Delayed Infection of an Autopolymerising Acrylic Resin Implanted for Orbital Floor Reconstruction
Satomi Sugiyama1, Toshinori Iwai2, Taro Mikami3, Jiro Maegawa4
1 Doctor, Department of Oral and Maxillofacial Surgery/Orthodontics, Yokohama City University Hospital, Yokohama, Kanagawa, Japan.
2 Doctor, Department of Oral and Maxillofacial Surgery/Orthodontics, Yokohama City University Hospital, Yokohama, Kanagawa, Japan.
3 Doctor, Department of Plastic and Reconstructive Surgery, Chigasaki Municipal Hospital, Chigasaki, Kanagawa, Japan.
4 Professor, Department of Plastic and Reconstructive Surgery, Yokohama City University Hospital, Yokohama, Kangawaka, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Toshinori Iwai, 3-9 Fukuura Kanazawa-ku, Yokohama, Kanagawa, Japan.
E-mail: iwai104oams@yahoo.co.jp
Complication, Cutaneous sinus tract, Orbit reconstruction
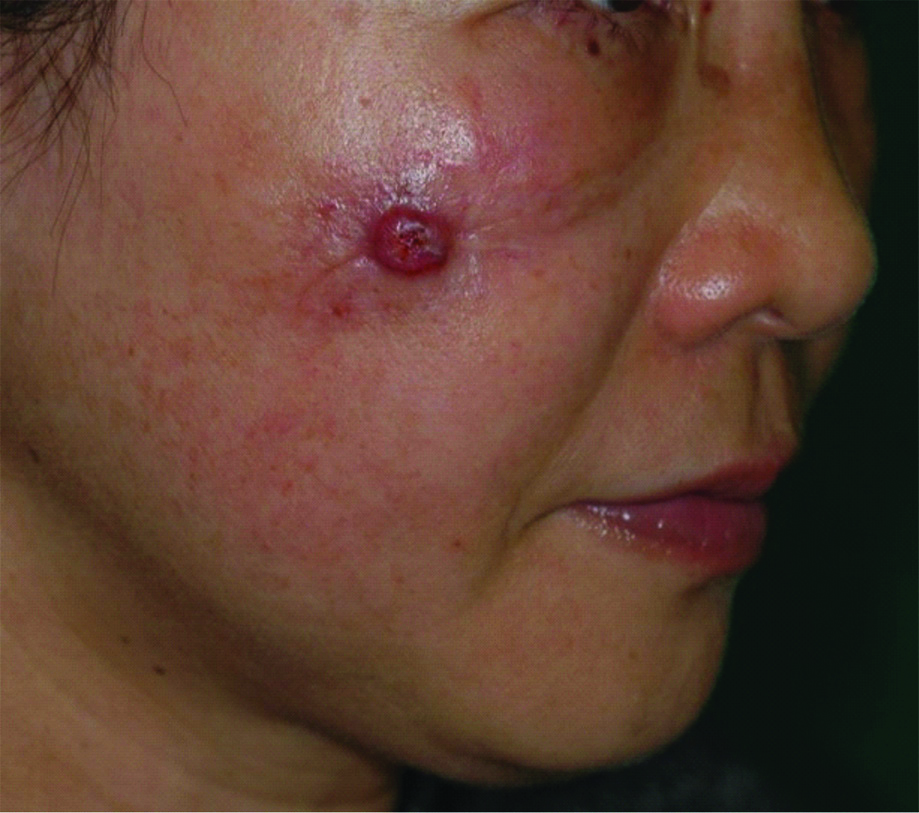
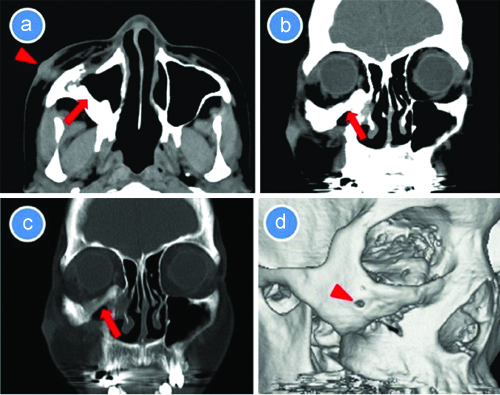
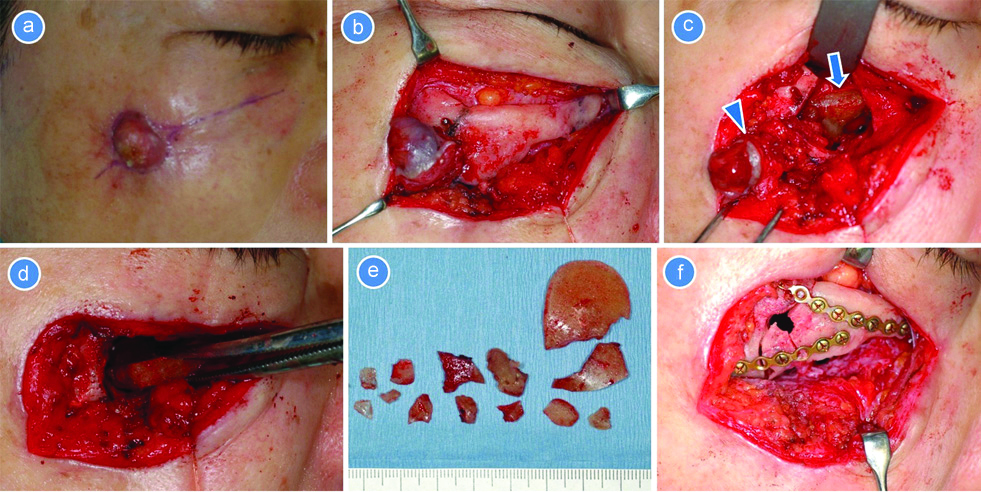
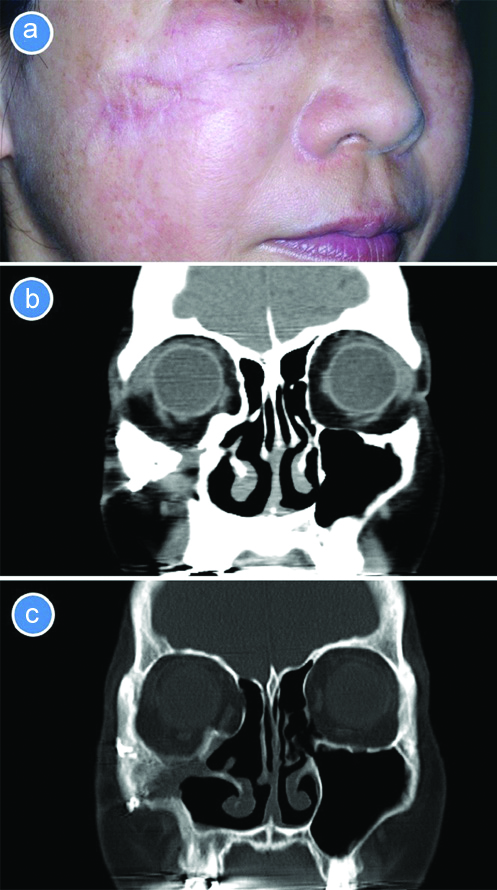
A 52-year-old woman with a chief compliant of pus discharge from the right cheek was referred to Department of Plastic and Reconstructive Surgery. Although she had a two years history of cutaneous sinus tract and purulent discharge from the right cheek, there was no pain and swelling [Table/Fig-1]. There was no previous medical history. She had right facial injury by a traffic accident 33 years ago, and was diagnosed with right zygomatic and orbital floor fracture. Therefore, she underwent open reduction and internal fixation of the zygomatic fracture and orbital floor reconstruction with an autopolymerising acrylic resin. One year after the surgery, only plate removal of the infraorbital rim and zygomaticomaxillary buttress was performed. Computed Tomography (CT) showed the resin in the orbit and cutaneous sinus tract, and the right maxillary sinus was clear [Table/Fig-2a-c], and three-dimensional CT revealed bone resorption caused by the sinus tract [Table/Fig-2d]. Clinical and radiological diagnosis was delayed infection of the resin implant. Antibiotics were not administrated preoperatively for continuous purulent discharge caused by chronic infection. As the informed consent was obtained from the patient, she underwent removal of the infected resin and cutaneous sinus tract under general anesthesia two weeks after the first visit. A skin incision was made on the scar of the cheek, and a cutaneous fistula penetrated the zygoma [Table/Fig-3a,b]. The resin was fragmented and removed completely after inferior orbitotomy for access to the orbit [Table/Fig-3c-e]. The fibrous union was strong enough to support the globe. The inferior orbital rim was replaced and fixed with titanium miniplates [Table/Fig-3f]. After haemostasis and saline irrigation with a syringe, the wound was closed with resorbable suture (VICRYL®, Ethicon part of Johnson & Johnson Family of Companies) and nylon suture (ETHILON®, Ethicon part of Johnson & Johnson Family of Companies). After that, Cefazolin (CEZ, 2 g/day) was administrated intravenously for three days; Cefdinir (CFDN, 300 mg/day) was administrated intraorally for three days. Postoperative assessments using Hess chart and Hertel exophthalmometer were performed, and there were no complications such as infection, diplopia, enophthalmos, and globe dysfunction. On follow-up, there was no recurrence of infection one and a half years after surgery [Table/Fig-4a-c].
Facial view shows a cutaneous sinus tract of the right cheek.
Computed tomography shows a resin (arrow) in the orbit. a) Axial image. Arrow indicates cutaneous sinus tract; b) Coronal image (soft tissue window); c) Coronal image (bone window); d): 3D image. Arrow head indicates bone resorption caused by sinus tract.
Surgical view. a) A skin incision was made on the scar of the cheek; b) a cutaneous fistula penetrated the zygoma; c) After inferior orbitotomy, resin (arrow head) was exposed. Arrow indicates a cutaneous sinus tract; d) Resin was removed by forceps; e) Removed resin; f) Plate fixation of the bony fragment.
Follow-up image one and a half years after surgery. Facial view (a) and CT (b,c).
Orbital implants are commonly used to repair orbital floor fracture. Complications after orbital floor reconstruction with alloplastic implants are well known, but it is not widely recognised that these can occur many years after the initial surgery. As delayed complications, orbital abscess or cellulitis, purulent discharge, diplopia, lower lid retraction, and extrusion of alloplastic implants have been reported [1-7].
Orbital reconstruction for orbital floor fracture is commonly performed with resorbable or alloplastic materials as well as autologous tissues (bone or cartilage). Although the complications sometimes occur, delayed infection of orbital implants is rare [1-6]. As a complication, osteomyelitis following delayed infection of orbital implants was reported by Suh SY et al., [1]. To our knowledge, the delayed infection has occurred 4 to 30 years after orbital reconstruction in English literature [1,3-7], whereas the present case had the most delayed infection i.e, 31 years after the orbital reconstruction with a resin implant. Alloplastic materials that caused the delayed infection, polytetrafluoroethylene [4], porous polyethylene [1,7], hydroxyapatite [3], silicone [2,5,6] were previously reported. Although it was reported that the cause of the delayed infection was the migration of alloplastic materials to the maxillary sinus [4] or the infratemporal fossa [6], the cause is unclear in some cases. Surgical removal of the orbital implant can lead to resolution of symptoms [2].
Although the resin implant did not extrude and did not contact the skin in the present case, delayed infection of orbital floor implant caused cutaneous sinus tract and purulent discharge. However, the cause of the infection which occurred 31 years after orbital reconstruction was unclear, because there were no migration of orbital implant and maxillary sinusitis.
Many complications may arise from the implants used for orbital floor reconstruction. Thus, the surgeons should consider the potential risk of delayed infection of the orbital implant and it should be removed immediately to prevent the infection from spreading.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 22, 2020
Manual Googling: Oct 14, 2020
iThenticate Software: Dec 17, 2020 (8%)
[1]. Suh SY, Yeom JA, Ahn JH, Porous polyethylene implant associated with delayed orbital complications and osteomyelitis after orbital reconstructionJ Craniofac Surg 2018 29:1910-11.10.1097/SCS.000000000000498530192296 [Google Scholar] [CrossRef] [PubMed]
[2]. Warrier S, Prabhakaran VC, Davis G, Selva D, Delayed complications of silicone implants used in orbital fracture repairsOrbit 2008 27:147-51.10.1080/0167683080207761118569817 [Google Scholar] [CrossRef] [PubMed]
[3]. Yeh LK, Kao SC, Tsai CC, Hsu WM, Liu JH, Delayed-onset of Pseudomonas infection in a hydroxyapatite orbital implant: A case reportZhonghua Yi Xue Za Zhi (Taipei) 1999 62:832-37. [Google Scholar]
[4]. Weintraub B, Cucin RL, Jacobs M, Extrusion of an infected orbital-floor prosthesis after 15 yearsPlast Reconstr Surg 1981 68:586-87.10.1097/00006534-198110000-000187025062 [Google Scholar] [CrossRef] [PubMed]
[5]. Brown AE, Banks P, Late extrusion of alloplastic orbital floor implantsBr J Oral Maxillofac Surg 1993 31:154-57.10.1016/0266-4356(93)90114-C [Google Scholar] [CrossRef]
[6]. Nitsche T, Yousefpour A, Bainton R, Chronic orbital infection caused by migration of an orbital Silastic implantInt J Oral Maxillofac Surg 2008 37:90-92.10.1016/j.ijom.2007.07.02217825528 [Google Scholar] [CrossRef] [PubMed]
[7]. Lee CA, Kang SJ, Yun JY, Sun H, Late complication of a silicone implant thirty years after orbital fracture reconstructionArch Craniofac Surg 2017 18:137-40.10.7181/acfs.2017.18.2.13728913322 [Google Scholar] [CrossRef] [PubMed]