Case Reports
Case 1
A 20-year-old male patient presented in the emergency unit with weakness of both lower limbs followed by upper limbs (lower > upper) since 12 hours which was insidious in onset and gradually progressive in nature and shortness of breath since six hours. There was flaccid hyporeflexic weakness of the limbs (corresponding to the Medical Research Council grade 3/5 in all muscles of the upper extremities - proximal and distal and 1/5 in lower extremities-proximal and distal) and bilateral flexor plantar responses. The bowel and bladder were uninvolved. He had a history of fever about a week back but was afebrile at the time of presentation. There was no other significant past history of any similar illness, chronic diseases or any previous hospitalisation or surgery, any family or personal history. He was having high respiratory rate (30 breaths/min), tachycardia (110 beats/min, regular) and hypotension (94/62 mm Hg) and since his oxygen saturation was dipping, he was intubated (later tracheostomised and ventilated) and admitted in the ICU.
In ICU, diagnosis of GBS was made on the basis of CT Scan head (no significant abnormality), Cerebrospinal Fluid Chemistry (increased CSF protein with normal cell count) and other haematological evaluations. ECG was normal. Treatment was mostly aimed at giving respiratory support, maintaining oxygen saturation and monitoring Arterial Blood Gas (ABG) status, treating chest infections (Ventilator-Associated Pneumonia-VAP) using antibiotics, giving deep venous thrombosis prophylaxis and pulmonary rehabilitation. Patient received steroids and immunoglobulin for GBS. Joint mobilisation and regular posture change started early to prevent joint contractures and pressure ulcer respectively.
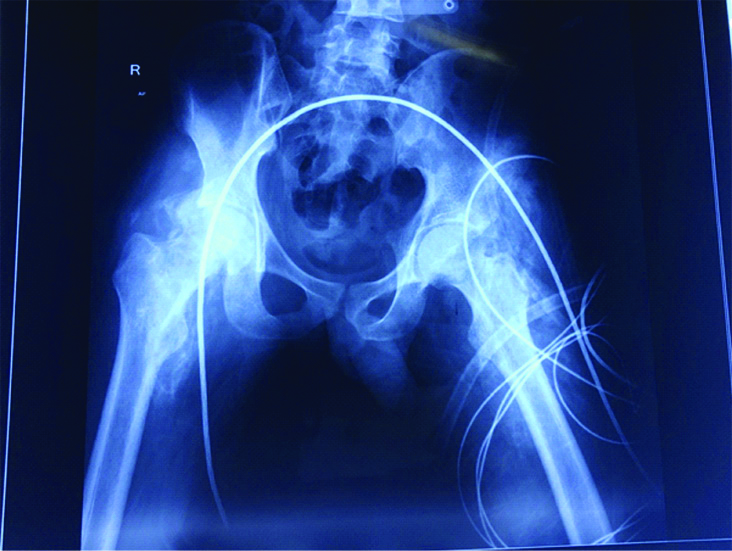
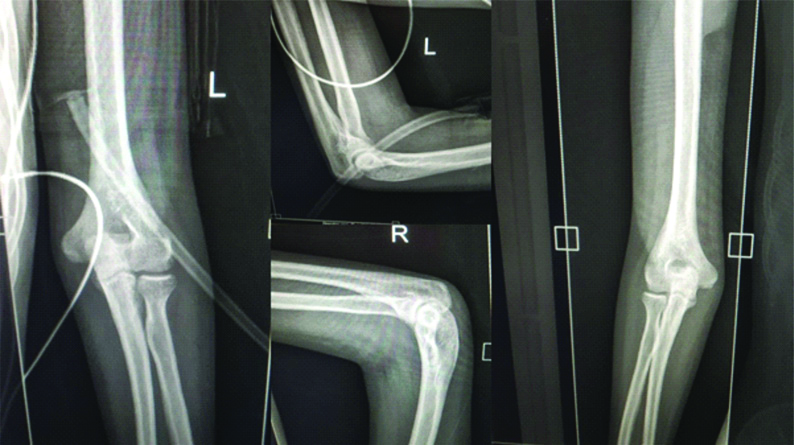
After about two months of ICU management, patient complained of insidious onset and gradually progressive bilateral hip joint pain and stiffness. The pain aggravated on joint mobilisation and relieved on rest or medications. There was no erythema, swelling, bony outgrowth or palpable warmth. Muscle power improved to 2/5 in lower limb. Passive range of motion of right hip flexion was 35 degrees, abduction 20 degrees, internal rotation was 10 degrees and external rotation was 30 degrees. While that of left hip was 30 degrees of hip flexion, 20 degrees abduction, 15 degrees internal rotation and 30 degree external rotation. Erythrocyte Sedimentation Rate (ESR) was 45 mm in 1st hour (normative range <20 mm in 1st hour), C-reactive Protein was 12.2 mg/dL (normative range <6), Total leukocyte count was 9260/mcL (normative range 4000-12000), Alkaline Phosphatase was 420.11 U/L (normative range 39-117), Serum Calcium was 9.13 mg/dL (normative range 8.8-10.6), Serum Magnesium was 1.77 mg/dL (normative range 1.8-2.6) and Serum Phosphate was 3.44 mmol/L (normative range 2.5-4.5). Digital X-Ray Pelvis and Bilateral Hip revealed massive HO in both hip joints [Table/Fig-1]. Patient also had pain and stiffness in bilateral elbow (Range of motion restricted to 90 degrees of flexion in both elbows), but digital x-Ray was within normal limit [Table/Fig-2]. Patient being in ICU, he could not be sent for triple phase bone scan of both elbows.
Digital radiograph showing matured HO in bilateral hip joints of Case 1.
HO: Heterotopic ossification
Digital radiograph showing AP and lateral views of both elbows of Case 1.
AP: Antero-posterior
In view of matured HO, tablet Indomethacin 75 mg (sustained release) was prescribed for six weeks, range of motion exercises (within permissible range, without excessive vigorous movement or massage) and pulmonary rehabilitation (postural drainage) was continued.
Patient reported significant pain relief and improvement in range of motion on follow-up and was asked to continue tablet indomethacin, range of motion exercises and postural drainage.
Case 2
A 24-year-old male patient presented in emergency room with acute onset slurred speech since eight hours associated with excessive salivation and weakness of bilateral upper limbs followed by lower limbs since six hours. The patient reported of diarrhoea/gastro-intestinal infection one week back. There was no previous history of similar illness, any significant family history, fever, fatigue, weakness or any toxin intake.
On examination, his pulse was 93 beats per minute, regular, normal volume and character with no radio-femoral delay, blood pressure was 138/78 mm Hg, oxygen saturation was 93%. Attitude of the patient was supine with inability to lift his neck or no bed mobility and bilateral facial paralysis. Neurological examination revealed difficulty in speech and swallowing. Neck flexors and extensors were weak. There was flaccid paresis of the limbs (corresponding to Medical Research Council grade 1/5 in all muscles of the upper extremities - proximal and distal and 1/5 in lower extremities – proximal and distal) and bilateral flexor plantar responses. The bowel and bladder were not involved. CT scan of head was clear. Neostigmine test was negative, ruling out Myasthenia Gravis. Cerebrospinal fluid study revealed albuminocytologic dissociation and hence, a diagnosis of GBS was made. Single Breath Count (SBC) was less than five so the patient was admitted in the ICU and was intubated.
Treatment was directed at giving respiratory support, hence he remained sedated and ventilated. The treatment he received in the ICU included steroids and immunoglobulin therapy. He had many episodes of chest infections VAP which were treated with antibiotics. Rehabilitation in terms of joint mobility, regular posture change to prevent pressure ulcer and pulmonary rehabilitation (including postural drainage) was started after one month.
After about six weeks of regular rehabilitation (Day 75 in ICU), patient complained of insidious onset, gradually progressive pain in bilateral hip joints (left > right). On examination, there was no redness, swelling, bony outgrowth or palpable warmth over the joint. Muscle power was 1/5 in all proximal lower limb muscles. Passive range of motion was restricted to 80 degree of flexion, 20 degree of internal rotation and 35 degree of external rotation in left hip and 90 degree of flexion, 30 degree of internal rotation and 40 degree of external rotation in right hip. ESR was 62 mm in 1st hour (normative value <20), C-reactive protein 73.47 mg/L (normative value <6), alkaline phosphatase 92.09 IU/L (normative range was 39-117), total leukocyte count 5030/mcL (normative range 4000-12000), serum calcium 8.89 mg/dL (normative range 8.8-10.6), serum magnesium 1.93 mg/dL (normative range 1.8-2.6) and serum phosphate was 3.97 mg/dL (normative range 2.5-4.5). The digital radiologic film of pelvis and bilateral hip showed mature HO on the Inferomedial and superolateral aspects of both the hip joints [Table/Fig-3,4].
Digital X-Ray left hip of case 2 showing HO in left hip.
HO: Heterotopic ossification
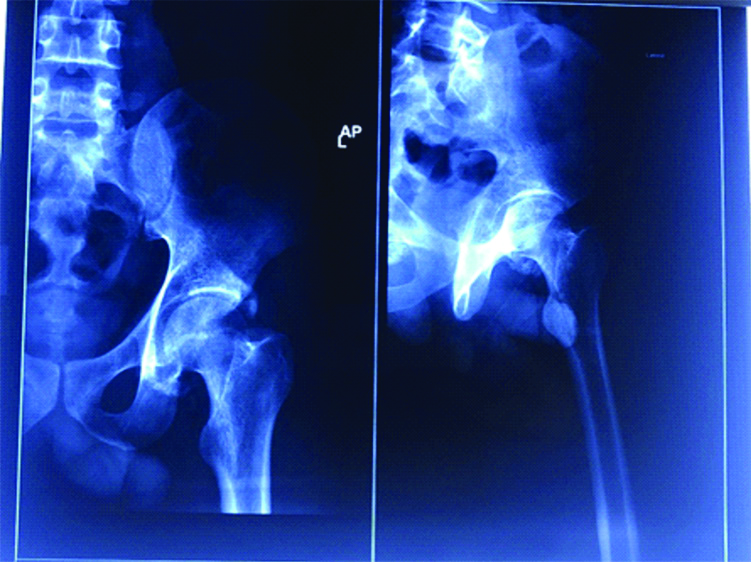
Digital X-Ray of pelvis and bilateral hip of case 2 showing HO in both hips.
HO: Heterotopic ossification

Patient was prescribed tablet indomethacin 75 mg (sustained release) for six weeks, range of motion exercises of all joints (including hip joint in painless range without any vigorous movement or massage) and pulmonary rehabilitation. Patient was asked to continue this on follow-up and report any complications or fresh complaints.
Discussion
Heterotopic Ossification is the formation of bone outside the normal skeleton that can occur in soft tissue and is usually seen in muscles or adipose tissue or non-muscle fibrous/connective tissue. HO can be genetic, such as Fibro-Dysplasia Ossificans Progressiva (FOP) and progressive osseous heteroplasia. Acquired forms of HO are seen mostly in Central Nervous System (CNS) injuries (Traumatic Brain Injury, Spinal Cord Injury), severe trauma, burns, and poliomyelitis, stroke and joint replacement surgeries. However, its presence in peripheral nerve disorders is extremely rare [1]. Its incidence following CNS trauma ranges from 13% and 57% and is usually seen in first six months after injury [2,3].
The cause of HO is still unknown. Contributing factors like vascular stasis, oedema, prolonged swelling, excessive passive manipulation, long term sedation and prolonged coma are suggested [4]. Heterotopic bone formation occurs predominantly around the hips, knees, shoulders and elbows and involves muscle groups like the quadriceps femoris, hip adductors, gluteal muscles, biceps of the arm and deltoid muscle [5].
The pathophysiology of HO remains unclear in both Upper Motor Neuron (UMN) and Lower Motor Neuron (LMN) lesions. Recent studies have shown that HO is associated with neuroinflammation and neural crest bone formation [6]. Bone Morphogenetic Proteins (BMP) are signalling factors which play a role in cell proliferation, apoptosis, differentiation and morphogenesis of nervous and musculoskeletal systems [7]. Trauma leads to damage of bone which releases BMPs, that opens the Blood-Nerve Barrier (BNB) which induces neuroinflammation in nerves in vicinity of the injury site [6]. Endoneurium contains neural crest stem cells and progenitors which are protected from external environment by BNB. As BNB opens, these cells along with BMPs and inflammatory cytokines are released in the blood. The BMPs in blood produce Brown Adipose Tissue (BAT) which promotes neoangiogenesis and hypoxic environment. This cascade of Neuro-inflammation, increased BMPs and BAT accelerates the neural crest stem cells to undergo osteogenic differentiation and causes HO [8].
Despite the perception that HO does not occur in peripheral nerve disorders, there have in fact been a number of case reports in various neurologic disorders, with no clear involvement of the CNS [9]. Acute inflammatory demyelinating polyneuropathy or GBS damages myelin sheath and axons. Since, it is an immune mediated reaction, there is altered BNB and increased production of BMP due to demyelination [10]. Although there is no trauma or bone fracture in GBS; peripheral nerve inflammation, immune mechanisms, elevated BMP and altered BNP leads to HO in GBS.
In the available literature, we found 17 reported cases of HO following GBS [Table/Fig-5] [4,9,11-20]. Zeilig G et al., reported 6% incidence of HO in GBS [9]. Ploumis A et al., reported less than 3% HO in GBS [11]. HO is most commonly seen in males (both the cases reported here). The mean age of HO in GBS as per reported cases was 42 years [16-20] while our cases were 20 years and 24-year-old. Hip joint was mostly affected in literature which is in concordance with our case report [12-17]. Risk factors reported were mechanical ventilation [4,12,15], prolonged immobilisation [4,12,15] and respiratory failure [9,15]. Both our cases were ventilated and had prolonged immobilisation while case no. 1 also had respiratory failure.
Reported cases of HO following GBS.
| Study | Number of cases | Average age and Gender | Risk factors | Joint affected |
|---|
| Ryu SR et al., [4] | 1 | 31 years, female | Mechanical ventilation, Prolonged immobilisation | Right hip joint |
| Zeilig G et al., [9] | 4 | 37.5 years mean age (range 34-59 years), 3 male and 1 female | Mechanical ventilation, Respiratory failure | 1 patient bilateral, 1 patient right and 2 patients left hip joint. |
| Vaishya R et al., [12] | 1 | 30 years, female | Mechanical ventilation, Prolonged immobilisation | Bilateral knee joints |
| Shawgi M [13] | 1 | 55 years, male | Prolonged immobilisation | Bilateral hip joints |
| Kerdoncuff V et al., [14] | 3 | Average age 42 years, male | Mechanical ventilation, Prolonged immobilisation, Encephalopathy | Bilateral shoulder, Knee and hip joints. One patient had compression of Ulnar nerve due to HO. |
| Ohnmar H et al., [15] | 1 | 39 years, male | Mechanical ventilation, Prolonged immobilisation, Respiratory failure | Bilateral shoulder, Elbow and hip joints |
| Bernard V [16] | 1 | 35 years, male | Prolonged immobilisation | Hand joints |
| Hung JCC et al., [17] | 1 | 13 years, male | Mechanical ventilation, Respiratory failure | Bilateral hip joints |
| Ploumis A et al., [11] | 1 | 67 years, male | Mechanical ventilation | Bilateral hip joints |
| Coppens E et al., [18] | 1 | 63 years, male | Mechanical ventilation, Prolonged immobilisation | Bilateral hip joints |
| Nalbantoglu M et al. [19] | 1 | 39 years, male | Mechanical ventilation, Prolonged immobilisation, Respiratory failure | Bilateral hip joints |
| Abid H et al., [20] | 1 | 42 years, female | Mechanical ventilation, Prolonged immobilisation, Respiratory failure | Bilateral hip joints |
HO: Heterotopic ossification; GBS: Guillain barre syndrome
Clinical Signs and Symptoms of HO develop within 4-12 weeks post-injury. It generally starts with the complaint of pain followed by stiffness/limitation in range of motion. Both the patients reported of hip pain and stiffness during passive joint mobilisation within 8 and 10 weeks of hospitalisation respectively. Diagnostically, simple radiograph with increased Alkaline Phosphatase is enough if the new bone is clearly visible. Only in a very early case of HO; MRI, triple phase bone scan and SPECT/CT [4,9,12,13] may be needed. We used only simple Radiograph in both these cases. Most studies used Serum Calcium and Serum Phosphate as supplementary lab investigations. Studies by Ryu SR et al., and Zeilig G et al., reported an increase in ALP which is the same in both these reported cases [4,9].
Treatment options consist of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) (mainly Indomethacin), Bisphoshonates (Etidronate Sodium and Alendronate), radiotherapy, surgical excision and Range of motion exercises within painless range. We used only NSAIDs and rehabilitation therapy in patients of the present study and they may be considered for surgery after re-evaluation.
Conclusion(s)
Both these cases are extremely rare cases of late onset HO after Guillain-Barre Syndrome. Long immobilisation and forceful joint mobilisation may cause HO by repetitive micro-trauma to muscles having flaccid paralysis, eventually leading to ectopic bone formation in soft tissues. Even though there are very few reported cases, physicians and healthcare professionals should be aware of this complication which has a huge effect on functional outcome of such patients.
HO: Heterotopic ossification; GBS: Guillain barre syndrome
[1]. George DH, Scheithauer BW, Spinner RJ, Buchler U, Cronin TE, Reedy MT, Heterotopic ossification of peripheral nerve (“neuritis ossificans”): Report of two casesNeurosurgery 2002 51(1):244-46.10.1097/00006123-200207000-0003912182426 [Google Scholar] [CrossRef] [PubMed]
[2]. Van Kuijk AA, Geurts AC, van Kuppevelt HJ, Neurogenic Heterotopic ossification in spinal cord injurySpinal Cord 2002 40(7):313-26.10.1038/sj.sc.310130912080459 [Google Scholar] [CrossRef] [PubMed]
[3]. Lal S, Hamilton BB, Heinemann A, Betts HB, Risk factors of heterotopic ossification in spinal cord injuryArch Phys Med Rehabil 1989 70(5):387-90. [Google Scholar]
[4]. Ryu SR, Kim JH, Choi IS, Han J-Y, Lee S-G, Heterotopic ossification as an unusual complication after Guillain-Barré syndrome: A case reportArch Phys Med Rehabil 2008 89(3):564-67.10.1016/j.apmr.2007.11.00418295638 [Google Scholar] [CrossRef] [PubMed]
[5]. Quek ST, Unger A, Cassar-Pullicinob VN, Roberts SNJ, A self-limiting tumourAnn Rheum Dis 2000 59(4):252-56.10.1136/ard.59.4.25210733470 [Google Scholar] [CrossRef] [PubMed]
[6]. Davis EL, Davis AR, Gugala Z, Olmsted-Davis EA, Is Heterotopic ossification getting nervous?: The role of the peripheral nervous system in heterotopic ossificationBone 2017 15:pii: S8756-3282(17)30242-49 [Google Scholar]
[7]. Hogan BL, Bone morphogenetic proteins: Multi-functional regulators of vertebrae developmentGenes Devop 1996 10(13):1580-94.10.1101/gad.10.13.15808682290 [Google Scholar] [CrossRef] [PubMed]
[8]. Huang H, Cheng WX, Hu YP, Chen JH, Zheng ZT, Zhang P, Relationship between heterotopic ossification and traumatic brain injury: Why severe traumatic brain injury increases the risk of heterotopic ossificationJ Orthop Translat 2017 12:16-25.10.1016/j.jot.2017.10.00229662775 [Google Scholar] [CrossRef] [PubMed]
[9]. Zeilig G, Weingarden HP, Levy R, Peer I, Ohry A, Blumen N, Heterotopic ossificationin Guillain-Barre syndrome: Incidence and effects on functional outcome with longterm follow-upArch Phys Med Rehabil 2006 87(1):92-95.10.1016/j.apmr.2005.07.30816401445 [Google Scholar] [CrossRef] [PubMed]
[10]. Willison HJ, Jacobs BC, van Doorn PA, Guillain-Barre syndromeLancet 2016 388(10045):717-27.10.1016/S0140-6736(16)00339-1 [Google Scholar] [CrossRef]
[11]. Ploumis A, Varvarousis D, Theodorou A, Gelalis I, Korompilias A, Pakos EE, Heterotopic ossification (HO) as a complication of Guillain-Barre syndrome (GBS): A case reportPhys Med Rehabil Res 2018 310.15761/PMRR.1000190 [Google Scholar] [CrossRef]
[12]. Vaishya R, Agarwal AK, Vijay V, Vaish A, Heterotopic Ossification Circumferentia Articularis (HOCA) of both knee joints After Guillain-Barre SyndromeCureus 2016 8(2):e48010.7759/cureus.480 [Google Scholar] [CrossRef]
[13]. Shawgi M, Heterotopic ossification of the hips in a patient with Guillain Barre syndrome demonstrated on SPECT/CTClin Nucl Med 2012 37(10):e253-54.10.1097/RLU.0b013e318248523322899193 [Google Scholar] [CrossRef] [PubMed]
[14]. Kerdoncuff V, Sauleau P, Petrilli S, Duruflé A, Ben Beroukh K, Brissot R, Heterotopic ossification in Guillain-Barre syndromeAnn Readapt Med Phys 2002 45(5):198-203.10.1016/S0168-6054(02)00203-9 [Google Scholar] [CrossRef]
[15]. Ohnmar H, Roohi SA, Naicker AS, Massive heterotopic ossification in Guillain-Barre syndrome: A rare case reportClin Ter 2010 161:529-32.10.15761/PMRR.1000190 [Google Scholar] [CrossRef]
[16]. Bernard V, Para-ostéo-arthropathies des deux mains compliquant un syndrome de Guillain-Barré Heterotopic ossification of the hands in a patient with Guillain-Barré syndromeAnn Réadapt Med Phys 1998 41:85-88.10.1016/S0168-6054(97)87445-4 [Google Scholar] [CrossRef]
[17]. Hung Jcc, Appleton RE, Abernethy L, Myositis ossificans complicating severe Guillain-Barré syndromeDev Med Child Neurol 1997 39(11):775-76.10.1111/j.1469-8749.1997.tb07382.x9393894 [Google Scholar] [CrossRef] [PubMed]
[18]. Coppens E, Kassouha A, Amzalag G, Schnider A, Leemann B, Heterotopic Ossification: A Rare Complication in Guillain-Barré SyndromeJ J Physical Rehab Med 2015 1(4):018 [Google Scholar]
[19]. Nalbantoglu M, Tuncer OG, Acık ME, Matur Z, Altunrende B, Ozgonenel E, Neurogenic heterotopic ossification in Guillain-Barre syndrome: A rare case reportJ Musculoskelet Neuronal Interact 2020 20(1):160-64.PMID: 32131381; PMCID: PMC7104584 [Google Scholar]
[20]. Abid H, El Idrissi M, Shimi M, El Ibrahimi A, El Mrini A, Neurogenic osteoarthritis in Guillain Barre syndrome: A rare complication (case report and review of the literature)Pan Afr Med J 2015 20:24510.11604/pamj.2015.20.245.314326161168 [Google Scholar] [CrossRef] [PubMed]