Securing the airway with an endotracheal tube is an important skill in the practice of anaesthesia. Inability to secure an airway is one of the important causes of anaesthesia related mortalities [1]. Videolaryngoscopes have come handy in unanticipated difficult airway scenarios. They have combined features of classic laryngoscopes and fiberoptic technology to improve visualisation of the glottis and increased intubation success rates [2]. Videolaryngoscopes utilise the features of indirect laryngoscopy through its camera and projects the view of glottic structures through an eye piece or to an external monitor. This improves the glottic visualisation with application of less force to the base of the tongue. Thereby, Videolaryngoscopes produce lesser trauma and lesser stress response to intubation [3]. Channeled videolaryngoscopes like airtraq and Pentax AWS cause lesser cervical movement than direct laryngoscopy [4].
The C-MAC (Karl- Storz Endoscopy, Tuttligen, Germany) and airtraq (Prodol Meditec S.A, Vizcaya, Spain) are the Videolaryngoscopes of interest in this study. The C-MAC comprises of a standard MacIntosh blade and a curved D-blade connected to a video unit to which images are transmitted from a distal lens placed two thirds of the way along the blade. The Airtraq Videolaryngoscope has two channels, one of which transfers the image to a proximal viewfinder via a series of prisms and lenses, the other channel acts a conduit for the tracheal tube. The video image can be projected to an external monitor too [3]. Airtraq laryngoscopes can also be nonchanneled. Various clinical trials have been carried out to find out the efficiency of one videolaryngoscope over the other [5-8]. But no videolaryngoscope has shown 100% intubation success rate.
This study was designed to compare the efficacy of C-MAC D-blade and channeled Airtraq for successful intubation in patients with simulated Manual In-Line Stabilisation (MILS). The primary outcomes were the time taken for tracheal tube placement and the quality of laryngoscopy assessed by Cormack Lehane grading between Airtraq Videolaryngoscope and C-MAC D-blade. The secondary outcomes were to assess the need for external laryngeal maneuvers, the need for airway adjuncts like stylets or bougies and to monitor and compare the haemodynamic parameters like heart rate and mean arterial pressure.
Materials and Methods
This randomised clinical trial was conducted in Pondicherry Institute of Medical Sciences, Pondicherry (CTRI REF/2017/11/016113). A total of 116 patients were included in the study after obtaining Institutional Ethics Committee approval (RC/16/98).
Sample size was calculated using Mann-Whitney U test, probability of observing X>Y 0.65 allocation ratio as 01:01, power 80%, alpha error 5%, ½ sided test-2; which was calculated to be 116 samples.
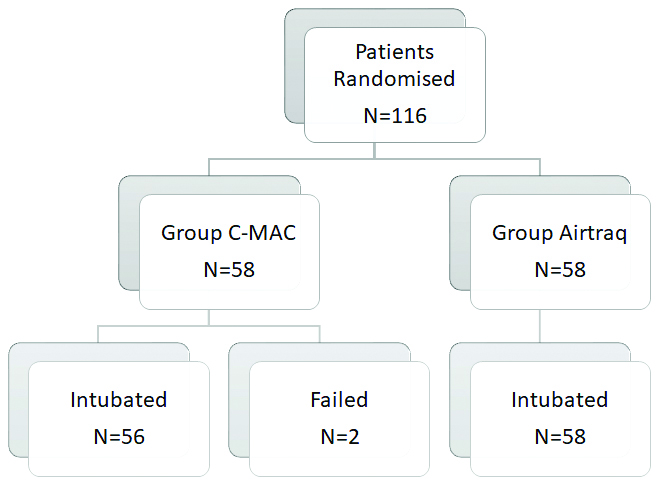
Fifty-eight patients were assigned to C-MAC D-blade and 58 patients to Airtraq group by computer generated random numbers [Table/Fig-1].
Inclusion criteria: Patients between 18-60 years with a Mallampatti score of 1 or 2, posted for elective surgeries under general anaesthesia were included in the study.
Exclusion criteria: Patients with anticipated difficult intubation like patients with Body Mass Index (BMI) >30, neck circumference >42 cm, Mallampatti grading three and above, patients with restricted neck mobility, distorted airway, cervical spine pathologies, pregnant or emergency surgeries were excluded from the study.
Pre-anaesthetic assessment was done on the day prior to surgery. Routine investigations were done according to the institutional protocol in all the patients. On the day of surgery, the patients were connected to the standard ASA monitors and anaesthetised using glycopyrrolate, fentanyl, propofol and vecuronium according to the weight of the patient. Patients were manually ventilated with sevoflurane 2% in oxygen for 3 minutes. The neck was immobilised using MILS applied by an experienced anaesthetist standing by the side of the patient and steadying the neck with hands on the mastoid process on either side of the neck and forearm resting on the upper chest, thereby preventing flexion/extension movement or rotational movement of the head and neck. Laryngoscopy and intubation were performed using either C-MAC D-blade or Airtraq by an experienced anaesthesiologist. The following parameters were recorded.
Time taken for intubation (in seconds)
Cormack and Lehane grading (CL 1, CL 2, CL 3, CL 4) [9]
External manipulation, if required (Yes/No)
Use of bougie, if required
Haemodynamic changes (heart rate and mean arterial pressure).
Trachea was intubated with appropriate size endotracheal tube. External manipulation was applied, if Cormack and Lehane grading was equal or more than 2. Bougie was used, if Cormack and Lehane grading was equal or more than 2 even after external manipulation. If intubation was not possible or if it required more than 3 attempts for intubation, it was considered as a failed intubation. In such situations, MILS was removed and the patients were intubated using standard intubation practice. The time taken from the introduction of laryngoscope to connection of endotracheal tube to the circuit with the appearance of normal ETCO2 curve was noted and taken as the intubating time. Heart rate, mean blood pressure were recorded, preinduction and at 0, 3, 5 and 10 minutes after successful intubation. Tachycardia or hypertension were considered, if the heart rate and mean blood pressure increased more than 20% from the baseline. If it increased more than 30% from the base line, Inj.Esmolol 500 mcg/kg had to be given intravenously as bolus dose.
Statistical Analysis
Statistical Analysis was done using Statistical Package for the Social Sciences (SPSS) version 21. Mean, Standard deviation, number and percentage were used to measure frequency distribution. Paired Student’s t-test was used to compare the mean between two groups and repeated measures of Analysis of Variance (ANOVA) to find significance in variation of Heart rate and mean arterial pressure. The p-value <0.05 was considered significant.
Results
There were two failed cases that were excluded from comparative analysis for time for successful intubation, heart rate and blood pressure variations [Table/Fig-1]. The demographic details were comparable between both the groups [Table/Fig-2]. Neck circumference was also measured and the mean neck circumference was 35.86 cm in the C-MAC group and 36.38 cm in the Airtraq group with no statistically significant difference (p=0.735).
| Demographic details | C-MAC D-blade (Mean±SD) | Airtraq (Mean±SD) | p-value |
|---|
| Age (Year) | 36.05±12.664 | 35.86±13.664 | 0.938 |
| Gender (M/F) | 26/32 | 28/30 | 0.710 |
| Weight (kg) | 63.88±11.906 | 65.28±10.683 | 0.507 |
| Height (mtr.) | 161.91±10.226 | 161.31±9.658 | 0.744 |
| BMI | 24.297±3.4110 | 25.074±3.2984 | 0.215 |
| Neck circumference (cm) | 35.86±8.447 | 36.38±7.947 | 0.735 |
M: Male; F: Female; BMI: Body mass index
The time taken for intubation was comparative between the two groups [Table/Fig-3]. The two failed cases in the C-MAC group were excluded from comparative analysis for time for successful Intubation. There was no difference in the time taken for intubation between the groups.
Comparison of time for successful tracheal intubation (in Sec).
| Group | Mean time (Sec.) | Standard deviation | p-value |
|---|
| Group C-MAC D-blade, N=56 | 41.88 | 19.310 | 0.734 |
| Group Airtraq N=58 | 40.78 | 16.752 |
t-test and Levene’s test were used to compare the study groups
CL grading between two groups showed no statistically significant difference using Chi-square testing (df) with p-value of 0.083 (>0.05). The Cormack Lehane view of vocal cords was I in 48.3% and II in 51.7% of the C-MAC D-blade group of patients. 65.5% of the patients in Airtraq group had CL I view and 32.8% patients had CL II grading. A 1.7% of patients in airtraq group and none in D-blade group had CL III grading [Table/Fig-4].
Comparison of Cormack-Lehane (CL) view between two groups.
| Group | CL view (Count %) | Total | p-value (Chi-square test) |
|---|
| 1 | 2 | 3 |
|---|
| C-MAC D-blade | 28 (48.3%) | 30 (51.7%) | 0 | 58 | 0.083 |
| Airtraq | 38 (65.5%) | 19 (32.8%) | 1 (1.7%) | 58 |
| Total | 66 (56.9%) | 49 (42.2%) | 1 (0.9%) | 116 |
Need for ELM- Chi-square testing (df) with p-value of 0.04 which is less than 0.05 showing a significant difference. Patients in Airtraq group required ELM for successful placement of tracheal tube [Table/Fig-5].
Comparison of External Laryngeal Manipulation (ELM).
| Group | Yes, n (%) | No, n (%) | Total | p-value (Cho-square test) |
|---|
| C-MAC D-blade | 26 (44.8%) | 32 (55.2%) | 58 | 0.04 |
| Airtraq | 37 (63.8%) | 21 (36.2%) | 58 |
| Total | 63 (54.3%) | 53 (45.7%) | 116 |
<0.05 considered significant
The need for airway adjuncts was not studied, as bougies or stylets could not be used in airtraq because of the fixed curvature. In C-MAC D-blade, the endotracheal tube was pre-curved with a stylet to accommodate the curvature of the laryngoscopic blade.
There were no significant difference between the groups with regards to heart rate and mean arterial pressure [Table/Fig-6,7].
Heart rate changes (beats/minute).
| Time (Min.) | C-MAC D-blade (Mean±SD) | Airtraq (Mean±SD) | p-value (Repeated measures of ANOVA) |
|---|
| Pre-induction | 79.16±13.788 | 83.71±12.987 | 0.07 |
| 0 min | 98.12±14.005 | 100.40±11.790 | 0.350 |
| 3 min | 92.43±13.191 | 94.17±12.662 | 0.473 |
| 5 min | 87.18±12.454 | 86.29±11.515 | 0.694 |
| 10 min | 82.11±11.276 | 80.55±11.001 | 0.458 |
SD: Standard deviation; ANOVA: Analysis of variance
Mean arterial pressure changes (mmHg).
| Time (Min.) | C-MAC D-blade (Mean±SD) | Airtraq (Mean±SD) | p-value (Repeated measures of ANOVA) |
|---|
| Pre-induction | 90.57±11.541 | 93.02±16.438 | 0.355 |
| 0 min | 99.07±13.195 | 103.29±10.570 | 0.062 |
| 3 min | 92.54±11.558 | 93.84±12.870 | 0.569 |
| 5 min | 86.29±11.861 | 86.10±12.017 | 0.935 |
| 10 min | 75.45±17.735 | 79.60±11.354 | 0.138 |
SD: Standard deviation; ANOVA: Analysis of variance
Discussion
The present study was undertaken to compare the two laryngoscopes, C-MAC D-blade and Airtraq, by setting the time taken for intubation as the primary objective; in patients undergoing general anaesthesia with simulated MILS. There was no difference in the mean time taken to place a tracheal tube successfully between C-MAC D-blade group and airtraq group.
In a study conducted by McElwain J and Laffey J, comparison of the intubation difficulty scores between Airtraq, C-MAC and McIntosh laryngoscopes with cervical spine immobilisation was undertaken [10]. The intubation difficulty scores were lowest with airtraq compared to McIntosh and C-MAC laryngoscopes with cervical spine immobilisation and also, the need for optimising maneuvers were less with airtraq than the other two laryngoscopes. It was concluded that airtraq reduced the intubation difficulty scores, enhanced the Cormack Lehane glottic view and decreased the number of optimisation manuevers. In another meta-analysis done by Kleine-Brueggeney, among a comparison of six videolaryngoscopes, Airtraq performed better with mean time to intubation compared to C-MAC D-blade, Glidescope, McGrath, AP advance or Kingvision [2]. However, the time taken to view the cords and the glottic view were better with the nonchanneled laryngoscopes than the channeled counterparts.
Laryngoscopic view: Clinically, Airtraq seemed to provide a better laryngoscopic view than the D-blade [Table/Fig-4]. Clinically, Airtraq seemed to provide a better laryngoscopic view than the D-blade. This is in agreement with the study conducted by Maharaj C et al., where all the 20 patients in the Airtraq group had CL I grading [11]. Also, the time taken to successfully intubate was less in Airtraq group than the McIntosh group in their study. In a study conducted by Kılıçaslan A et al., comparing C-MAC D-blade, conventional C-MAC and McIntosh laryngoscopes, D-blade caused less dental compression than the other two. Failure to intubate in 7% of the patients in D-blade group, in spite of a good laryngoscopic view was also noted, in spite of a good glottic view [12]. This was also true for McGrath, Truview and Glidescope laryngoscopes. These difficulties are faced when the blades are curved and angulated. When the blade was more angled to get a better view of the glottis, the tip of the tube impinges on the anterior tracheal wall and could not be advanced further [2]. Two patients among 58 patients in C-MAC group D-blade could not be intubated though the CL grading less than II and were intubated with the conventional McIntosh laryngoscope [Table/Fig-1]. In a clinical scenario with difficult laryngoscopic view, ELM is helpful in optimising the laryngoscopic view. A 44.8% of patients required ELM in C-MAC D-blade group and 63.8% patients required ELM in airtraq group [Table/Fig-5]. This is in concordance with the study conducted by Xue FS et al., where they concluded the effectiveness of maneuvers in paediatric difficult airway intubations improving the laryngoscopic views in airtraq [13]. As a standard practice, stylet was used in C-MAC D-blade Videolaryngoscope. However, stylet cannot be used in airtraq because of the fixed curvature of the blade. So, the use of bougie was not accounted for in the study. An improved result with hockey stick stylet usage has been demonstrated in a study conducted by Batuwitage B et al., with respect to time taken for intubation [14]. Jain D et al., found that the overall performance of conventional C-MAC was better compared to D-blade, McCoy or McIntosh for intubation in simulated cervical spine injury [15].
Haemodynamic parameters: Heart rate and arterial pressure variations were monitored in all the 116 patients from preinduction to 10 minutes postintubation at regular intervals. In both the C-MAC D-blade group and Airtraq group, there was a significant increase in heart rate from 0-3 minutes postlaryngoscopy and started to settle down after 3 minutes without any intervention [Table/Fig-6] in a study done by Maharaj C et al., the heart rate changes were less with airtraq than with McIntosch [16]. Unlike their study, a statistical significance couldn’t be demonstrated in this study probably because of the curvature of the D-blade causing lesser trauma.
Similarly, the arterial pressure increased significantly in both the group of patients post laryngoscopy and intubation. The blood pressure dropped to preinduction values after 5 minutes [Table/Fig-7] and none of the patients showed an increase in blood pressure of more than 30% the baseline requiring esmolol as per the protocol. In a study conducted by Varsha AV et al., they compared the haemodynamic stress response during intubation between MacIntosh and Airtraq laryngoscopes in cardiac patients, the airtraq intubations provided better haemodynamic stability than MacIntosch [17]. The reason could be the videoscopes applied lesser traction in the oropharynx to get a better glottic view. This may be extrapolated to D-blade laryngoscope too as in present case. In another study conducted by McElwain J et al., the changes in the heart rate and mean arterial pressure had returned to baseline 5 minutes after intubation [18].
Limitation(s)
The study was conducted in ASA I & II patients with simulation of neck stabilisation. Further studies are required to extrapolate the results for difficult airway scenario like obesity, higher Mallampatti grading and patients with associated co-morbidities. Also, the present study have not compared the number of attempts required to intubate.
Conclusion(s)
From this study of 116 demographically, MILS patients, both airtraq Videolaryngoscope and C-MAC D-blade were comparable with respect to time taken for intubation and providing a good laryngoscopic view. ELM was required more in airtraq group and usage of stylet was mandatory in all the patients in D-blade group. Haemodynamic stability was comparable in both the groups. However, C-MAC laryngoscopes may be considered better because it is not limited by the battery life.
M: Male; F: Female; BMI: Body mass index
t-test and Levene’s test were used to compare the study groups
<0.05 considered significant
SD: Standard deviation; ANOVA: Analysis of variance
SD: Standard deviation; ANOVA: Analysis of variance