Venous Thromboembolism Prophylaxis in Medical Intensive Care Unit: An Audit
Basant Kumar Pathak1, P Harikrishnan2, Manish Manrai3
1 Assistant Professor, Department of Internal Medicine, Armed Forces Medical College, Pune, Maharashtra, India.
2 Junior Resident, Department of Internal Medicine, Armed Forces Medical College, Pune, Maharashtra, India.
3 Associate Professor, Department of Internal Medicine, Armed Forces Medical College, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manish Manrai, Associate Professor, Department of Internal Medicine, Armed Forces Medical College, Pune-411040, Maharashtra, India.
E-mail: manishmanrai@yahoo.com
Introduction
Venous Thromboembolism (VTE) is a major cause of morbidity and mortality in patients admitted to healthcare facilities. This can be prevented by giving thromboprophylaxis to patients after assessing the risk for VTE. This however is not being routinely done leading to underuse of thromboprophylaxis due to inadequate practice of risk assessment.
Aim
To conduct an audit of VTE prophylaxis in Intensive Care Unit (ICU) based on Padua score and International Medical Prevention Registry on Venous Thromboembolism (IMPROVE) Risk Assessment Model (VTE RAM).
Materials and Methods
This was a cross-sectional observational study and the data was collected from medical records of patients retrospectively who were admitted to medical ICU between October 2019 and December 2019. Based on medical records risk assessment was done using the Padua score and IMPROVE VTE RAM. The prophylaxis given to patients was scrutinised for appropriateness based on American Society of Haematology (ASH) guidelines. The two validated scores Padua score and IMPROVE VTE RAM were compared with each other for any significant difference in the risk assessment made using Chi-square test and p-value <0.05 were considered significant.
Results
Out of the 176 patients risk assessment was not done in any patient. On calculating the Padua score, 149 patients (84.66%) were in high risk for VTE (Padua Score ≥4) and amongst them only 76 (51%) patients received thromboprophylaxis. On calculating the IMPROVE VTE RAM score, 137 patients (77.84%) were in moderate or high risk for VTE requiring prophylaxis and amongst them only 76 (55.47%) patients received thromboprophylaxis. The accuracy of clinician’s judgement without risk assessment was 58.52% (95% CI: 65.80%-51.24%) and 64.20% (95% CI: 71.28%-57.12%) as compared to risk assessment by Padua score and IMPROVE VTE RAM, respectively. There was no significant difference between IMPROVE VTE RAM and Padua score with respect to risk assessment for VTE (p-value of 0.10).
Conclusion
The practice of VTE prophylaxis is grossly inadequate and there is a requirement to sensitise the healthcare providers about the importance of risk assessment for VTE.
American society of haematology, Padua score, Pulmonary embolism
Introduction
Venous Thromboembolism (VTE) is a major cause of morbidity and mortality in patients admitted to healthcare facilities [1]. The incidence of VTE in hospitalised patients as evidenced by autopsy studies is as high as 34.7% with fatal Pulmonary Embolism (PE) in 9.4% of cases [2]. PE is responsible for 5-10% of death in hospitalised patients, making VTE the most common avoidable cause of in-hospital death [3]. Critical patients are at a higher risk of developing VTE and thus require immediate risk assessment and prophylaxis for VTE wherever indicated [4]. The risk of developing VTE can be as high as 81% in critically ill patients without thromboprophylaxis and it reduces to 44% with thromboprophylaxis [5]. There are multiple guidelines to help clinicians decide whether a patient requires prophylaxis for VTE. Multiple risk assessment tools are available and the choice of prophylaxis to be given to patients is also varied which leads to inappropriate management of patients as far as VTE prophylaxis is concerned. The most validated tools for risk assessment are Padua score [6] and IMPROVE VTE RAM [7]. Bleeding risk can be assessed by using IMPROVE bleeding score [8]. These scores have been extensively validated. The choice of thromboprophylaxis is varied and various guidelines including the American College of Chest Physicians (ACCP) 2016 [9] and ASH guidelines 2018 [10] recommend using Low Molecular Weight Heparin (LMWH) in critically ill medical patients. If the treating physician perceives a high risk of bleed, then mechanical thromboprophylaxis can be used. Patients not receiving appropriate prophylaxis can develop life threatening complications like pulmonary thromboembolism and patients who are inappropriately given anticoagulation can develop catastrophic complications like intracerebral haemorrhage. Despite the extensive evidence of benefit of VTE prophylaxis almost 71% patients do not receive appropriate prophylaxis [11].
This study aims to assess the appropriateness of VTE prophylaxis practices in a medical ICU of a tertiary care hospital. The two validated scores Padua score and IMPROVE VTE RAM were compared with each other for any significant difference in the risk assessment made using them. Assessing this will help us find out the gaps and improve our management of patients in future as far as VTE prophylaxis is concerned.
Materials and Methods
This was a cross-sectional observational study and the data was collected from medical records of patients. Records of all patients who were admitted to medical ICU in a tertiary care hospital from October 2019 to December 2019 were included in the study. Ethical clearance was obtained for the present study from Institutional Ethical Committee (IEC No. IEC/2019/267). Patients with an ICU stay of less than 48 hours or already on anti-coagulation were excluded from the study. The details of each patient were taken from the medical records. This included their age, sex, current illness, other co-morbidities and whether risk assessment was done for VTE. Based on medical records risk assessment was done using the Padua score [6] and IMPROVE VTE RAM [7]. The bleeding risk was calculated using the IMPROVE Bleeding risk score [8]. The data required for calculating the above scores were taken from medical records and based on the validated risk assessment scoring the respective scores were calculated. The prophylaxis given to patients was scrutinised for appropriateness based on ASH guidelines [10].
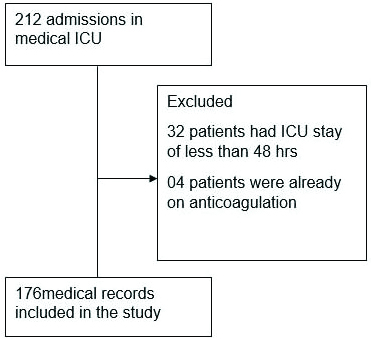
A total of 212 admissions took place in medical ICU of the hospital from 01st October 2019 to 31st December 2019. Amongst these 36 were excluded from the study, 32 patients either died within 48 hours of admission or were transferred to other wards in view of improved general condition. A total of 04 patients were already on anti-coagulation. Total 176 medical records were included in this study [Table/Fig-1].
Flow chart of recruitment of patients.
Statistical Analysis
The results were computed using Microsoft Excel. The continuous variables were described using mean and Standard Deviation (SD). The categorical variables were analysed using number and percentages with 95% confidence interval. The statistical analysis for difference between risk assessments based on Padua score and IMPROVE VTE RAM was calculated by Chi-square test and p-value <0.05 were considered significant.
Results
Patient Characteristics
The mean age of patients was 61.65 (±16.8) years. There were 115 male patients and 61 female patients (M:F ratio of 1.89). Only 3 patients (1.7%) had Body Mass Index (BMI) recorded out of 176 patients. The major contributors to ICU admission were Cerebrovascular Accident (CVA) (22.73%; 95% CI: 28.91%-16.53%) and Pneumonia (10.23%; 95% CI: 14.70%-05.75 [Table/Fig-2]. Primary Hypertension (53.40%; 95% CI: 60.77%-40.03%) and Type 2 Diabetes Mellitus (36.36%; 95% CI: 43.47%-29.25%) were the most common co-morbidities in these patients [Table/Fig-3].
Major diseases contributing to admissions in medical ICU.
| Diagnosis | Number of patients | Percentage (N=176) |
|---|
| Cerebrovascular accident | 40 | 22.73% (95% CI: 28.91%-16.53%) |
| Pneumonia | 18 | 10.23% (95% CI: 14.70%-05.75%) |
| Malignancy | 16 | 9.09% (95% CI: 13.33%-04.84%) |
| Chronic liver disease | 11 | 6.25% (95% CI: 9.82%-2.67%) |
| Other diseases | 91 | 51.70% (95% CI: 59.08%-44.32%) |
Common co-morbidities in patients admitted to medical ICU.
| Co-morbidities | Number of patients* | Percentage (N=176) |
|---|
| Primary hypertension | 94 | 53.40% (95% CI: 60.77%-40.03%) |
| Type 2 diabetes mellitus | 64 | 36.36% (95% CI: 43.47%-29.25%) |
| Chronic kidney disease | 15 | 8.52% (95% CI: 12.64%-04.39%) |
| Coronary artery disease | 14 | 7.95% (95% CI: 11.95%-03.95%) |
| Cerebrovascular accident | 09 | 5.11% (95% CI: 08.36%-01.85%) |
*Many patients had more than one co-morbidity
Risk Assessment for VTE
Out of the 176 patients appropriate risk assessment was not done in any patient.
Padua Score
On calculating the Padua score 149 patients (84.66%; 95% CI: 89.98%-79.33%) were in high risk for VTE (Padua Score ≥4) and 27 patients were (15.34%; 95 % CI: 10.01%-20.66%) in low risk for VTE.
IMPROVE VTE RAM
Based on IMPROVE VTE RAM 39 patients (22.16%; 95% CI: 28.29%-16.02%) were in low risk (Score of 0 or 1), 94 (53.41%; 95% CI: 60.77%-46.03%) in moderate risk (Score of 2 or 3) and 43 (24.43%; 95% CI: 30.77%-18.08%) in high risk (Score equal to or more than 4) for VTE thus prophylaxis was indicated in 137 patients (Moderate and high risk) (77.84%; 95% CI: 83.97%-71.70%).
VTE Prophylaxis
Prophylaxis was given in a total of 76 patients out of which 09 received unfractionated heparin in view of renal involvement and rest all patients received LMWH. Mechanical prophylaxis was not given to any patient.
The sensitivity of clinician’s judgement as compared to Padua score in assessing the requirement of thromboprophylaxis in a patient was 51% and the specificity was 100%. Positive Predictive Value and Negative Predictive Value (NPV) of clinician’s judgement as compared to Padua score in assessing the requirement of thromboprophylaxis in patients were 100% and 27%, respectively. Accuracy of clinician’s judgement was 58.52% as compared to Padua score in assessing requirement of thromboprophylaxis in patients [Table/Fig-4].
Clinician’s judgement as compared to Padua score in assessing risk for VTE.
| Prescribed thromboprophylaxis by clinician based on clinical judgement | Risk assessment as per Padua score |
|---|
| High risk | Low risk |
|---|
| Yes | 76 | 00 |
| No | 73 | 27 |
| Sensitivity of clinician’s judgement without risk assessment | 51% (95% CI: 59.03%-42.98%) |
| Specificity of clinician’s judgement without risk assessment | 100% |
| Positive predictive value | 100% |
| Negative predictive value | 27% (95% CI: 35.07%-18.29%) |
| Accuracy | 58.52% (95% CI: 65.80%-51.24%) |
The sensitivity of clinician’s judgement as compared to IMPROVE VTE RAM in assessing the requirement of thromboprophylaxis in a patient was 55.47%. PPV and NPV of clinician’s judgement as compared to IMPROVE VTE RAM in assessing the requirement of thromboprophylaxis in patients were 97.43% and 37.75%, respectively [Table/Fig-5].
Clinician’s judgement as compared to IMPROVE VTE RAM in assessing risk for VTE.
| Prescribed thromboprophylaxis by clinician based on clinical judgement | Risk assessment as per IMPROVE VTE RAM |
|---|
| Moderate and high risk | Low risk |
|---|
| Yes | 76 | 02 |
| No | 61 | 37 |
| Sensitivity of clinician’s judgement without risk assessment | 55.47% (95% CI: 63.79%-47.15%) |
| Specificity of clinician’s judgement without risk assessment | 94.87% (95% CI: 100%-87.94%) |
| Positive predictive value | 97.43% (95% CI: 100%-93.09%) |
| Negative predictive value | 37.75% (95% CI: 47.35%-28.15%) |
| Accuracy | 64.20% (95% CI: 71.28%-57.12%) |
Difference in number of patients in whom thromboprophylaxis was indicated as per IMPROVE VTE RAM and as per Padua RAM was not significant (p-value=0.10) [Table/Fig-6].
Risk assessment based on IMPROVE VTE RAM versus Padua score.
| Requires thromboprophylaxis | Does not require thromboprophylaxis | Grand total |
|---|
| Padua RAM | 149 | 27 | 176 |
| IMPROVE VTE RAM | 137 | 39 | 176 |
| p-value=0.10 using chi-square test |
IMPROVE Bleeding Risk
There was high risk of bleeding in 91 patients (51.7%; 95% CI: 59.08%-44.32%) as assessed by IMPROVE bleeding risk score and incidence of major bleeding was 05 in high risk patients and 02 in low risk patients however none of the bleeding episode was related to anticoagulation. No episode of VTE was recorded in any patient.
Bleeding Episodes
Seven (3.97%; 95% CI: 06.86%-01.09%) patients had bleeding episodes but none was related to anticoagulation rather they were part of patient’s primary diagnosis (Four patients with intracerebral haemorrhage due to CVA, one patient with Upper Gastrointestinal (UGI) bled due to duodenal ulcer, one patient with UGI bleed due to Immune Thrombocytopenic Purpura (ITP) and one patient with UGI bleed due to esophageal varices).
Discussion
Majority of critical medical patients are elderly; in present study the mean age was 61.65 (±16.8) years. These patients are at a higher risk of thromboembolism as well as bleed thus these patients must be assessed appropriately for the need of thromboprophylaxis. Only three patients had BMI recorded in medical documents likely due to inability to take weight in bed bound patients in a critical care environment.
In this study, none of the patients have been assessed for risk of VTE using any validated tool. There were 149 (84.65%; 95% CI: 89.98%-79.33%) patients in high risk as per Padua score however only 76 out of the 149 patients in high risk (51%; 95% CI: 59.03%-42.98%) were given thromboprophylaxis based on overall clinical impression of treating physician. A total of 73 patients who were in high risk of VTE as per Padua score and 61 patients who were either moderate or high risk for VTE as per IMPROVE VTE RAM score did not receive any thromboprophylaxis. The clinician has however not prescribed thromboprophylaxis to any patient in low risk of VTE as per Padua score. This reflects the fact that we have missed many high-risk patients who required thromboprophylaxis. The accuracy of clinicians judgement as compared to validated risk assessment tools have been just above 50% {58.52% (95% CI: 65.80%-51.24%) as per Padua score and 64.20% (95% CI: 71.28%-57.12%) as per IMPROVE VTE RAM} which is grossly inadequate, emphasising the need to assess each medical patient using a validated tool for risk of VTE as early as possible after admission to a critical care setting. Similar findings were seen in ENDORSE study in which only 39.5% of total medical patients in high risk for VTE received any thromboprophylaxis. In the same study, Indian data showed that only 17.4% of the total high-risk patients received thromboprophylaxis [3]. Another study by Parikh KC et al., revealed that 20% of patients requiring thromboprophylaxis did not receive it [12]. These findings emphasise the fact that risk assessment is of utmost importance and must be practiced by all critical care physicians.
There is limited data on comparison between IMPROVE VTE RAM and Padua score for VTE risk assessment however in this study difference in number of patients in whom thromboprophylaxis was indicated as per IMPROVE VTE RAM and as per Padua RAM was not significant (p-value=0.1). This emphasises the fact that both risk assessment tools are equivalent in assessing risk for VTE. The consensus on management of deep vein thrombosis by association of physicians of India recommends the use of Padua score for risk assessment in medical patients [13]. Irrespective of the risk assessment tool used, the practice of thromboprophylaxis will improve if we follow any validated risk assessment tool to decide whether a patient requires thromboprophylaxis for VTE.
The bleeding risk was high in 51.7% (95% CI: 59.08%-44.32%) patients in this study as compared to 13% patients in the STIME study which is likely due the clinical profile of ICU medical patients who have multiple co-morbidities and are on multiple drugs making them vulnerable to bleeding episodes. In STIME study, all patients admitted to a medical unit were assessed and not only ICU patients [14].
Limitation(s)
Obesity is one of the risk factors for VTE [15] and this factor could not be added in present study patients in view of non-availability of data; if the BMI would have been available than the number of high-risk cases might have been higher using the Padua score. No VTE episodes were recorded in present study however in view of limited follow-up of patients due to paucity of medical records and relatively small sample size this should not be interpreted as reduced risk of VTE in these critically ill patients. This data was taken from a single centre and thus large scale data from multiple hospitals will help us understand the problem better.
Conclusion(s)
Critically ill medical patients are at high risk of VTE as well as bleeding episodes and thus appropriate prophylaxis is of utmost importance which is not being practiced in critical care settings. There is a need to sensitise the healthcare providers about the importance of risk assessment for VTE and bleeding in all critical care patients using any validated risk assessment tool. This will go a long way in preventing morbidity and mortality in the patients.
*Many patients had more than one co-morbidity
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? No
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 22, 2020
Manual Googling: Dec 07, 2020
iThenticate Software: Dec 17, 2020 (14%)
[1]. Heit JA, Melton LJ, Lohse CM, Petterson TM, Silverstein MD, Mohr DN, Incidence of venous thromboembolism in hospitalised patients vs community residentsMayo Clin Proc 2001 76(11):1102-10.Available from: https://pubmed.ncbi.nlm.nih.gov/11702898/10.4065/76.11.110211702898 [Google Scholar] [CrossRef] [PubMed]
[2]. Agarwal S, Lee A, Raju R, Stephen E, Venous thromboembolism: A problem in the Indian/Asian population?Indian J Urol 2009 25(1):11Available from: http://www.indianjurol.com/text.asp?2009/25/1/11/4553110.4103/0970-1591.4553119468423 [Google Scholar] [CrossRef] [PubMed]
[3]. Cohen AT, Tapson VF, Bergmann JF, Goldhaber SZ, Kakkar AK, Deslandes B, Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): A multinational cross-sectional studyLancet 2008 371(9610):387-94.Available from: https://pubmed.ncbi.nlm.nih.gov/18242412/10.1016/S0140-6736(08)60202-0 [Google Scholar] [CrossRef]
[4]. Boonyawat K, Crowther MA, Venous thromboembolism prophylaxis in critically ill patientsSemin Thromb Hemost 2015 41(1):68-74.Available from: https://pubmed.ncbi.nlm.nih.gov/25594495/10.1055/s-0034-139838625594495 [Google Scholar] [CrossRef] [PubMed]
[5]. Attia J, Ray JG, Cook DJ, Douketis J, Ginsberg JS, Geerts WH, Deep vein thrombosis and its prevention in critically ill adults. Vol. 161, Archives of Internal MedicineAmerican Medical Association 2001 :1268-79.Available from: https://pubmed.ncbi.nlm.nih.gov/11371254/10.1001/archinte.161.10.126811371254 [Google Scholar] [CrossRef] [PubMed]
[6]. Barbar S, Noventa F, Rossetto V, Ferrari A, Brandolin B, Perlati M, A risk assessment model for the identification of hospitalised medical patients at risk for venous thromboembolism: The Padua Prediction ScoreJ Thromb Haemost 2010 8(11):2450-57.Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/j.1538-7836.2010.04044.x10.1111/j.1538-7836.2010.04044.x20738765 [Google Scholar] [CrossRef] [PubMed]
[7]. Mahan CE, Liu Y, Graham Turpie A, Vu JT, Heddle N, Cook RJ, External validation of a risk assessment model for venous thromboembolism in the hospitalised acutely-ill medical patient (VTE-VALOURR)Thromb Haemost 2014 112(4):692-99.Available from: https://pubmed.ncbi.nlm.nih.gov/24990708/10.1160/TH14-03-023924990708 [Google Scholar] [CrossRef] [PubMed]
[8]. Rosenberg DJ, Press A, Fishbein J, Lesser M, McCullagh L, McGinn T, External validation of the IMPROVE Bleeding Risk Assessment Model in medical patientsStroke, Systemic or Venous Thromboembolism 2016 [cited 2020 Jul 11]; Available from: www.thrombosis-online.com [Google Scholar]
[9]. Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, Antithrombotic therapy for VTE disease: CHEST guideline and expert panel reportChest 2016 149(2):315-52.Available from: https://pubmed.ncbi.nlm.nih.gov/26867832/10.1016/j.chest.2015.11.02626867832 [Google Scholar] [CrossRef] [PubMed]
[10]. Schünemann HJ, Cushman M, Burnett AE, Kahn SR, Beyer-Westendorf J, Spencer FA, American Society of Haematology 2018 guidelines for management of venous thromboembolism: Prophylaxis for hospitalised and nonhospitalised medical patients [Internet]. Vol. 2Blood Advances. American Society of Haematology 2018 :3198-225.Available from: https://pubmed.ncbi.nlm.nih.gov/30482763/10.1182/bloodadvances.201802295430482763 [Google Scholar] [CrossRef] [PubMed]
[11]. Rashid ST, Thursz MR, Razvi NA, Voller R, Orchard T, Rashid ST, Venous thromboprophylaxis in UK medical inpatientsJ R Soc Med 2005 98(11):507-12.Available from: /pmc/articles/PMC1275999/?report=abstract10.1177/01410768050980111216260800 [Google Scholar] [CrossRef] [PubMed]
[12]. Parikh KC, Oh D, Sittipunt C, Kalim H, Ullah S, Aggarwal SK, Venous thromboembolism prophylaxis in medical ICU patients in Asia (VOICE Asia): A multicenter, observational, cross-sectional studyThromb Res 2012 129(4)Available from: https://pubmed.ncbi.nlm.nih.gov/22326367/10.1016/j.thromres.2012.01.01222326367 [Google Scholar] [CrossRef] [PubMed]
[13]. Pinjala PK, Parakh R, Consensus on management of DVT with emphasis on NOACs: Recommendations from inter-disciplinary group of Indian expertsJ Assoc Physicians India 2016 64(9 Suppl):6Available from: http://www.ncbi.nlm.nih.gov/pubmed/28825230 [Google Scholar]
[14]. Depietri L, Marietta M, Scarlini S, Marcacci M, Corradini E, Pietrangelo A, Clinical impact of application of risk assessment models (Padua Prediction Score and Improve Bleeding Score) on venous thromboembolism, major hemorrhage and health expenditure associated with pharmacologic VTE prophylaxis: A “real life” prospective and retrospective observational study on patients hospitalised in a Single Internal Medicine Unit (the STIME study)Intern Emerg Med] 2018 13(4):527-34.Available from: https://pubmed.ncbi.nlm.nih.gov/29502330/10.1007/s11739-018-1808-z29502330 [Google Scholar] [CrossRef] [PubMed]
[15]. Anderson FA, Risk factors for venous thromboembolismCirculation 2003 107(90231):9I-16.Available from: http://circ.ahajournals.org/cgi/doi/10.1161/01.CIR.0000078469.07362.E610.1161/01.CIR.0000078469.07362.E6 [Google Scholar] [CrossRef]