Pulmonary Nocardiosis in Immunocompetent Patient: A Rare Case Report
Kusum V Shah1, Saket Kumar2, Yash Rana3, Arti D Shah4
1 Professor, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth (Deemed To Be University), Vadodara, Gujarat, India.
2 Third Year Postgraduate Resident, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth (Deemed To Be University), Vadodara, Gujarat, India.
3 Assistant Professor, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth (Deemed To Be University), Vadodara, Gujarat, India.
4 Professor and Head, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth (Deemed To Be University), Vadodara, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Saket Kumar, Room No. 82, Gargi Hostel, Sumandeep Vidyapeeth, Vadodara, Gujarat, India.
E-mail: saket1503@gmail.com
Pulmonary nocardiosis is a rare bacterial infection that may lead to severe disease in immunodeficient patients and usually not so common in immunocompetent patients. The report is about a 57-year-old male with Norcardiosis. His sputum and Bronchial Alveolar Lavage (BAL) were negative for acid-fast bacilli. Nocardia species was isolated in BAL culture. He was started on Trimethoprim/Sulfamethoxazole and Clarithromycin, which was later continued for six months.
Immunocompromised, Organ transplant, Pulmonary infection
Case Report
A 57-year-old male, farmer by occupation, presented in respiratory medicine Outpatient Department with complaints of dry cough, breathlessness and high grade fever for past 15 days. Patient had past history of pulmonary Koch’s 30 years back and completed treatment for six months.
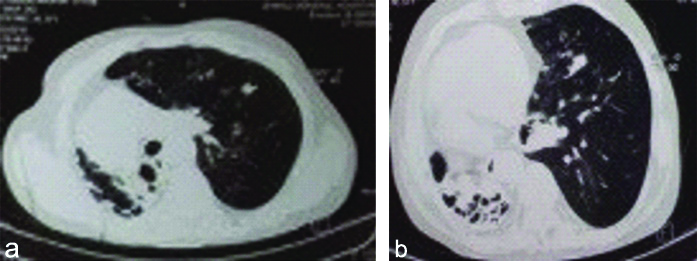
On examination, patient was afebrile, pulse rate- 110/min, bood pressure-120/80 mm Hg, SpO2-95% on room air. On inspection, drooping of shoulder was present on right side and trachea shifted to right side. Inspectory findings were confirmed on palpation and on auscultation, bronchial breathing was present on right suprascapular, interscapular and supraclavicular areas with bilateral generalised polyphonic rhonchi. Laboratory investigations revealed Hb-9.4 g/dL, WBC-10,000 mm3, DLC- Neutrophils/Lymphocytes/Eosinophils/Monocytes-82/10/02/02, ESR-34 mm/hr. The chest radiograph was suggestive of right-sided fibrocavitory lesion with destruction of lung parenchyma [Table/Fig-1]. CT thorax showed fibro-bronchiectatic changes in right lung with near complete collapse and shift of cardio-mediastinum to right side, multiple nodular opacities in left-sided lung with surrounding ground glass opacities [Table/Fig-2]. There were multiple calcified granulomas in both lung fields with few noncalcified lymph nodes in pretracheal, paratracheal, paracarinal and subcarinal region. Clinical and radiological findings were in more favour of infective aetiology, pulmonary koch’s, and fungal infection as a differential diagnosis. Sputum was negative for Acid Fast Bacillus (AFB). Bronchoscopy was done and Bronchial Alveolar Lavage (BAL) was negative for AFB. Nocardia species was isolated in culture of BAL. Patient was started on Trimethoprim/Sulfamethoxazole and Clarithromycin and called for follow-up after 15 days. Clinical improvement and partial resolution of shadows were seen on follow-up.
Chest X-ray PA view showing right sided fibrocavitory lesion with destruction of lung parenchyma.

CT thorax showing fibro-bronchiectatic changes in right lung with near complete collapse and multiple nodular opacities in left-sided lung.
Discussion
Pulmonary nocardiosis is a rare but a life-threatening infection caused by Nocardia species. Nocardia species, areaerobic, gram-positive bacilli, forming branching filaments and have a beaded appearance on Gram stain [1]. The diagnosis is often missed causing delay in appropriate treatment and increasing mortality. Pulmonary nocardiosis particularly affects individuals with low cell-mediated immunity for example those with human immunodeficiency virus infection, malignancies, solid organ, or haematopoietic stem cell transplantation, and those on long-term treatment with steroids or other immunosuppressive pressants [2]. Besides immunosuppression, impaired local pulmonary defense mechanism predispose to pulmonary nocardiosis. The diagnosis of pulmonary nocardiosis is often challenging due to the fact that there are no specific pathognomonic signs or symptoms. Isolation and identification of the organism from the clinical specimens (BAL, biopsy) forms the backbone for diagnosis of pulmonary nocardiosis [3].
Pulmonary nocardiosis may present as an acute, subacute or chronic disease, very similar to tuberculosis or community-acquired pneumonia. Fever, cough, breathlessness, haemoptysis, and weight loss are the common symptoms. Nocardiosis is likely to mimic fungal pneumonia and lung cancer. Imaging studies are not diagnostic. Nodules, necrotising consolidation, cavities, and mass shadows are some of its varied but non-specific presentations [4].
Baburao A et al., presented a case series on pulmonary nocardiosis in an immunocompetent renal transplant recipient patient. The presented with similar clinico-radiological profile and with SpO2 of 90% on room air with bilateral crepitations scattered through the lung fields. Sputum was negative for AFB, BAL revealed Nocardia species; following which he was started on Trimethoprim-Sulphamethoxazole and Linezolid [5].
The CT thorax of the index patient showed multiple nodular opacities in left lung suggestive of infective aetiology (active tuberculosis), while there were few rounded opacities with surrounding ground glass opacities seen in left lung suggestive of fungal aetiology. BAL culture revealed Nocardia species. Due to lack of required infrastructure, species identification could not be done.
The treatment for Nocardiosis needs to be individualised, in view of difference in virulence and in-vitro drug susceptibility of bacterial subtypes. The index patient was treated with Trimethoprim-sulfomethoxazole in combination with clarithromycin for 15 days. Patient improved clinically as well as resolution of shadows were seen on follow-up; the regimen was continued for the next six months. The usual treatment recommended is for 6 to 12 months of duration, which is usually prolonged in immunocompromised patients [6].
Conclusion(s)
Pulmonary nocardiosis is often missed, underestimated and requires appropriate microbiological correlation. It should always be considered in the differential diagnosis of pneumonia, not only in the immunocompromised, but also among non-responding immunocompetents. Nocardiosis must be excluded primarily in the patients who do not respond to anti-tubercular treatment.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 06, 2020
Manual Googling: Nov 23, 2020
iThenticate Software: Dec 14, 2020 (20%)
[1]. Beaman BL, Burnside J, Edwards B, Causey W, Nocardial infections in the United States, 1972-1974J Infect Dis 1976 134:286-89.10.1093/infdis/134.3.286789786 [Google Scholar] [CrossRef] [PubMed]
[2]. Wilson JW, Nocardiosis; Updates and clinical overviewMayo Clin Proc 2012 87:403-07.10.1016/j.mayocp.2011.11.01622469352 [Google Scholar] [CrossRef] [PubMed]
[3]. McNeil MM, Brown JM, The medically important aerobic actinomycetes: Epidemiology and microbiologyClin Microbiol Rev 1994 7:357-417.10.1128/CMR.7.3.3577923055 [Google Scholar] [CrossRef] [PubMed]
[4]. Tsujimoto N, Saraya T, Kikuchi K, Takata S, Kurihara Y, Hiraoka S, High-resolution CT. Findings of patients with pulmonary nocardiosisJ Thorac Dis 2012 4:577-82. [Google Scholar]
[5]. Baburao A, Prasad S, Prakash S, Narayanswamy H, Pulmonary nocardiosis: Report of two cases from a tertiary care hospitalIndian J Pathol Microbiol 2019 62:153-55.10.4103/IJPM.IJPM_793_1730706884 [Google Scholar] [CrossRef] [PubMed]
[6]. Aggarwal D, Garg K, Chander J, Saini V, Janmeja AK, Pulmonary nocardiosis revisited: A case seriesLung India: official organ of Indian Chest Society 2015 32(2):165-68.10.4103/0970-2113.15263825814804 [Google Scholar] [CrossRef] [PubMed]