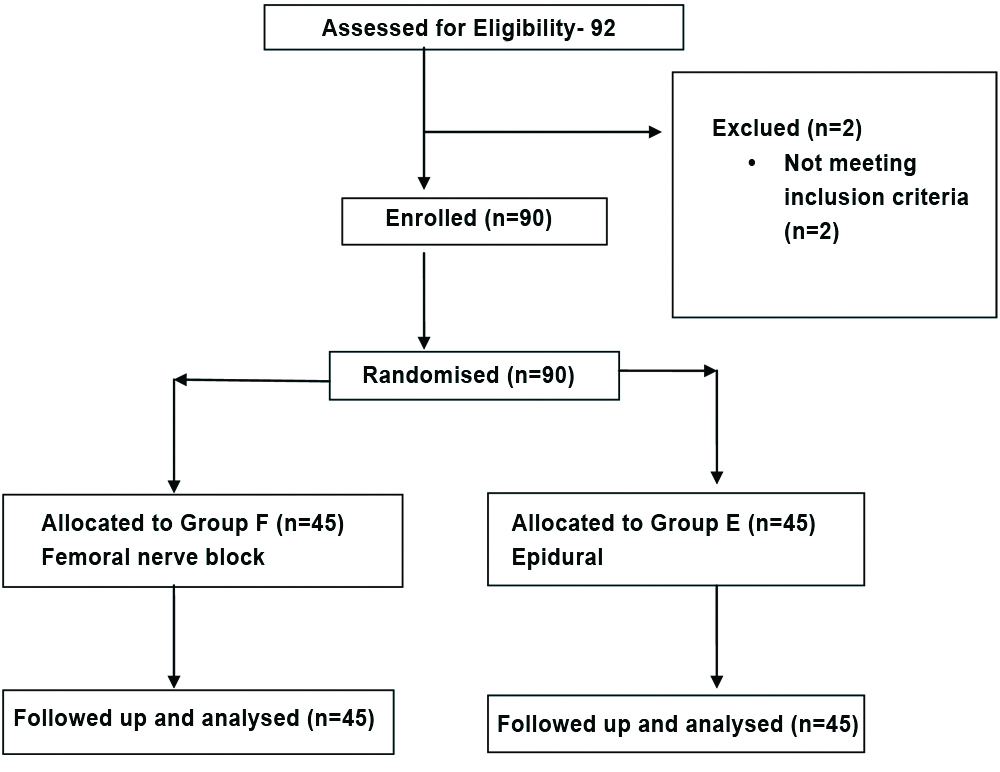
Ninety patients who underwent unilateral TKA were randomised using computer generated random number table and assigned to two groups. Patients who received CEA were included in Group E and those who received CFNB were included in Group F till the sample size of 45 was reached in each group.
After obtaining written informed consent, patients were selected according to inclusion and exclusion criteria.
Inclusion and Exclusion criteria: Patients who belonged to American Society of Anaesthesiologist Physical Status (ASA PS) I and II between the age of 20-65 years and of weight 40-80 kg were included in the study. Patients who had coagulopathy, infection at the site of block, history of chronic analgesic usage, allergy to local anaesthetics and duration of surgery more than 150 minutes were excluded from the study. Duration of surgery was defined as time taken from incision to skin closure [Table/Fig-1].
NRS was used to assess postoperative pain intensity. It consists of a scale from 0 to 10 where 0 represent “no pain” and 10 the “worst imaginable pain”. Patients were asked to indicate the strength of pain in this scale. The use of NRS was described to patients during pre-operative visit. All patients were premedicated with ranitidine 150 mg and metoclopramide 10 mg tablets on the night before and morning of surgery and tablet alprazolam 0.5 mg on night before surgery. They were advised fasting of eight hours for solids and two hours for clear liquids.
In the operating room, standard monitors like pulse oximeter, ECG machine, noninvasive blood pressure measuring equipment were used. After securing intravenous access, all patients were premedicated with injection midazolam 1 mg intravenously just before the procedure. For patients in group E, 18 G epidural catheter was inserted at L2-3 interspace using 18 G Tuohy needle by loss of resistance technique to air. A test dose of 3 mL of 2% lignocaine with 1 in 2 lac adrenaline was given to rule out intravenous or intrathecal catheter placement. All patients in both the groups were given preferential unilateral spinal anaesthesia at L3-4 level with 2.0 mL 0.5% bupivacaine (heavy) with 60 μg of buprenorphine as adjuvant. Surgery was commenced after getting a T10 sensory level of blockade. After the completion of surgery and before the analgesia of spinal wore off completely, patients in group F were given CFNB on the operated limb through an 18G catheter inserted under ultrasound guidance using in-plane approach and secured by tunnelling into subcutaneous tissue.
Vitals were monitored and kept stable throughout the procedure and the postoperative period. After surgery, a bolus of 8 mL 0.2% ropivacaine was given epidurally for group E and a bolus of 20 mL of 0.2% ropivacaine was given through femoral catheter for group F. Sensory block was assessed and confirmed using pinprick and cold sensation and continuous infusion of 0.2% ropivacaine at a rate of 5 mL per hour was started in both groups and continued for 72 hours. In postoperative intensive care unit, all patients were given oral acetaminophen 650 mg every six hourly on the day of surgery.
Postoperative analgesia was assessed using NRS score at 6, 12, 24, 48 and 72 hours after the surgery. Tramadol 50 mg was given intravenously as rescue analgesic when NRS score was ≥4. Rescue analgesics requirement during first and second POD was assessed. Epidural or femoral catheters were checked daily for ruling out migration or infection at the site of insertion and were removed after 72 hours surgery.
Postoperative knee rehabilitation indices were measured by percentage of patients who were able to sit at the bedside and stand with help on the first POD1. On POD2 percentage of patients who were able to stand without help, use the walker, and transfer to chair with help was analysed. Percentage of patients who were able to transfer to a chair and do walker mobilisation without help was looked for on POD3. Incidences of side-effects such as hypotension, dizziness, nausea, vomiting, urinary retention, respiratory depression (Respiratory Rate <10) and pruritus were also noted.
Statistical Analysis
Statistical analysis was done using IBM SPSS (Statistical Package for the Social Sciences) Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp. Continuous variables such as age, weight, duration of surgery were represented as mean with standard deviation and association between these variables were analysed using students t-test. The categorical variables such as sex, ASA PS, rescue analgesic requirement, rehabilitation indices were represented as numbers with percentages. Association between these variables was tested using chi-square test. NRS scores were represented as mean with standard deviation and association between the two groups was tested by Mann Whitney U test. The p-value less than 0.05 were considered as statistically significant.
Results
Patients in both groups were comparable with respect to demographic parameters like age, sex, and weight. Duration of surgery and ASA physical status were also comparable [Table/Fig-2].
Demographic features and duration of surgery.
| Parameters | Group E | Group F | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Age (years) | 50.36±5.9 | 49.36±6.2 | 0.437* |
| Weight (kg) | 63.67±6.32 | 63.62±5.96 | 0.937* |
| Duration of surgery (hours) | 2.0±0.9 | 1.9±0.5 | 0.78* |
| Sex (M:F) n (%) | 16:29 (35.6%: 64.4%) | 18:27 (40%:60%) | 0.664† |
*students t-test p-value, †chi-square test p-value. p-value <0.05 was significant
NRS score for 6, 12, 24, 48, 72 hours were similar in both groups. There was no significant difference between group E and group F in terms of NRS pain scores (p=0.673, 0.704, 0.905, 0.720, 0.870, respectively) [Table/Fig-3].
Numerical Rating Scale (NRS).
| Time (hours) | Group E Mean±SD | Group F Mean±SD | p-value* (Mann Whitney U test) |
|---|
| 6 | 3.98±1.27 | 3.87±1.2 | 0.673 |
| 12 | 4.01±1.09 | 4.11±1.11 | 0.704 |
| 24 | 2.76±0.86 | 2.78±0.90 | 0.905 |
| 48 | 1.87±0.87 | 1.93±0.89 | 0.720 |
| 72 | 1.53±0.63 | 1.51±0.66 | 0.870 |
*p-value <0.05 was significant
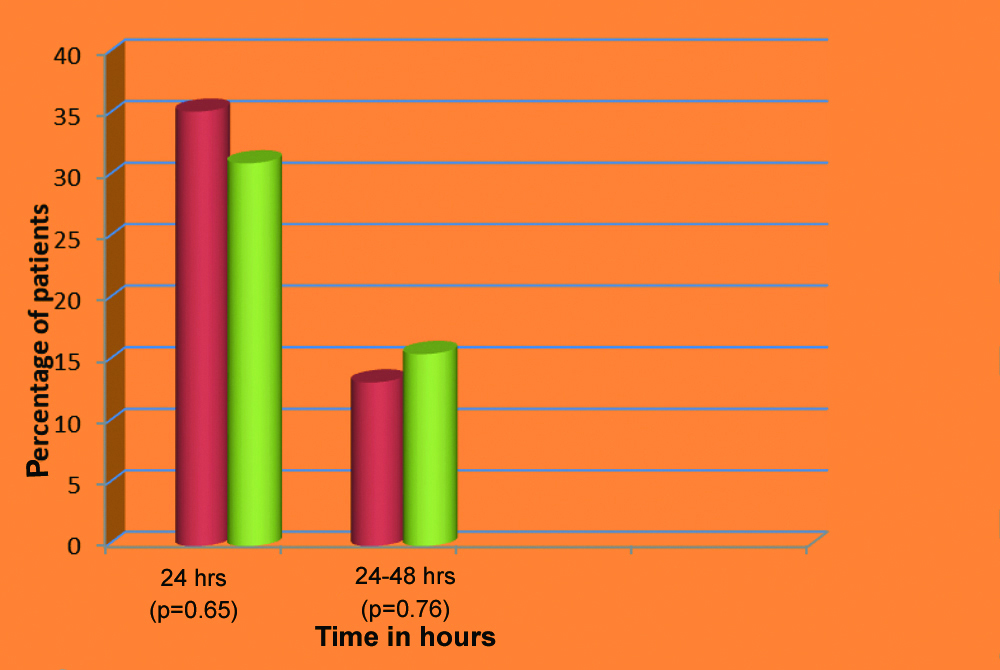
In the initial 24 hours, 35.3% of patients in Group E required rescue analgesic tramadol as against 31.1% of patients in Group F (p=0.650). Then in 24-48 hours, only 13.3% of patients in Group E and 15.6% of patients in Group F required tramadol as rescue analgesia (p=0.760) [Table/Fig-4].
Graph showing consumption of rescue analgesia.
Chi-square test p-value; Red bars represents E group and Green bars represents F group
There was no statistically significant difference between group E and group F with regard to attainment of rehabilitation indices on POD1, 2 and 3 [Table/Fig-5].
Table showing attainment of rehabilitation indices.
| Rehabilitation indices | Group E n (%) | Group F n (%) | p-value (Chi-square test) |
|---|
| POD 1 sit at bed side and stand with help | 34 (75.6%) | 32 (71.1%) | 0.630 |
| POD 2 stand without help, use walker and transfer to chair with help | 32 (71.1%) | 31 (68.9%) | 0.820 |
| POD 3 transfer to a chair and use walker without help | 28 (62.2%) | 30 (66.7%) | 0.660 |
POD:Postoperative day. p-value <0.05-significant
Two patients in group E had urinary retention. Other than that, none of the side-effects like hypotension, nausea, vomiting, dizziness, pruritus and respiratory depression were seen in either of the groups.
Discussion
Adequate analgesia in immediate postoperative period is essential after TKA as it can affect early physiotherapy and mobilisation. Out of many modalities for postoperative analgesia, epidural analgesia remains the gold standard [9]. However, Peripheral Nerve Blocks (PNB) is gaining popularity because of increase in use of ultrasound in the speciality of anaesthesia. Both FNB and epidural analgesia reduce opioid requirement and the associated adverse effects [12,13]. This allows early mobilisation, improved postoperative rehabilitation, patient satisfaction and reduced hospital stay. Despite the advantages, epidural is associated with adverse effects such as hypotension, urinary retention, pruritus etc., and sensory and motor blockade in the nonoperative leg which may hinder early initiation of physiotherapy. FNB is coming up in a big way with a very short learning curve and the use of ultrasound guidance making it more precise. FNB is less likely to have complications seen with central neuraxial techniques and can be used in situations where epidural is contraindicated. It is relatively safe to start concomitant prophylactic anticoagulants which pose a risk of epidural haematoma in the latter.
This study was conducted not to compare analgesia alone but also rehabilitation indices and side-effects between the CFNB and CEA groups. In this study, NRS scores for 6, 12, 24, 48 and 72 hours were mostly in the mild or moderate range and were similar in both epidural and CFNB groups. Rescue analgesic requirement in the first 24 hours and the next day was similar in both groups and it was also noted that the analgesic requirement for the second postoperative day was reduced to less than half of that of the first day in both groups. There was no statistically significant difference in rescue analgesic requirement between the groups. Thus, the present study showed similar efficacy of CEA and CFNB in postoperative analgesia after TKA surgeries.
Zaric D et al., compared epidural analgesia with continuous femoral- SNBs after TKA [9]. They had employed ropivacaine 2 mg/mL along with sufentanyl 1 μg/mL for the infusion. The median Visual Analogue Scale (VAS) scores were comparable in both groups. Barrington MJ et al., when comparing FNB and epidural analgesia for TKA in 112 patients and found that there was no significant difference in VAS scores between the two groups [10]. They had used ropivacaine 0.2% with fentanyl 4 μg/mL for epidural infusion and bupivacaine 0.2% for femoral infusion. There was no statistically significant difference between the groups with respect to doses of rescue analgesics also, irrespective of addition of opioids in epidural.
In meta analyses by Gerrard AD et al., and Fowler SJ et al., the pain scores were similar in both epidural and PNB groups irrespective of combining with sciatic block [14,15]. This shows that SNB is not a must add on to FNB for rendering adequate analgesia in knee surgeries. Park SJ et al., compared FNB combined with SNB to epidural in TKA [16]. There was no significant difference between the two groups in terms of pain score, motor blockade of the operative limb, range of motion of knee, or rehabilitation. The findings of these studies are in concordance with the present study. In contrast to findings of the present study, studies by Shanthanna H et al., and Sundarathiti P et al., suggest epidural is superior to FNB for pain control, especially in the early postoperative hours [8,17]. But study by Sakai N et al., showed superiority of FNB over epidural [18].
Postoperative knee rehabilitation is an important part of the overall management of patients undergoing knee surgeries and significantly affects the outcome. The assessment of the progress of rehabilitation is done by various parameters including assessment of range of movements of knee, continuous passive motion, straight leg raising test, ambulatory distance, performance of activity of daily living etc., [19].
Percentage of patients who achieved the rehabilitation indices was similar in both the groups and no statistically significant difference was there on POD 1, 2 and 3 with p-values of 0.630, 0.820 and 0.660, respectively. Results of the present study are similar to the prospective randomised study conducted by Sundarathiti P et al., who employed same rehabilitation indices as in this study [17]. In study by Al-Zahrani T et al., different indices were used such as postoperative daily mobilisation (p=0.80), knee joint range of motion (p=0.83), and straight leg test (p=0.98), and they were similar in both CFNB and epidural groups [20]. The findings in these studies are congruous with that of the present study.
Side-effects like hypotension, nausea, vomiting, and pruritus were not seen in any of the participants. Two patients in epidural group had urinary retention. However, there was no statistically significant difference in incidence of side-effects in both the groups. Gandhi HJ et al., used 0.2% ropivacaine, same as that used in the present study, but the rate of infusions was allowed to be increased upto 10 mL/h [11]. They found that though the number of side-effects such as hypotension and nausea, vomiting was more in epidural group, it did not achieve statistical or clinical significance. No statistically significant increased side-effects were noted in the study by Shanthanna H et al., also [8].
Park SJ et al., employing ropivacaine 0.2% and fentanyl 2 μg/mL, Vishwanatha S et al., using 0.0625% bupivacaine with fentanyl 2 μg/mL and Lu Yi et al., who used 0.375% ropivacaine in infusion found that the side-effects were significantly more in epidural group compared to femoral group [16,21,22]. These findings are in contrast to the present study and this may be attributed to the use of opioids and the concentration of the local anaesthetic agent used.
FNB and epidural have their own advantages and can provide effective postoperative analgesia and rehabilitation. Proper selection of local anaesthetic concentration and probable avoidance of opioids can help in reducing the side-effects. Thus, in the present study the postoperative analgesia and rehabilitation indices were comparable in femoral and epidural groups with no significant side-effects in either of the groups.
Limitation(s)
The motor blockade of limbs was not assessed specifically, though the rehabilitation indices indirectly indicate the same. Patient and surgeon satisfaction were also not assessed.
Conclusion(s)
CFNB is as effective as continuous epidural block for postoperative analgesia and knee rehabilitation after TKA with no significant side-effects with either technique. CFNB can be used as an alternative especially in situations where epidural fails or is contraindicated. For future research, patient-controlled epidural and femoral infusions of local anaesthetic with and without opioids can be studied. Effectiveness of IPACK blocks in post operative analgesia in TKA can also be explored.
*students t-test p-value, †chi-square test p-value. p-value <0.05 was significant
*p-value <0.05 was significant
POD:Postoperative day. p-value <0.05-significant