Endocrinopathy Causing Skeletal Decalcification and Ectopic Calcification Highlighted by Imaging Tour
PRK Bhargav1, Sunil Kumar Kota2, M Sabaretnam3
1 Consultant, Department of Endocrine Surgery, Vijayawada, Andhra Pradesh, India.
2 Consultant, Department of Endocrinology, Endocare Clinic, Berhampur, Odisha, India.
3 Associate Professor, Department of Endocrine Surgery, SGPGIMS, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. PRK Bhargav, Gokul Street, Currency Nagar, Vijayawada, Andhra Pradesh, India.
E-mail: endoanswers@gmail.com
Primary Hyperparathyroidism (PHPT) is an endocrine disorder which is caused by increased production of Parathyroid Hormone (PTH). Hypercalcemia leads to a number of symptoms and may cause patient’s morbidity and even mortality if left untreated. In the present case, a 21-year-old female presenting with frequent attacks of urinary tract infection, diffuse bone pain and episodic pain abdomen since 15 months. On clinical, biochemical and radiological evaluation, the case was diagnosed as PHPT due to left superior parathyroid adenoma. Patient underwent uneventful surgical parathyroidectomy following preoperative optimisation. She achieved normocalcaemia without any surgical complications. This case is presented to highlight the impact of hyperparathyroidism on calcium metabolism leading to extensive skeletal decalcification and ectopic deposition of calcium leading to end organ damage. Various images are used to highlight this phenomenon of decalcification and calcification.
Hyperparathyroidism, Nephrocalcinosis, Osteoporosis, Parathyroidectomy, Pancreatitis, Surgery
Case Report
A 21-year-old female presented with clinical history of recurrent burning micturition and frequency of urination for past 20 months. She also complained of episodic pain abdomen and diffuses bone pains since 15 months. Patient also gave history of two attacks of seizures in past six months. She had multiple orthopaedic, neuropsychiatric and urology consultations, but was only treated symptomatically. Later, a local physician detected hypercalcaemia and referred her to our Endocrine Surgery Department. The case was provisionally diagnosed as metabolic bone disease and was investigated for the cause. There was no family history suggestive of similar disease. Biochemistry was consistent with diagnosis of PHPT with serum parathyroid hormone of 367 pg/mL. Corresponding serum calcium, phosphorus, alkaline phosphatase, creatinine, vitamin D as follows- 12.7 mg/dL, 2.4 mg/dL, 345 IU/L, 1.4 mg/dL 25 ng/dL respectively and Bone Mineral Density (T score) at hip, spine and radius of -4.5, -3.5 and –5.0, respectively. Thorough clinical, biochemical and radiological evaluation confirmed the diagnosis of PHPT caused by single superior parathyroid gland enlargement as depicted in Computed Tomography (CT scan) of neck [Table/Fig-1a,b].
a) Coronal section of Contrast Enhanced Computed Tomography (CECT) shows hypodense left superior extrathyroidal lesion; b) Ex-vivo specimen of surgically excised left superior parathyroid adenoma corresponding to the lesion on CECT scan.
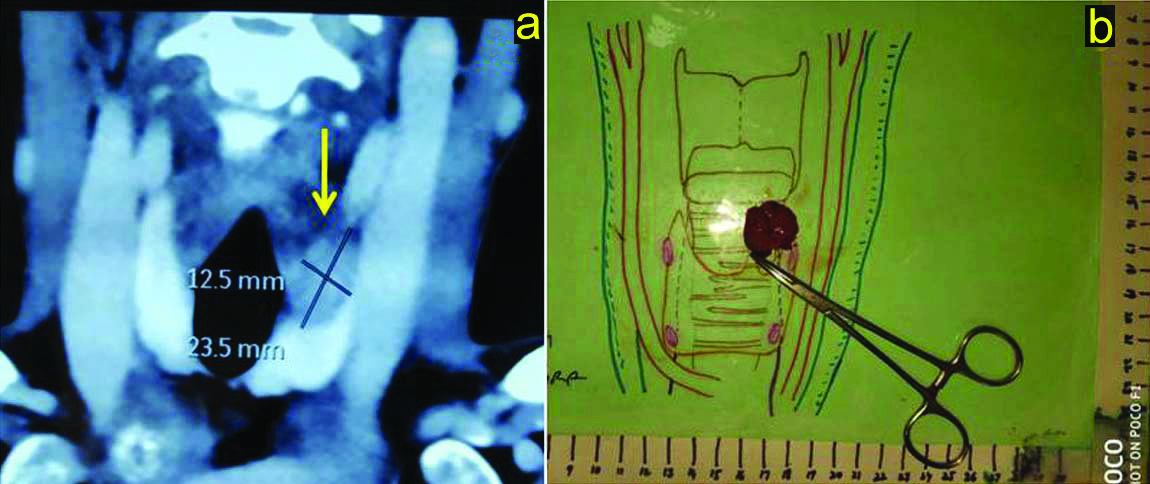
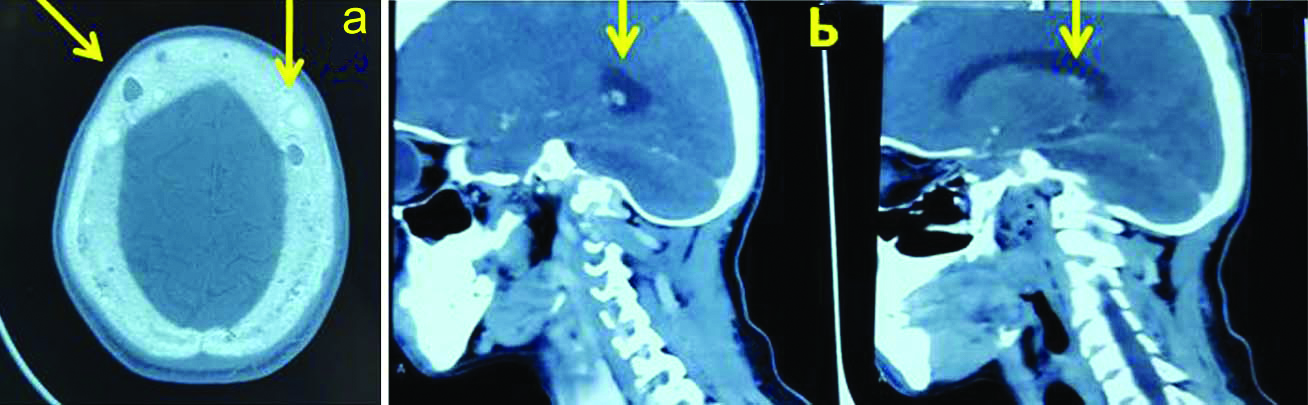
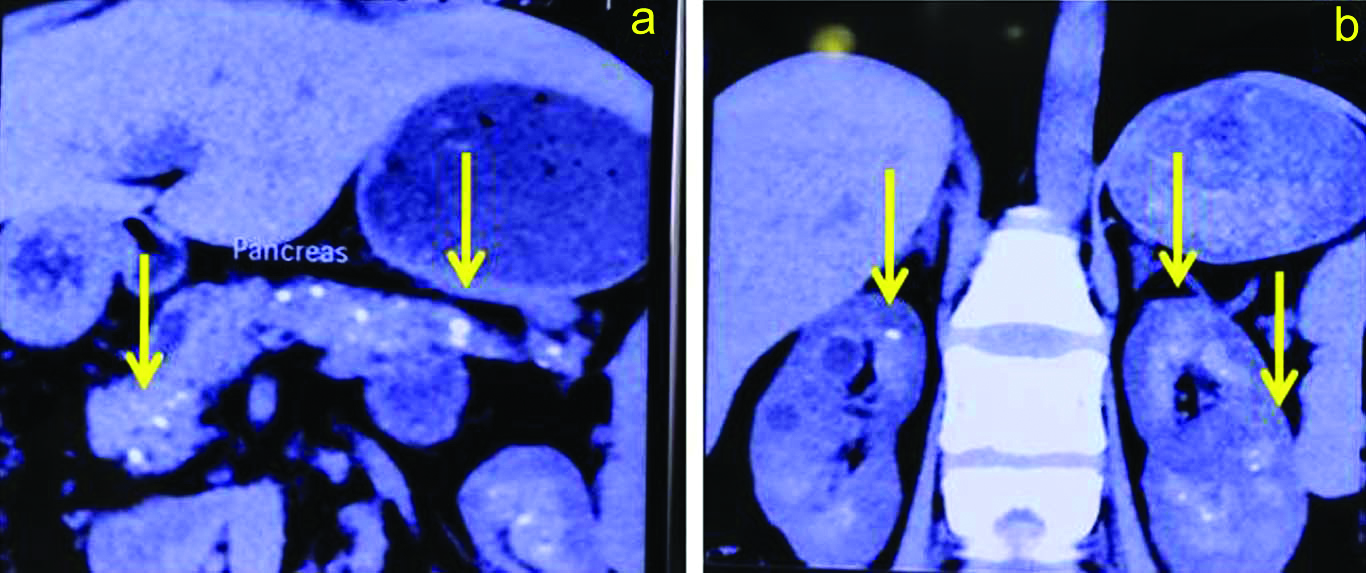
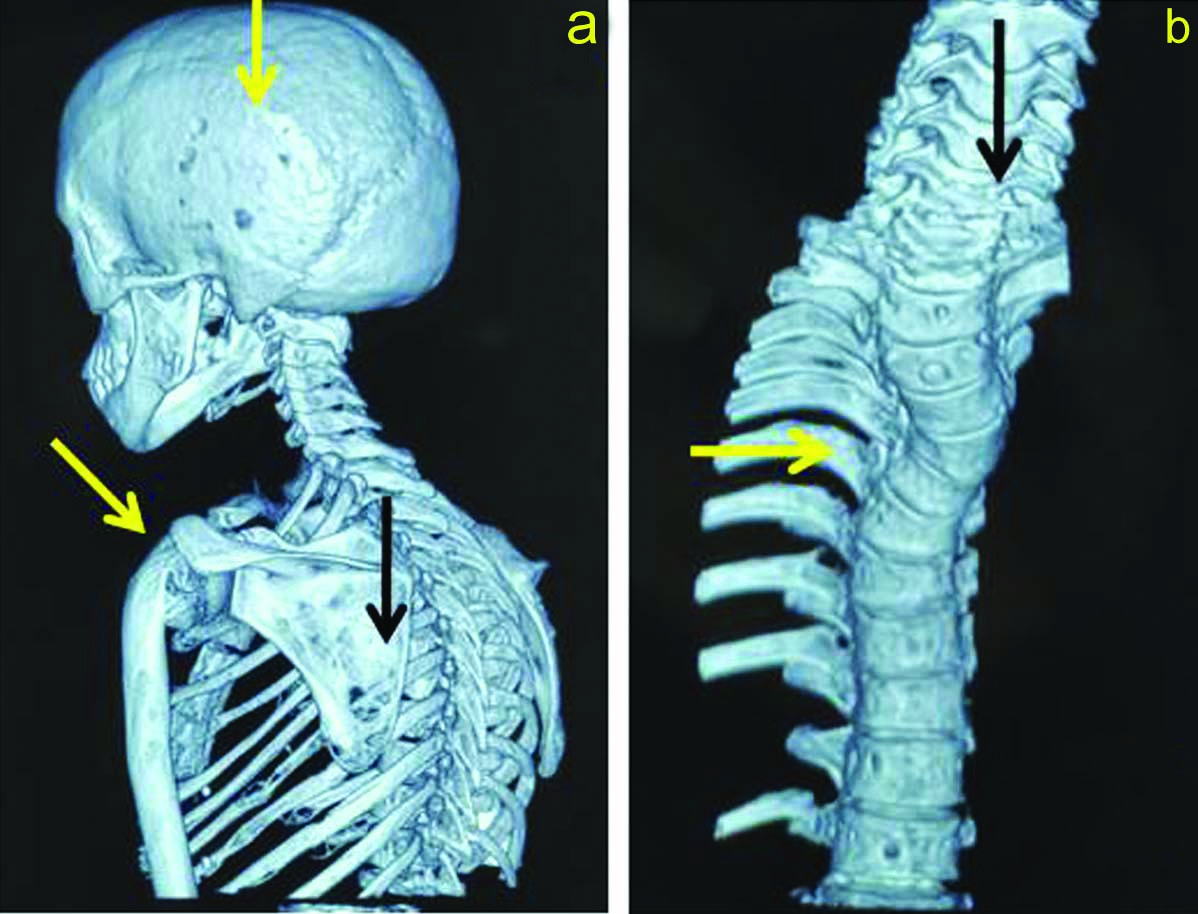
The differential diagnosis of hypercalcaemia such as osteomalacia, multiple myeloma, steroid intake, tuberculosis, sarcoidosis, drug intake was excluded. Multiple Endocrine Neoplasia (MEN) syndromes and other familial syndromic associations were excluded. Plain CT scan of skull showed extensive osteoporosis and punched out osteopenic areas [Table/Fig-2a] and CT scan brain showed ectopic basal ganglia calcifications [Table/Fig-2b]. Contrast Enhanced Computed Tomography (CECT) scan of abdomen shows extensive ductal and periductal calcifications in pancreas [Table/Fig-3a]. CECT scan of Kidneys, Ureters, and Bladder (KUB) region shows bilateral nephrocalcinosis [Table/Fig-3b]. With this diagnosis, author undertook focussed parathyroidectomy under general anaesthesia and a 2.0×2.5 cm vascular right superior parathyroid adenoma was excised [Table/Fig-1b]. Postoperatively, she had symptomatic hypocalcaemia from 3-6 days with least serum calcium level of 6.4 mg/dL. She was treated with parenteral calcium infusions and vitamin D supplements till normocalcaemia was achieved and maintained. Normocalcaemia was achieved at three months follow-up. Histopathology was reported as benign classical type Parathyroid adenoma. At 12 months follow-up, patient was normocalcaemic, euglycaemic with no attacks of urinary tract infection, pancreatitis or seizures. Whole body skeletal 3D CT scan shows extensive osteoporosis, punched out osteopenic zones and deformed bones [Table/Fig-4].
a) CT scan of skull shows extensive osteoporosis, punched out osteopenic areas and areas of new bone formation; b) CT scan brain shows basal ganglia and periventricular calcifications.
a) CECT of abdomen shows extensive ductal and periductal calcifications in pancreas; b) CECT of KUB shows bilateral nephrocalcinosis.
a) 3 D CT scan of skeleton shows diffuse osteoporosis, punched out osteopenic zones in skull, scapula, ribs, sternum, vertebrae; b) Deformed kyphoscoliotic spinal column with osteopenia.
Discussion
Primary Hyperparathyroidism (PHPT) is often popularly known by popular adage "bones, stones, groans, moans, fatigue overtones" [1]. It is one of the frequent endocrinopathies with a clinical spectrum ranging from asymptomatic biochemical hyperparathyroidism to debilitating and deadly hypercalcaemic crisis. Untreated PHPT can lead to mortality due to hypercalcaemic crisis or end organ damage due to renal failure, multiple bone fractures etc., [2]. Inappropriately, elevated serum PTH targets bones leading to its decalcification followed by resultant hypercalcaemia. This diagnostic feature was appropriately highlighted in this case [3]. Elevated serum calcium levels get deposited at physiological ectopic sites leading to a process called calcification. Present case highlights this phenomenon of ectopic calcification at multiple end organs often leading to their deranged function [4]. As seen in the present case, left superior parathyroid adenoma lead to PHPT, which caused decalcification of bones and calcific deposits in pancreas (leading to chronic and acute on chronic pancreatitis), basal ganglia of brain and kidneys (nephrocalcinosis). Fortunately, this patient got timely intervention and underwent successful parathyroidectomy ensuring cure and obviating catastrophic end organ damage of pancreas (which leads to secondary diabetes) and renal failure due to calcification and bone fractures due to decalcification. Surgical excision of all pathological adenomatous parathyroid tissue (in this case single adenoma) was the only definitive option for symptomatic PHPT such as this case. The aetiology in present case report was consistent with the reported literature, that the commonest cause of PHPT is solitary sporadic adenoma [5]. Similarly, histopathology was the commonest subtype-classical adenoma [6]. Due to severe osteoporosis, the postoperative recalcification leads to initial hypocalcaemia, followed by achievement of normocalcaemia over a period of days to weeks [7,8], as shown in this case. Further, these images and report highlight the need for a high index of suspicion, timely diagnosis and surgical intervention to treat this commonest calcifying endocrinopathy. The reasons for presenting this case with pictoral assay are four fold: 1) To highlight the pathophysiology of PHPT affecting calcium metabolism; 2) End organ effects of ectopic calcium deposits; 3) Above imagings and similar findings should alert clinician/ radiologist to consider PHPT in differential diagnosis; and 4) Serves as a good teaching material to Post Graduates/Residents of Radiology, Medicine, Endocrinology, Urology, Orthopaedics, Neurology, Gastroenterology and Surgery.
Conclusion(s)
Primary Hyperparathyroidism (PHPT) caused by solitary benign adenoma leads to skeletal decalcification and ectopic calcification. Familiarity with these imaging findings should prompt clinicians towards early diagnosis and surgical cure of PHPT.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 17, 2020
Manual Googling: Oct 10, 2020
iThenticate Software: Dec 22, 2020, (8%)
[1]. Madkhali T, Alhefdhi A, Chen H, Elfenbein D, Primary hyperparathyroidismTurkish J Surg 2016 32:58-66.10.5152/UCD.2015.303226985167 [Google Scholar] [CrossRef] [PubMed]
[2]. Singh DN, Gupta SK, Kumari N, Krishnani N, Chand G, Mishra A, Primary hyperparathyroidism presenting as hypercalcaemic crisis: Twenty-year experienceIndian J Endocrinol Metab 2015 19(1):100-05.10.4103/2230-8210.13176325593835 [Google Scholar] [CrossRef] [PubMed]
[3]. Cummings D, Vannahme M, Stanworth H, A case of multi-organ failure due to hyperparathyroidism-related hypercalcaemiaJ Intensive Care Soc 2020 21(3):274-77.10.1177/175114371983217932782468 [Google Scholar] [CrossRef] [PubMed]
[4]. Tahim AS, Saunders J, Sinha P, A parathyroid adenoma: Benign disease presenting with hyperparathyroid crisisCase Rep Med 2010 2010:59618510.1155/2010/59618521209735 [Google Scholar] [CrossRef] [PubMed]
[5]. Starker LF, Björklund P, Theoharis C, Long WD 3rd, Carling T, Udelsman R, Clinical and histopathological characteristics of hyperparathyroidism-induced hypercalcemic crisisWorld J Surg 2011 35(2):331-35.10.1007/s00268-010-0840-621042912 [Google Scholar] [CrossRef] [PubMed]
[6]. Cordellat IM, Hyperparathyroidism: Primary or secondary disease?Rheumatol Clin 2012 8:287-91.10.1016/j.reumae.2011.06.002 [Google Scholar] [CrossRef]
[7]. Alabdulkarim Y, Nassif E, Delayed serum calcium biochemical response to successful parathyroidectomy in primary hyperparathyroidismJ Lab Physicians 2010 2(1):10-13.10.4103/0974-2727.6670021814399 [Google Scholar] [CrossRef] [PubMed]
[8]. Anwar F, Abraham J, Nakshabandi A, Lee E, Treatment of hypocalcaemia in hungry bone syndrome: A case reportInt J Surg Case Rep 2018 51:335-39.10.1016/j.ijscr.2018.08.01130245357 [Google Scholar] [CrossRef] [PubMed]