Introduction
India has one sixth of the global population, but accounts for about one-fourth of the global load of Tuberculosis [1]. Genito-urinary cases account for 27% of Extra-Pulmonary Tuberculosis (EPTB) [2]. The exact incidence of FGTB is not known because the cases are obscure and are often under-reported. Many cases of pain abdomen and adnexal mass are FGTB but often misdiagnosed as ovarian tumours. This is a series of four patients who had peculiar presentations and came to a private, tertiary care institute. They were later diagnosed as FGTB. This article reviews the investigations, the role of CBNAAT, need to notify through online nikshay portal and the revised treatment as per the latest Index TB guidelines 2018 [1]. Future structured studies are required to investigate the sensitivity and specificity of different tissues for CBNAAT in different clinical scenarios of FGTB.
Case Series
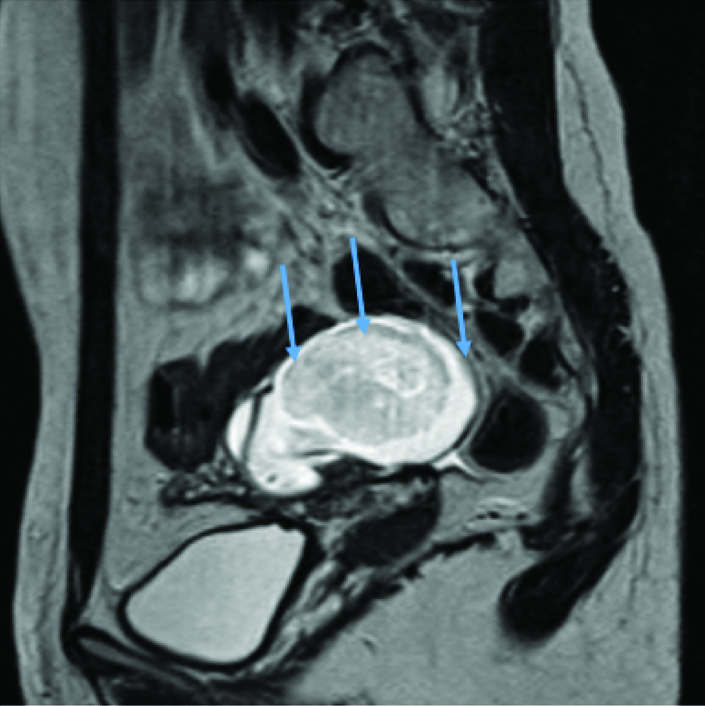
Case 1: A 18-year-old married woman presented to the OPD with complaints of moderate pain in the right side of abdomen and low-grade, evening rise fever with loss of weight since the last one month. The patient also had a Tubo-Ovarian (TO) mass of 5×6 cm since the preceding three months [Table/Fig-1]. The patient had been investigated and treated with antibiotics and antimalarials in different clinics, but without any improvement. Chest x-ray was normal and monteaux was positive. Typhoid, malaria and dengue were ruled out. Blood cultures and culture for Acid Fast Bacilli (AFB) on endometrial curettings were negative. On clinical suspicion, the patient was started on Antituberculosis Therapy (ATT). A diagnosis of tubercular tubo-ovarian with pyrexia was made. She became afebrile within two weeks and the tubo-ovarian mass had resolved on the follow-up sonography, six months later. She completed six months of ATT and has been asymptomatic till the last visit, which was six months after stopping ATT.
MRI T2 weighted sagittal image of pelvis through the adnexa showing complex tubo-ovarian mass in Case 1.
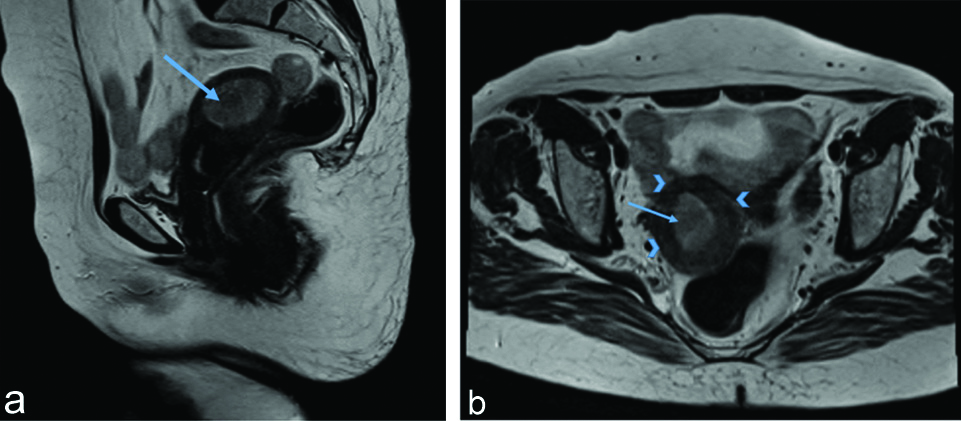
Case 2: A 20-year-old nulliparous woman came to the Outpatient Department (OPD) with a history of five months of amenorrhoea, pus discharge pervaginum and pain in the lower abdomen, since the last one week. Pregnancy test was negative and Ultrasound and MRI showed that the patient had pyometra with no congenital anomalies [Table/Fig-2a,b]. She had a similar episode of pyometra drainage few months earlier. On both the occasions, the pyometra was drained, culture for AFB was negative and CBNAAT could not be afforded by the patient. Her papsmear was normal. Chest X-ray and monteaux were negative. On the basis of the clinical presentation of pyometra in a nulliparous woman and amenorrhoea, a provisional diagnosis of endometrial TB was made. ATT was given for six months. Pain was relieved with no further recurrence of pyometra. However, the secondary amenorrhoea continued which failed to respond to any treatment.
a) MRI T2 weighted sagittal image of pelvis showing dilated endometrial cavity with heterogenous hyperechoeic contents suggesting pyometra in Case 2. b) T2 weighted axial image of pelvis through uterine body (arrowheads) showing dilated endometrial cavity with heterogenous hyperechoeic contents (arrow) suggesting Pyometra.
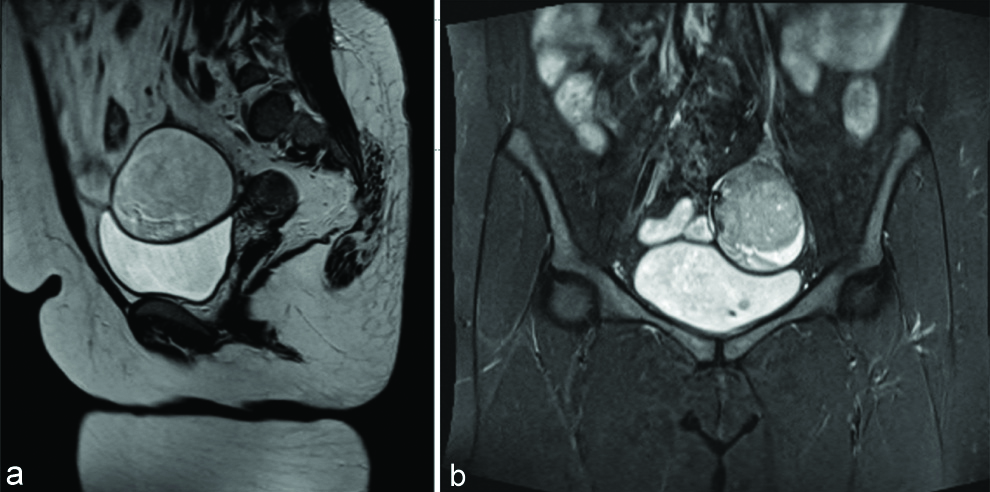
Case 3: A 26-year-old multiparous woman came with the complaints of heaviness and pain on left side of the abdomen, since 2-3 months. The sonography and MRI gave an impression of a unilateral dermoid of 9×8 cm [Table/Fig-3a,b]. On laparoscopy, a 10 cm tubo-ovarian mass was seen with dense adhesions. The case was converted to a laparotomy. After adhesiolysis, the fimbrial end was freed and multiple granules of yellow cheesy caseous material, of 1-2 mm were found clinging on to it. The dissected portion of the tube was congested and edematous. The cyst was found to be an inflammatory peritoneal cyst with the ovary under it. Partial cystectomy, unilateral salpingectomy and contralateral tubal ligation were done. Peritoneal biopsies were also sent. On histopathological examination, the cyst wall was found to be inflammatory with no ovarian components and the caseous material, which was sent for CBNAAT, came out negative possibly due to inadequate sample. On the basis of the typical laparoscopic picture with multiple granules of caseous necrosis, a clinical diagnosis of genital TB was made and the patient completed six months of ATT. The pain was relieved and she experienced a general improvement in appetite and well-being. The patient has been under follow-up for more than three years now and has been symptom free.
Sagittal T2 weighted (a) and STIR (b) (T2 fat suppressed) MR image showing 7-8 cm left adnexal mass with mixed signal intensity suggestive of dermoid.
Case 4: A 39-year-old nulliparous woman came to the OPD with severe chronic pain in lower abdomen, dysmenorrhoea, dyspareunia and menorrhagia since the last one year. The patient had a previous laparoscopy for some mass, nature of which was not known. The patient was a diagnosed case of deep pelvic endometriosis. The pain and menorrhagia failed to respond to Dilation and Curettage (D&C), high dose progesterones and even Dienogest. Endometrial biopsy was negative on culture for mycobacterium.
MRI was done which showed that the uterus was adenomyotic and there was a left-sided 9×7 cm abscess/endometrioma [Table/Fig-4a-c] with a hydrosalpinx with dense pelvic adhesions. The patient was taken up for laparoscopic adhesiolysis and cystectomy. Per-operatively, there were dense adhesions with complete obliteration of the Pouch of Douglas and Uterovesical pouch. A tubo-ovarian abscess of around 10 cm, with dense adhesions was present from which around 80cc of pus was drained. Both the tubes were markedly edematous, congested and necrotic. As per the strong wishes of the patient and family, bilateral salpingectomy was done after due consent. The right ovary was normal and left in situ.
Shows T1 weighted MR through pelvis with left adnexal lesion showing hypointense contents (star) with thick hyperintense walls (arrow). b) Shows T2 weighted MR image with adnexal lesion showing hyperintense contents (star) with thick hypointense walls (arrow). c) Shows corresponding Diffusion weighted MRI at b=800 with diffusion restriction in the contents (star). These imaging features favour adnexal abscess.
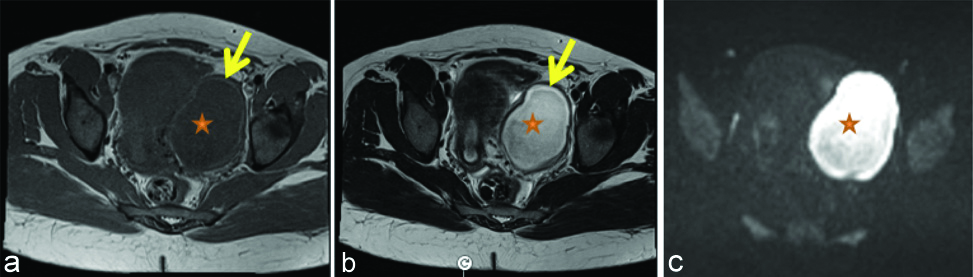
The pus drained from the tubo-ovarian abscess, showed growth of Mycobacterium and was CBNAAT positive. The patient was given ATT for six months. The intensity of pain reduced substantially with ATT. Her cycles also became normal. She has been under follow-up, till one year of the surgery and was found to be very satisfied with the results.
Discussion
In the India TB Report 2020, the government has taken up the target of eliminating TB in India with the National Tuberculosis Elimination Programme (NTEP). India has the highest burden of tuberculosis. In 2019, 26.9 lakh cases were confirmed [3]. Total 80% of the cases are Pulmonary Kochs and around 30% of TB cases occur in women. The exact incidence of FGTB is not known, but estimates say Genital TB contributes to around 9% of EPTB cases [1]. FGTB can manifest as adnexal masses, genital ulcers and may mimic a number of diseases like Pelvic Inflammatory Disease (PID), carcinoma, dermoid, endometriosis etc. Clinical suspicion is of paramount importance when unusual findings present during surgery like unexpected adhesions, caseous material, ascites etc. Infact in any chronic illness in India, TB should always be a differential diagnosis [4-10].
Diagnosis of FGTB: A complete personal and family history is very important. Symptoms may be systemic like fever, weight loss, night sweats or localised like chronic lower abdominal pain, dyspareunia, infertility, menorrhagia, secondary amenorrhea, adnexal masses etc. However, many cases are asymptomatic.
Preliminary investigations include Complete Blood Count (CBC), urinary pregnancy test and chest x-ray. The Tuberculin test (Monteaux) may help in making the diagnosis; however it is only 55% sensitive and 80% specific. Index TB guidelines have made it mandatory to test for HIV in all cases of TB [Table/Fig-5].
Working case definitions of TB.
| Presumptive case | A patient with symptoms and signs of EPTB who needs to be investigated |
|---|
| Bacteriologically confirmed case | A patient who has a microbiological diagnosis of EPTB, based on positive microscopy, culture or a validated PCR-based test.A clinically diagnosed case subsequently found to be bacteriologically positive (before or after starting treatment) should be reclassified as bacteriologically confirmed. |
| Clinically diagnosed case | A patient with negative microbiological tests for TB (microscopy, culture and validated PCR-based tests), but with strong clinical suspicion and other evidence of EPTB, such as compatible imaging findings, histological findings, ancillary diagnostic tests or response to anti-TB treatment.A presumptive case started on ATT empirically, without microbiological testing, should also be considered a clinically diagnosed case (empirically treated). |
| Non-EPTB case | A patient who has been investigated for EPTB and has been diagnosed with a different condition, with no microbiological evidence of EPTB found. |
Reprinted from Index TB Guidelines -Guidelines on extra-pulmonary tuberculosis for India. 2018.
EPTB: Extra-pulmonary tuberculosis; PCR: Polymerase chain reaction; ATT: Antituberculosis therapy
Sonography should be done in all suspected cases to diagnose any signs like mesenteric lymph nodes/ileo-caecal thickening/adhesions or any adnexal mass. Adnexal masses may have calcification or some associated ascites [1,11].
Tumour markers: Should be done in case of complex cysts as either Kochs may mimic carcinoma or both may coexist together. Ca 125 is raised in TB but remain less than 200. A very high level indicates malignancy.
CT/MRI help in assessment of the full extent of the pathology, better delineation of any other structures involved. It is vital to assess the need for a frozen section, to plan the surgical management and to counsel the patients appropriately.
Tissue-based diagnosis: These include Endometrial Aspiration Biopsy (EAB), with or without a hysteroscopy and biopsies taken at laparotomy/laparoscopic surgeries.
Diagnostic hysteroscopy may reveal adhesions (Ashermans syndrome) [11]. Diagnostic Laparoscopy is the gold standard for diagnosis of FGTB. There may be tuberculomas or caseous granulomas on the pelvic organs, fixed tubo-ovarian masses or abscesses. The tube may be damaged manifesting in hydrosalpinx or pyosalpinx. Multiple biopsies have to be taken from the suspicious areas and from the peritoneum [9-12].
All tissues need to be subjected to histopathological examination, Ziehl-Neelsen (ZN) stain, culture with sensitivity testing and cartridge CBNAAT. However, as FGTB is a paucibacillary disease, the results may be negative in spite of the presence of the disease. Wherever possible, TB should be diagnosed preoperatively with the help of imaging and tissue-based diagnosis. It is important to defer surgery and complete ATT. Surgery in active Kochs can spread the disease intra and extraperitoneally.
The Index TB guidelines published by the Ministry of Health and Family Welfarae India have focussed on EPTB and there are clearer guidelines for FGTB [Table/Fig-5] [1]. The guidelines stress on U-DST (Universal drug Sensitivity Testing) for all TB cases, but the infrastructure to support it throughout the country is still lacking. India accounts for one fourth of the global burden of Multidrug-Resistant TB (MDR-TB) and has also seen unique cases of monodrug (isoniazid) resistance [13,14]. Assessment of their numbers and distribution is vital to treat them and arrest further spread. Therefore, CBNAAT is advised for all cases of FGTB-especially endometrial biopsy/laparoscopic biopsy specimens and fluid aspirations.
About CBNAAT
CBNAAT is an automated instrument which does sample processing, nucleic acid amplification, and detection of the target sequences. They are portable and therefore, can be made available in places with minimal outreach as well. The advantage of CBNAAT is that it can improve diagnosis in body fluids which are smear and culture negative. It also tests for rifampicin resistance in all cases [13,14]. The results come back in few hours, so the reports are usually available on the same or next day. This prevents any delay in the treatment. If done in all patients, it will give an idea of the burden of drug resistant TB.
Keeping all these in mind, the government has offered CBNAAT for all cases of FGTB from 2018 onwards. Its disadvantages include its high cost. Another problem arises in small biopsy specimens which either can be sent for CBNAAT or for HPE or for culture. In this institute, it has also been observed that small samples usually test negative with CBNAAT. The CBNAAT tests have primarily improved the diagnosis in body fluids which are smear and culture negative- like in pleural fluid/lymphnode/empyema or ascitic fluid samples [15,16]. As of now, their sensitivity and specificity in FGTB have been extrapolated from that data. So, the diagnosis should take into account all the other microbiological and pathological tests as well. Review of other studies too has proved the need to take clinical picture into consideration, instead of relying on CBNAAT alone for diagnosis of genital TB [11,16,17].
Notification: After diagnosis, it is very important for all healthcare providers to notify the disease, which has become simpler now with Nikshay online notification portal [3].
The notification rates have improved substantially in the last few years. However, only 25% of the notifications come from the private sector, which is very low considering the huge proportion of the population which are catered to, by the private sector especially infertility centers [1,12]. Depending on the clinical scenario, a working case definition should be assigned to each case [Table/Fig-5].
Treatment
The diagnostic criteria for FGTB may be:
ZN stain or culture positive or CBNAAT positive
Histopathological evidence of TB (caseous granulomas or langerhans Giant cells)
Laparoscopic assessment consistent with FGTB.
Treatment may be started, if diagnosis is made by the above criteria or empirically in selected cases, if it has been assessed by a specialist.
Treatment regime [Table/Fig-2]: Two months Isoniazid (H), Rifampicin (R), Pyrazinamide (Z) and Ethambutol (E) + four months Isoniazid (H), Rifampicin (R) and Ethambutol (E)
Index TB guidelines don’t mention separate treatment for relapse or treatment failure and there is no option of thrice weekly doses. There are recommendations for MDR-TB as well which has not been discussed here. There is no need for a repeat laparoscopy to label one as a cured patient, absence of symptoms is sufficient. However, infertility, pain due to adhesions, TO masses etc., may remain as it is a sequelae of the old infection and that cannot be reversed [18]. Selected cases may require surgery. In case of persistence of disease, MDR-TB should be kept in mind and such patients should be referred to designated TB referral centers.
Difficulties in Diagnosis in the Case Series
In all the said cases, diagnosis posed a challenge. There was no personal or family history of tuberculosis and the presentations were unique. Nulliparous pyometra and tuboovarian mass with fever are both scenarios which should raise the suspicion of TB [19]. There was no microbiological confirmation of TB. The surgeon faces a dilemma of whether a very small tissue obtained at surgery should be sent for culture or CBNAAT. Very small tissues may give false-negative reports (like caseous granulomas in the third case). In the latter, two cases presumed to be dermoid and abscess in endometriosis, the final diagnosis was on the basis of operative findings and by culture. If the distinction between an active and old infection becomes difficult, management should involve specialists.
Conclusion(s)
The varied clinical presentations of FGTB may elude diagnosis for some time. Pyometra in a young woman should alert a gynaecologist. During assessment of suspicious adnexal masses, appropriate preoperative evaluation should be done for TB. Wherever there is a suspicion of TB during surgery, ZN staining, sufficient biopsies, culture with sensitivity testing and tissues for CBNAAT should be procured. If they are negative, laparoscopic pictures may aid in diagnosis. Culture should be accompanied by sensitivity testing in all patients. Diagnostic definitions have to be documented and all FGTB cases are notifiable (including empirical treatment on clinical diagnosis). ATT now is two months of HRZE and four months of HRE. Further research will throw light on MDR-TB and the now emerging INH mono-resistance, which may again need a policy change soon.
Reprinted from Index TB Guidelines -Guidelines on extra-pulmonary tuberculosis for India. 2018.
EPTB: Extra-pulmonary tuberculosis; PCR: Polymerase chain reaction; ATT: Antituberculosis therapy
[1]. Index TB Guidelines. Guidelines on extra-pulmonary tuberculosis for India. World Health Organization. 2016 [Google Scholar]
[2]. Golden MP, Vikram HR, Extrapulmonary tuberculosis: An overviewAm Fam Physician 2005 72:1761-68. [Google Scholar]
[3]. Central TB Division, Directorate General of Health ServicesIndia TB. Report: Revised National Tuberculosis EliminationProgramme: Annual status report 2020 New DelhiMinistry of Health and Family Welfare [Google Scholar]
[4]. Koch A, Lecointre L, Garbin O, Pelvic tuberculosis mimicking deep endometriosisJ Gynaecol Obstet Hum Reprod 2017 46(5):463-64.10.1016/j.jogoh.2017.04.00228411084 [Google Scholar] [CrossRef] [PubMed]
[5]. Gupta AN, Shivashankara KN, Pelvic-peritoneal tuberculosis presenting as an adnexal mass and mimicking ovarian cancerAnn Trop Med Public Health 2013 6:117-19.10.4103/1755-6783.115177 [Google Scholar] [CrossRef]
[6]. Ilmer M, Bergauer F, Friese K, Mylonas I, Genital tuberculosis as the cause of tuboovarian abscess in an immunosuppressed patientInfect Dis Obstet Gynaecol 2009 2009:74506010.1155/2009/74506020224814 [Google Scholar] [CrossRef] [PubMed]
[7]. Martingano D, Colon KC, Chiaffarano J, Markus A, Contreras D, Pelvic tuberculosis diagnosed during operative laparoscopy for suspected ovarian cancerHindawi Case Rep Obstet Gynaecol 2018 2018:645272110.1155/2018/645272129850317 [Google Scholar] [CrossRef] [PubMed]
[8]. Efared B, Sidibé I, Erregad F, Hammas N, Chbani L, Fatemi H, Female genital tuberculosis: A clinicopathological report of 13 casesJ of Surg Case Rep 2019 2019(3):rjz08310.1093/jscr/rjz08330937159 [Google Scholar] [CrossRef] [PubMed]
[9]. Sharma JB, Current diagnosis and management of female genital tuberculosisJ Obstet Gynaecol India 2015 65(6):362-71.10.1007/s13224-015-0780-z26663993 [Google Scholar] [CrossRef] [PubMed]
[10]. Kumar S, Sharma JB, Female genital tuberculosis. In: Sharma SK, Mohan A, editorsTuberculosis 2015 3rd edDelhiJaypee:362-71. [Google Scholar]
[11]. Sharma JB, Sharma E, Sharma S, Dharmendra S, Female genital tuberculosis: RevisitedIndian J Med Res 2018 148(Suppl S1):71-83. [Google Scholar]
[12]. Philip S, Isaakidis P, Sagili KD, Meharunnisa A, Mrithyunjayan S, Kumar AMV, They know, they agree, but they don’t do”- the paradox of tuberculosis case notification by private practitioners in Alappuzha District, Kerala, IndiaPLoS ONE 2015 10(4):e012328610.1371/journal.pone.012328625909330 [Google Scholar] [CrossRef] [PubMed]
[13]. Chatterjee S, Poonawala H, Jain Y, Drug-resistant tuberculosis: Is India ready for the challenge?BMJ Glob Health 2018 3(4):e00097110.1136/bmjgh-2018-00097130116597 [Google Scholar] [CrossRef] [PubMed]
[14]. World Health Organization. WHO global tuberculosis report 2017: Geneva: WHO; 2017 [Google Scholar]
[15]. Mukherjee S, Begum S, Kundu S, Mitra S, Clinical profile of tubercular empyema with special reference to diagnostic role of Cartridge Based Nucleic Acid Amplification test (CBNAAT)J Clin Diagn Res 2017 11(10):OC01-OC05.10.7860/JCDR/2017/31193.10689 [Google Scholar] [CrossRef]
[16]. Sharma D, Depan A, Yadav K, Narayan S, Sharma A, Prevalence of female genital tract tuberculosis in suspected cases attending Gynaecology OPD at tertiary centre by various diagnostic methods and comparative analysisInt J Reprod Contracept Obstet Gynaecol 2019 8:2286-92.10.18203/2320-1770.ijrcog20192419 [Google Scholar] [CrossRef]
[17]. Garg R, Agarwal N, Gupta M, Genexpert test and endometrial histological findings in infertile womenInt J Reprod Contracept Obstet Gynaecol 2018 7(4):1480-83.10.18203/2320-1770.ijrcog20181339 [Google Scholar] [CrossRef]
[18]. Tripathy SN, Tripathy SN, Infertility and pregnancy outcome in female genital tuberculosisInt J Gynaecol Obstet 2002 76(2):159-63.10.1016/S0020-7292(01)00525-2 [Google Scholar] [CrossRef]
[19]. Singhal M, Tanwar R, Kumar A, Prasad S, A rare case of tuberculous pyometra in a young infertile female confirmed by mRNA-based RT-PCRJ Fam Reprod Health 2012 6(3):139-41. [Google Scholar]