Fluid for irrigation is widely used in the manipulation of the urinary tract to dilate the mucosal spaces and to clear the operating field of blood and dissected tissue. Various studies done previously have demonstrated that there is a drop in core temperature and shivering incidences in these procedures [1,2]. Perioperative shivering is very common under spinal anaesthesia. Its incidence rate is 40 to 70% [1]. Shivering can be very unpleasant and physiologically stressful for the patients after enjoying the comforts of modern anaesthesia. It interferes with electrocardiogram, pulse rate, blood pressure monitoring [2,3].
Shivering increases oxygen consumption to four times its basal value, increases CO2 production, causes a rise in intracranial and intraocular pressure, leads to severe discomfort and pain, can also increase surgical bleeding. This harmful event has got very complex pathophysiology so no modality of treatment is perfect. Hence, it is advisable to prevent hypothermia and shivering.
Various drugs used in the treatment of shivering are ketanserine, ketamine, nefopam, tramadol and pure μ opioid receptor agonists like morphine, fentanyl, etc. But none is truly effective, also higher doses of anti-shivering medications can lead to adverse effects like respiratory depression, nausea vomiting, itching and sedation etc. Considering the complexity of managing shivering it is always better to prevent the occurrence of shivering [2,3].
Tramadol and fentanyl both have proved useful for shivering prevention when used in spinal anaesthesia but their role is not studied and compared in a selected population of endoscopic urological cases like Transurethral Resection of the Prostate (TURP), Ureteroscopy (URS), Percutaneous Nephrolithotomy (PCNL), cystoscopy with Optical Internal Urethrotomy (OIU) and/or Bladder Neck Incision (BNI), cystolithotomy, cystoscopy, etc., which involves large amount of irrigation of mucosal spaces to dilate and to create working field. Also to clear it of blood and tissue [1].
The primary aim of the study was to compare the anti-shivering effect of intrathecal tramadol with intrathecal fentanyl when given as an additive in spinal anaesthesia for endoscopic urosurgical cases. Secondary outcome was to study the safety profile of the drugs.
Materials and Methods
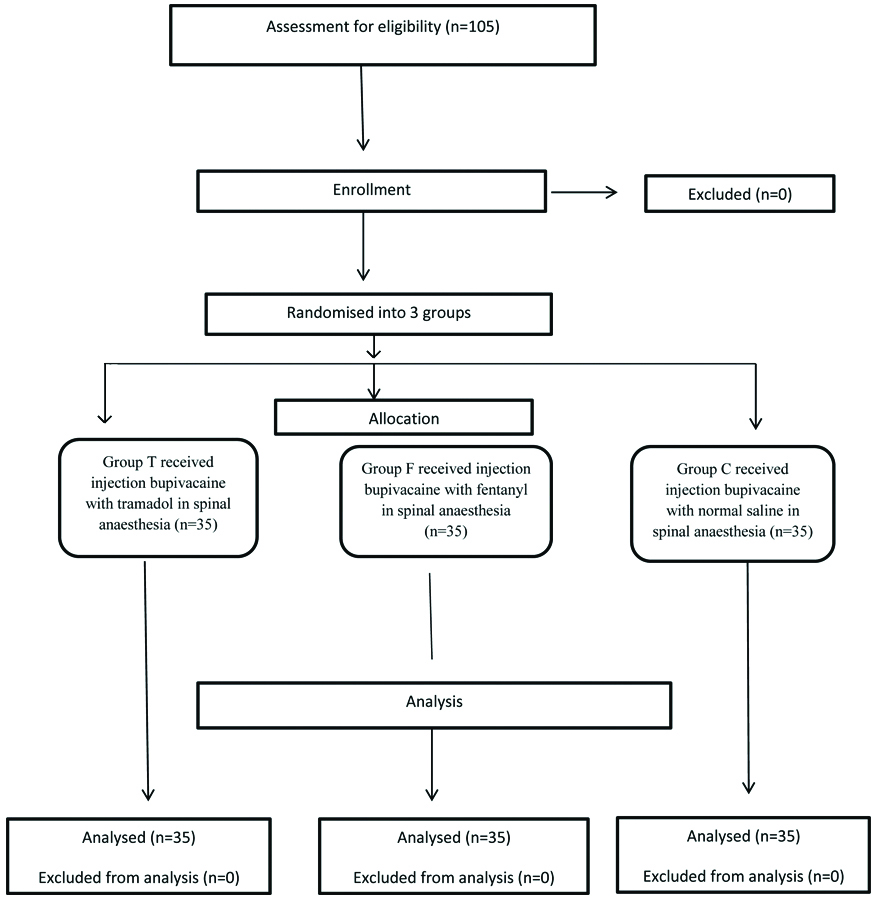
It was a randomised, double-blind control study conducted at MIMER Medical College, Pune. After obtaining approval (IEC No /591 dated 20-02-2019) from the Institutional Ethical Committee and informed consent from the patients, a total of 105 patients undergoing various endoscopic urological surgeries under spinal anaesthesia were included in the study. Study duration was from February to September 2019. The CONSORT diagram is shown in [Table/Fig-1].
Inclusion criteria: Patients undergoing endoscopic cryosurgical procedures like URS, TURP, PCNL, cystoscopy, 18 to 60 years of either sex, ASA grade I and II.
Exclusion criteria: Patients with absolute contraindication to spinal anaesthesia, patient refusal, known allergy to any of the study drugs, ASA grade III and onwards.
Sample size calculation
The confidence interval contains an estimate, above or below a margin of error. The margin of error for a 95% confidence interval is 1.96 times the standard error. It shows the accuracy of the guess and is based on the variability of the estimate.
Let E denote the margin of error.
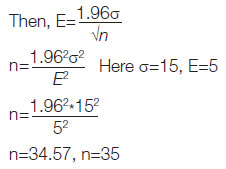
Thirty five patients were included in each group by closed envelope randomisation method.
Group T patients received injection tramadol 20 mg (0.4 mL) with injection bupivacaine 0.5% heavy 15 to 20 mg (3 to 4 mL) in spinal anaesthesia, Group F received injection fentanyl 25 microgram (0.5 mL) with injection bupivacaine 0.5% heavy 15 to 20 mg (3 to 4 mL) in spinal anaesthesia, Group C received injection sodium chloride as placebo 0.5 mL with injection bupivacaine 0.5% heavy 15 to 20 mg (3 to 4 mL). Drug syringes were wrapped with sterile tape for blinding. For all the three groups injection bupivacaine and the additive drug were given through two different syringes. All patients received injection Ondansetron as an antiemetic in a dose of 0.08 mg per kilogram intravenously. All the patients received warm intravenous crystalloids (warmed using electric kettle fitted with thermometers at 37°C), OT temperature was maintained between 22°C to 25°C, and all patients were completely covered with drapes except for the operative field. Any episode of perioperative shivering was treated with mechanical warming methods like warming blanket, keeping warm fluid bottles or hot water gloves in underarms.
Primary outcome analysis: In all the three groups, the following parameter were recorded intraoperatively and postoperatively up to 2 hours
a) Incidence of shivering. Grade of shivering was assessed by Wrench grading system [6]:
0-No shivering
1- One or more of: piloerection, peripheral vasoconstriction but without visible muscular contraction.
2- Visible muscular activity confined to one muscle group
3- Visible muscular activity in more than one muscle group
4- Gross muscular activity involving entire body
Secondary outcome analysis:
a) Level of sedation was assessed by sedation scale [7]:
0-Awake and alert
1-Resting with eyes closed;
2-Drowsy and responsive to verbal stimuli,
3-Unarousable.
b) Perioperative nausea and vomiting were assessed using four-point ordinal scale:
0-No nausea/vomiting
1-Nausea;
2-Itching;
3-Vomiting
Intravenous metoclopramide 10 mg was given as a rescue drug for nausea, vomiting. Incidence of itching was also assessed in all three groups based on subjective complain of itching above the level of sub arachnoid block which was not present before the block.
c) Haemodynamic parameters: mean arterial pressure, systolic blood pressure, diastolic blood pressure, heart rate, peripheral oxygenation as per SPO2 range, axillary skin temperature.
d) Side effects: respiratory rate to diagnose respiratory depression, sedation as per sedation scoring, itching, incidence of nausea, vomiting.
Equipment and drugs required:
Injection (Inj.) Tramadol hydrochloride, inj. Fentanyl, inj. Bupivacaine 0.5% heavy, Spinal needles 25, 26 Quincke type, routine monitoring, Electrocardiogram (ECG), pulse oximeter, Non-Invasive Blood Pressure (NIBP), Heart Rate (HR) monitoring Electric kettle.
Statistical Analysis
The data was analysed using statistical package SPSS version 21.0. Mean and SD were calculated for the quantitative variables. Analysis of variance test was used to compare the means of three groups with respect to each of the parameters. A p-value less than 0.05 were considered statistically significant.
Results
Demographic parameters like age, sex, ASA status, body weight, height were statistically comparable in all three groups [Table/Fig-2]. Also, the basal parameters like heart rate, systolic BP, diastolic BP, SPO2, and axillary skin temperature were statistically comparable as the p-values were not significant. Patients of various urosurgical cases were equally distributed in all three groups, so the three groups were comparable in this aspect [Table/Fig-3].
Demographic and basal/baseline characteristics.
| Variables | Tramadol group (Group T) | Fentanyl group (Group F) | Control group (Group C) | p-value |
|---|
| Age (years) | 42.63±11.15 | 38.77±11.16 | 41.54±13.03 | 0.37 |
| Sex (Male/Female) | 18/17 | 19/16 | 20/15 | 0.26 |
| ASA (I/II) | 27/8 | 25/10 | 24/11 | 0.72 |
| Weight (kg) | 65.62±8.95 | 64.03±10.27 | 59.97±6.85 | 0.22 |
| Height (cm) | 160.83±5.47 | 159.03±7.63 | 156.91±7.17 | 0.16 |
| Basal HR | 72.40±9.38 | 73.20±8.01 | 71.91±10.24 | 0.84 |
| Basal SBP (mmHg) | 120.51±14.14 | 122.91±17.12 | 117.77±14.52 | 0.37 |
| Basal DBP (mmHg) | 74.37±8.25 | 72.40±7.51 | 73.03±10.97 | 0.65 |
| Basal SPO2 | 98.94% | 98.85% | 99.40% | 0.11 |
| Basal axillary skin temperature | 36.72±0.31 | 36.85±0.25 | 36.73±0.33 | 0.14 |
ASA: American society of anaesthesiologist; HR: Heart rate; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; SPO2: Peripheral oxygen saturation; For Sex and ASA status Chi-square test was used and for all other parameters ANOVA was used.
Types of surgeries performed.
| Types of surgery | Group T (n) | Group F(n) | Group C (n) |
|---|
| URS | 18 | 16 | 16 |
| TURP | 6 | 6 | 7 |
| PCNL | 6 | 6 | 7 |
| Cystolithotrispy | 1 | 4 | 2 |
| Cystoscopy +OIU or BNI | 2 | 2 | 2 |
| Cystoscopy | 2 | 1 | 1 |
URS: Uretroscopy; TURP: Trans urethral resection of prostrate; PCNL: Per cutaneous nephrolithotomy; OIU: Optical internal urethrotomy; BNI: Bladder neck incision; test applied: ANOVA
In the intraoperative stage, the haemodynamic variables like heart rate, systolic BP, diastolic BP and mean arterial pressure did not show any significant difference amongst the three groups (p-value >0.05). There was no significant difference (p-value >0.05) of axillary skin temperature amongst the three groups. There was no significant difference in the respiratory rate and SPO2 (p-value >0.05) amongst the three groups which proves that neither the test group nor the control group recorded any significant respiratory depression [Table/Fig-4].
Comparison of intraoperative haemodynamic data.
| Variables | Group T | Group F | Group C | p-value |
|---|
| HR | 72.46±10.15 | 71.94±8.18 | 72.03±11.38 | 0.97 |
| SBP | 113.08±9.97 | 119.40±14.76 | 111.20±13.63 | 0.17 |
| DBP | 71.46±6.91 | 70.94±6.89 | 69.43±8.86 | 0.51 |
| MAP | 85.11±7.37 | 86.77±8.79 | 83.00±9.96 | 0.21 |
| RR | 12.43±0.50 | 12.34±0.74 | 12.00±0.73 | 0.27 |
| SPO2 | 99.4% | 99.6% | 99.3% | 0.14 |
| Axillary skin temperature | 36.64±0.32 | 36.68±0.29 | 36.62±0.32 | 0.73 |
test applied: ANOVA.
HR: Heart rate; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; MAP: Mean Arterial pressure; RR: Respiratory rate; SPO2: Peripheral oxygen saturation
In the postoperative stage also, the haemodynamic variables did not show any significant difference amongst the three groups (p-value >0.05). There was no significant difference of axillary skin temperature, the respiratory rate and SPO2 (p-value >0.05) amongst the three groups [Table/Fig-5].
Comparison of haemodynamic parameters at postoperative stage.
| Variable | Group T | Group F | Group C | p-value |
|---|
| HR | 72.45±10.17 | 71.94±7.17 | 74.14±11.98 | 0.63 |
| SBP | 113.09±9.97 | 119.03±14.19 | 117.71±12.88 | 0.12 |
| DBP | 71.46±6.91 | 71.14±6.98 | 73.06±10.37 | 0.58 |
| MAP | 85.11±7.37 | 87.20±8.62 | 87.26±10.49 | 0.52 |
| RR | 12.43±0.50 | 12.34±0.54 | 12.23±0.69 | 0.36 |
| SPO2 | 99.4% | 98.7% | 98.9% | 0.53 |
| Axillary skin temperature | 36.64±0.32 | 36.67±0.26 | 36.72±0.31 | 0.59 |
test applied: ANOVA.
A significant difference was observed among three groups in respect of incidence of shivering intraoperatively. Least incidence of shivering was observed in tramadol group (four patients), in fentanyl group (six patients) and control group (group C) recorded maximum incidence of shivering (p-value <0.05) (12 patients). Also, the grade of shivering in control group was significantly higher (p-value <0.05) than that of both group F and group T. Incidence of shivering and grade of shivering was least in tramadol group patients indicating better prevention of shivering than control and fentanyl group [Table/Fig-6].
Comparison for different parameters at intraoperative stage (number of patients in each group).
| Variables | Group T | Group F | Group C | p-value |
|---|
| Shivering (Yes/No) | 4/31 | 6/29 | 12/23 | p<0.05 |
| Grade of shivering (I/II/III) | 0/2/2 | 0/2/4 | 0/4/8 | p<0.05 |
| Sedative score (0/1) | 32/3 | 29/6 | 34/1 | p>0.05 |
| Itching (Yes/No) | 1/34 | 4/31 | 34/1 | p>0.05 |
| Nausea, vomiting (Yes/No) | 2/33 | 3/32 | 2/33 | p>0.05 |
test applied: ANOVA.
There was no statistically significant difference among the three groups in respect of sedative score, itching, nausea, vomiting and respiratory depression at the intraoperative stage.
There were significant differences among the three groups in incidence of shivering at the postoperative stage. Maximum incidence of shivering was observed in the control group (p-value <0.05). With regards to the grade of shivering highest number of patients were observed in grade III (8 patients) control group, intermediate but more than tramadol group were recorded in fentanyl group (grade II/III, 3 and 5 patients, respectively) and minimal in tramadol group (grade II/III, 1 and 1 patient respectively (With p-value <0.05). The significant difference was observed among three groups in respect of incidence of shivering at both intraoperative and postoperative stages [Table/Fig-7].
Comparison for different parameters at the postoperative stage (number of patients in each group).
| Variables | Group T | Group F | Group C | p-value |
|---|
| Shivering (Yes/No) | 2/33 | 8/27 | 12/23 | p<0.05 |
| Grade of shivering (I/II/III) | 0/1/1 | 0/3/5 | 0/4/8 | p<0.05 |
| Sedative score (0/1) | 33/2 | 30/5 | 33/2 | p>0.05 |
| Itching (Yes/No) | 2/33 | 4/31 | 0/35 | p>0.05 |
| Nausea, vomiting (Yes/No) | 2/33 | 3/32 | 2/33 | p>0.05 |
test applied: ANOVA.
No significant differences among the three groups were observed in respect of sedative score and itching. There were no significant differences among the three groups in respect of nausea vomiting and respiratory depression at postoperative stage p-value >0.05.
Discussion
Tramadol a synthetic opioid is postulated to exert its anti-shivering effect by μ opioid receptor agonism and serotonin and noradrenaline reuptake inhibition [5,8]. Fentanyl is a potent opioid agonist which is known to have its anti-shivering effect by μ receptor agonism. Both the agents have anti-shivering effect and the purpose of the study was to compare their efficacy with their safety profile in endoscopic urosurgeries. To the best of the author’s knowledge, this is the first study, evaluating and comparing intrathecal tramadol with intrathecal fentanyl in prevention of shivering in endoscopic urosurgeries.
In this study, it was observed that tramadol was most effective in prevention of intraoperative as well as postoperative shivering which is in accordance with the study done by Jayraj A et al., in caesarean section patients [9]. The results also are in accordance with similar studies done by Jain S et al., in anorectal surgeries [10] and Tobi KU et al., in lower limb orthopaedic surgeries [11].
Fentanyl was observed to have anti-shivering effect better than that of placebo but lower than that of tramadol which is in accordance to studies conducted by Chow TC and Cho PH in TURP, and Sadegh A et al., in caesarean section patients [12,13]. Side effects like hypotension and bradycardia were not significant in any of the two study groups as well as control group. In various past studies done with intrathecal tramadol like 10 mg and 20 mg also found that there were no haemodynamic ill effects in tramadol group [14,15]. Intrathecal fentanyl provides haemodynamic stability and incidence of bradycardia and hypotension is rarely noted. A similar trend was observed in this study. Sadegh A et al., also found similar haemodynamic results after use of intrathecal fentanyl in caesarean sections [13]. The incidence of itching, nausea, vomiting, sedation and respiratory depression was not significantly different in any of the study groups and control group as well. Results are similar with multiple similar studies [16-20].
Emetic effect of inj. tramadol is dose dependent. Twenty miligrams intrathecal tramadol is rarely found to cause emesis [21]. Up to 0.5 mg/kg IV or intrathecal dose is not known to cause nausea, vomiting [21]. Considering the safety profile of 20 mg intrathecal tramadol and its significant impact on prevention of shivering in endoscopic urosurgical cases, it is a worth additive and gives comfortable perioperative period.
Limitation(s)
The comparison was done for a schedule of fixed dose of the drugs. The results may vary with doses of drugs but the safety profile may change. A multricentric trial will be appropriate to reduce the error of ethnicity and geographic location.
Conclusion(s)
Intrathecal tramadol is more effective than fentanyl in preventing shivering in endoscopic urosurgical cases. Thus, tramadol can be recommended as an additive in spinal anaesthesia for endoscopic urosurgical cases for effective prevention of shivering and good safety profile.
ASA: American society of anaesthesiologist; HR: Heart rate; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; SPO2: Peripheral oxygen saturation; For Sex and ASA status Chi-square test was used and for all other parameters ANOVA was used.
URS: Uretroscopy; TURP: Trans urethral resection of prostrate; PCNL: Per cutaneous nephrolithotomy; OIU: Optical internal urethrotomy; BNI: Bladder neck incision; test applied: ANOVA
test applied: ANOVA.
HR: Heart rate; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; MAP: Mean Arterial pressure; RR: Respiratory rate; SPO2: Peripheral oxygen saturation
test applied: ANOVA.
test applied: ANOVA.
test applied: ANOVA.