The Horseshoe Kidneys (HSKs) are the most common congenital fusion of the kidneys, among other fusion anomalies. The incidence of HSK is approximately 1 in 500 in the normal population with a male preponderance of 2:1 [1]. The incidence is higher in those who present to urology clinics with some chromosomal disorders. These include Edward syndrome at approximately 67%, Turner syndrome at 14% to 20%, and Down syndrome at about 1% [2-4]. HSK appear as renal masses along both sides of the vertebra, fused together. The ureters remain uncrossed from the renal hilum to the urinary bladder [5]. The isthmus may be positioned in the midline or laterally. The isthmus is composed of renal parenchyma in about 80% of cases with the remainder being composed of a fibrous band. More commonly, the fusion occurs at the lower pole [6-8]. Insertion of the ureter on the renal pelvis is displaced superiorly and laterally which results into ureteropelvic obstruction. Thus, the HSKs are prone to infection and calculus formation. The incidence of stone formation in such kidneys has been reported to be approximately 20% [9].
Percutaneous puncture of the HSK is considered to be safe because of favourable calyceal orientation and vascularity and there is higher success rate with minimal complication [13-17]. In this era of advancement of RIRS, PCNL still holds strong position for HSK stone management, due to HSK vascular and pelvicalyceal anatomy.
This study aimed to evaluate PCNL in managing large HSK stone disease in the form of stone free rate and to assess procedure related complication between October 2016 to March 2020.
Materials and Methods
This was a retrospective cross-sectional study, performed at a single institute over the period of 4 years (October 2016 to March 2020). The Ethical Committee Clearance was exempted.
Inclusion criteria: The patient record showing stone size >15 mm, failed ESWL and recurrent stones with HSKwere included in the study. So, total 18 patient’s data fit the inclusion criteria.
Exclusion criteria: The patient records showing stone size <15 mm were excluded from the study.
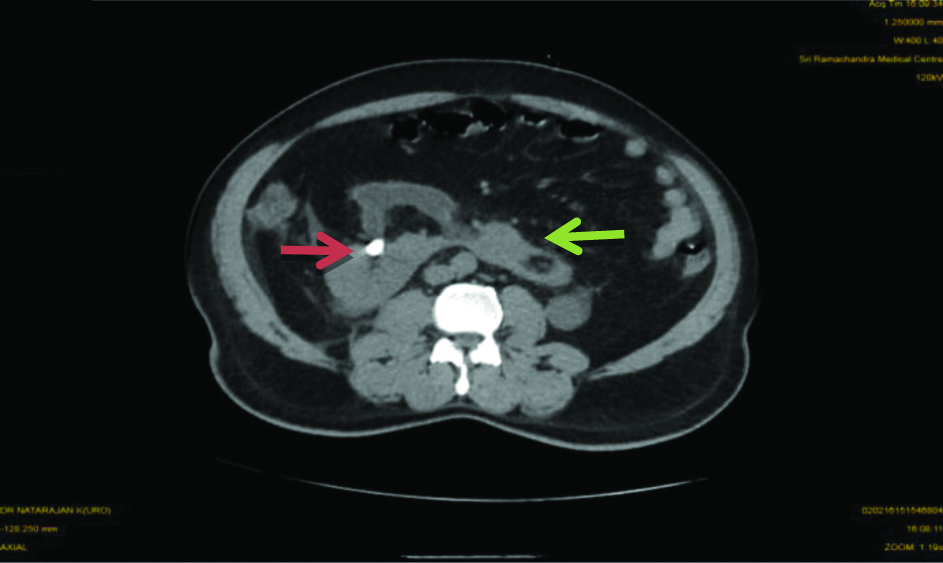
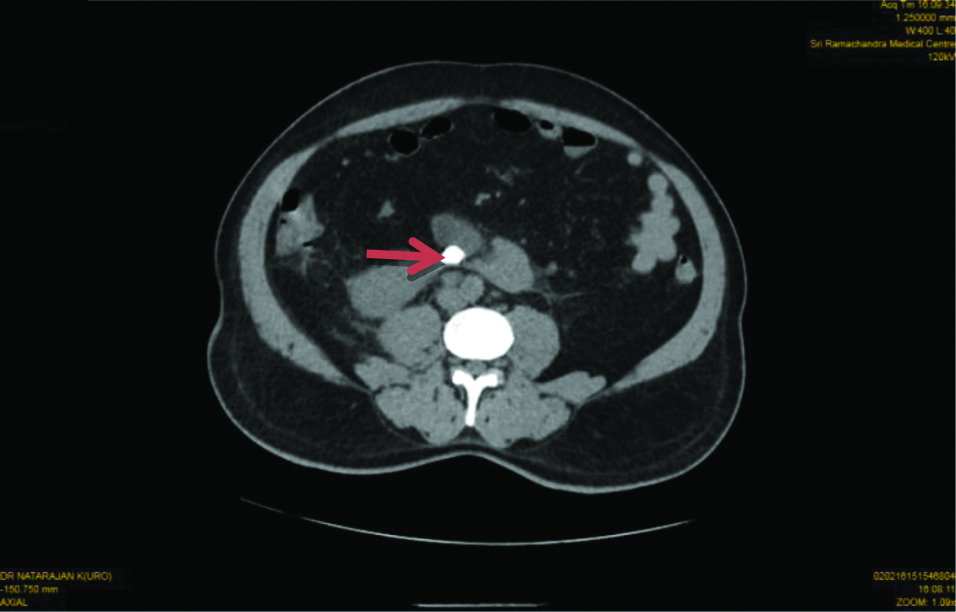
A per the protocol all patients were initially evaluated for medical history, physical examination, urine examination, Renal Function Test, ultrasonography Kidney, Ureter, Bladder (KUB), and Computed Tomography (CT) KUB (plain) [Table/Fig-1,2], CT Urography is done in some specific cases as and when required. Any infection detected in urine cultural and sensitivity is treated with a culture specific antibiotic. All the patients were given one dose of preoperative antibiotic (1.5 g cefoperazone+sulbactum IV) before induction of general anaesthesia.
Computed Tomography (CT) of Kidney, Ureter, Bladder (KUB) region axial cuts showing Horseshoe Kidney (HSK) (Green arrow) and stone in right renal pelvis (Red arrow).
Computed Tomography (CT) of Kidney Ureter Bladder (KUB) region axial cuts showing Horse Shoe Kidney (HSK) and stone in isthmus (Red arrow).
For this study, patient data in the form of sex, age, stone size, stone location, procedure time, Stone-Free Rate (SFR) in the primary procedure, complications according to Clavien grade (intraoperative and postoperative) [18], pain score measured postoperatively using Visual Analogue Score (VAS), hospital stay and ancillary procedures if any were collected and analysed. All surgeries were performed by trained urologist having minimum 5 years post M.Ch. experience. All patients’ data were extracted from the Urology Department.
Procedure
As per the hospital protocol, all the patients were admitted a day before the procedure and anaesthesia evaluation done. All the surgeries were performed under general anaesthesia. The usual surgery procedure is as follows:
Cystoscopy was done; guide wire secured in the kidney and 6F ureteric catheter was placed in lithotomy position. Patient was then turned into prone position. Bolsters were placed underneath the patient’s lower thorax, abdomen and pelvis in order to fix the kidney, pushing it posteriorly and limiting its movement during respiration.
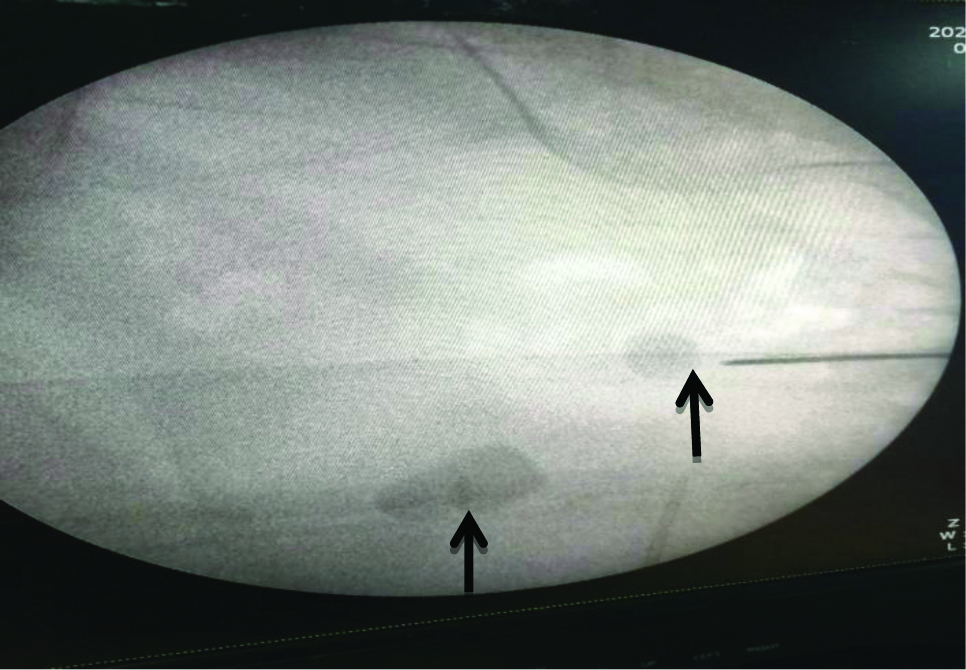
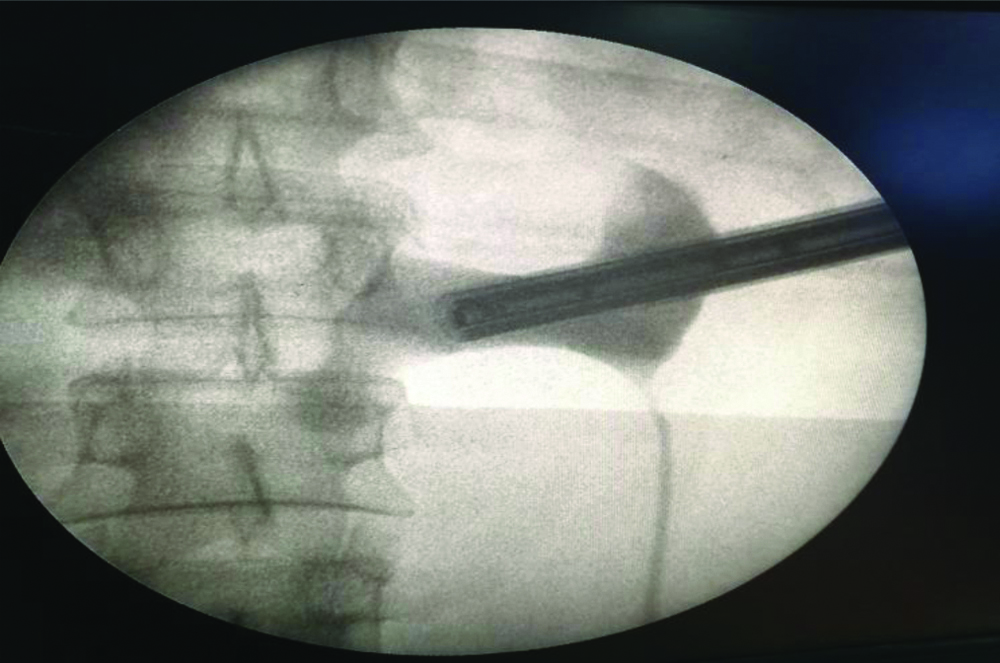
With the C-arm in the vertical position and in zero degree, the pelvicalyceal system was opacified and distended with contrast material through the ureteric catheter. Under C-arm guidance appropriate puncture site was identified, and puncture was made with an 18-gauge I.P. Needle in the desired calyx [Table/Fig-3]. Due to the downward and medial displacement of the calyces, examination with C-arm at 90 degrees provides a direct end-on view of the posterior calyx. The C-arm was then rotated 30 degrees towards the surgeon and the depth of needle penetration is monitored fluoroscopically. In all punctures bull’s eye technique was used. In most of the patient punctures were upper calyceal and subcostal and in few cases middle calyceal puncture was done.
Under C-arm at 0 degree position both stones (right renal pelvis and isthmus) are seen (Black arrow) and puncture was made with an 18-gauge I.P. Needle in the upper calyx.
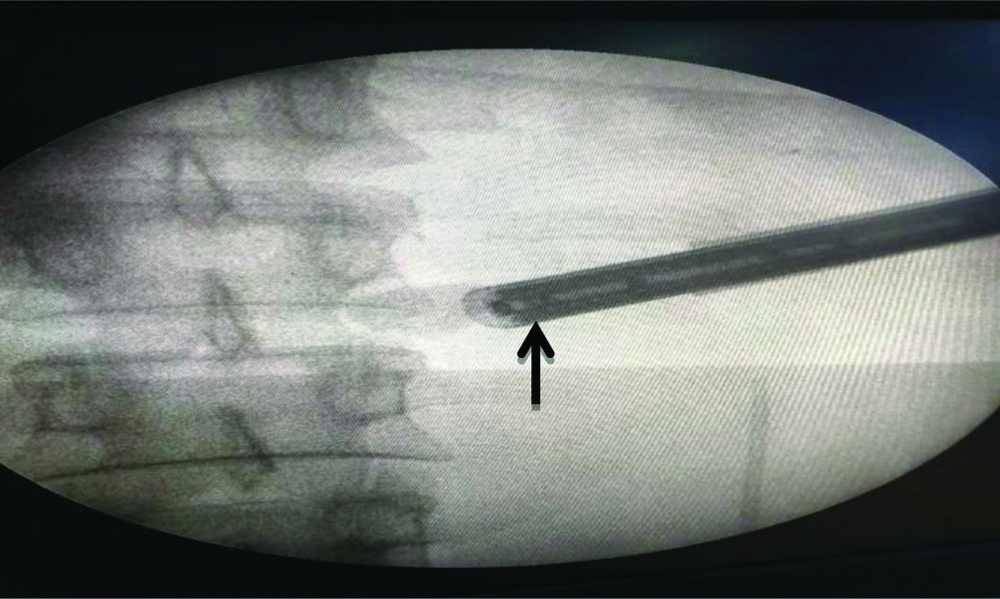
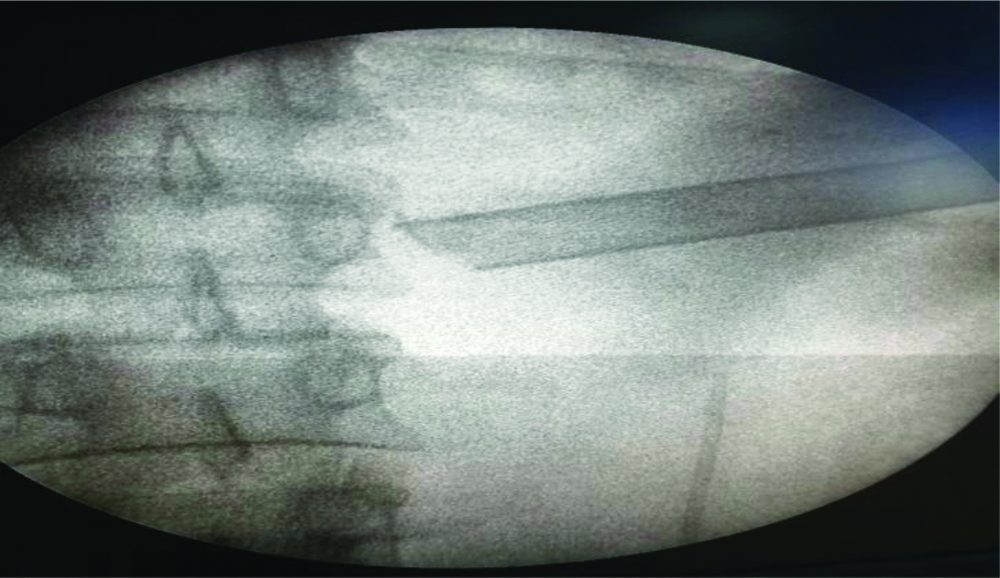
Once the puncture was made, a Lunderquitst extra stiff 0.035 inches guide wire was then passed into the collecting system through puncture needle followed by dilation of the tract using the standard telescopic metal Alken dilators over a central rod. Extra long Amplatz sheath was passed over the dilator in the system. Nephroscopy was done using 28 Fr rigid nephroscope [Table/Fig-4,5]. Stone fragmentation was done using pneumatic lithoclast and larger fragments were removed with biprong forceps and in all patient complete clearance achieved [Table/Fig-6]. Additional calyceal puncture was made as per the requirement in individual cases.
Nephroscopy done using 28 Fr rigid nephroscope (Black arrow) shows stone in isthmus.
Pyelography done using 28 Fr rigid nephroscope shows Horseshoe Kidney’s (HSK) pelvi calyceal system.
Postlithotripsy complete clearance of stone confirmed by intraoperative use of C-arm.
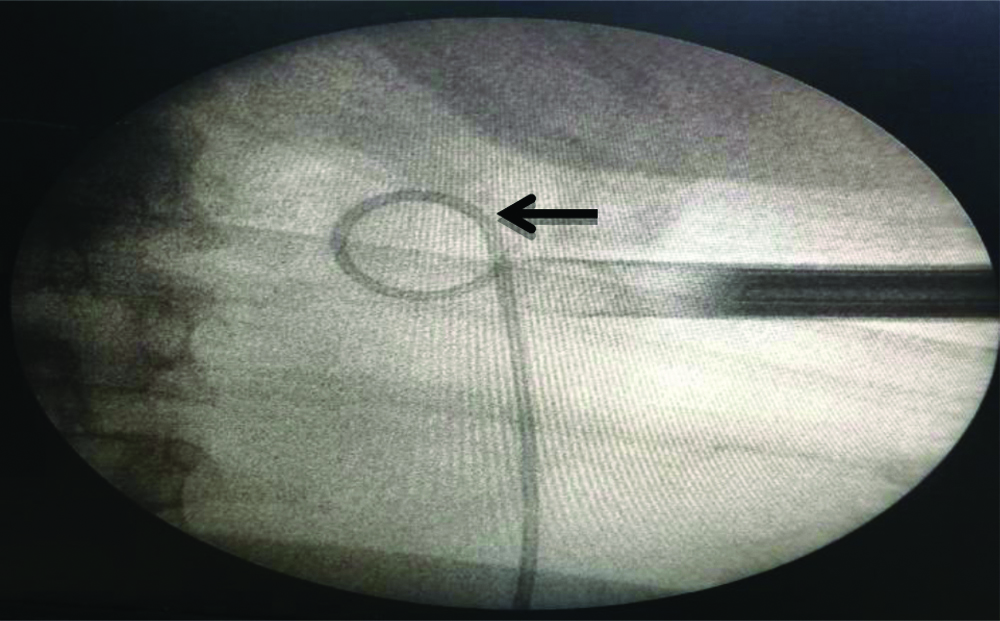
After stone removal, antegrade JJ stenting was done in every case [Table/Fig-7] and nephrostomy tube was avoided in all cases (as a standard institutional protocol). X-ray KUB was performed 24 hours later to detect any residual stones and to check position of JJ stent in every case. Intraoperative and postoperative complications and stone-free rates were recorded. Any stone fragment visible on X-ray KUB or measured more than 4 mm on USG KUB were taken as an incomplete clearance and ancillary procedures were followed for the same. Complications were characterised as major if they required additional intervention or resulted in a prolonged hospital stay (more than 72 hours) or minor if they could be managed conservatively with no additional intervention or morbidity. In all patients JJ stent was removed after one week. The patients were followed-up after one month and six months, clinically.
Antegrade JJ stenting after (Black arrow) confirming complete stone clearance.
All patients were telephonically reached to obtain approval for potential use of their anonymous medical data from the database for research and audit purposes.
Statistical Analysis
Data were coded and recorded in MS Excel spreadsheet program. SPSS v23 (IBM Corp.) was used for data analysis. Descriptive statistics were elaborated in the form of mean/standard deviations and median/IQRs for continuous variables, and frequencies and percentages for categorical variables.
Results
Patient’s age ranged between 29 years to 52 years and mean age was 40.67±7.87 years. Of the 18 patients, there were 12(66.7%) males and 6 (33.3%) females. Three patients had stones in both renal units and were treated separately; therefore total 21 renal units were taken into the study. Nine renal units had stone on right side, 11 had on left side and one had stone in the isthmus. Twenty renal units had single stone and one renal unit had two stones. Two patients had two sessions of prior ESWL.
Six (28.6%) patients presented with pain with haematuria and four (19.0%) cases were diagnosed incidentally. Three patients had only haematuria, that on evaluation were found to be having stone with HSK. Baseline blood investigations (complete blood count, renal function tests, coagulation profile) were within normal limits for all the patients.
The mean Stone Size (mm) was 22.19±7.43 (12.00-46.00) mm. Patients characteristics are listed in [Table/Fig-8]. Twelve units had stone in the pelvis (57.1%) which was the most common location, followed by upper calyx in 6 units (28.6.%). One unit (4.8%) had stone in isthmus and 3 units (14.3%) had staghorn calculi. Access site was upper calyx in majority 16 (76.2%) of the cases, 5 cases (23.8%) required additional puncture most commonly through middle calyx.
| Patient characteristics | Mean±SD || Median (IQR) || Min-Max || Frequency (%) |
|---|
| Age (Years) | 40.67±7.87 || 40.50 (14.50) || 29.00-52.00 |
| Gender | |
| Male | 12 (66.7%) |
| Female | 6 (33.3%) |
| Renal Units involved in 18 patient (Total 21), (%) | |
| One | 15 (71.4%) |
| Two | 3 (14.3%) |
| Stone size (mm) | 22.19±7.43 || 20.00 (6.00) || 12.00-46.00 |
| Location (%) | |
| Right | 9 (42.9%) |
| Left | 11 (52.4%) |
| Isthmus | 1 (4.7%) |
| Presentation, (%) | |
| Incidental finding | 4 (19.0%) |
| Pain | 5 (23.8%) |
| Haematuria | 3 (14.3%) |
| Pain with Haematuria | 6 (28.6%) |
| Pain with UTI | 3 (14.3%) |
| Number of stones, (%) | |
| One | 20 (95.2%) |
| Two | 1 (4.8%) |
| Indication, (%) | |
| Primary | 18 (85.7%) |
| Failed ESWL | 3 (14.3%) |
The mean operating time was 46.76±16.78 minutes. During PCNL two patients (both staghorn calculi) had intraoperative bleeding, due to which procedure was stopped in the middle and once patient was stable stone clearance was done with RIRS.
Total 8 patients had postoperative complications, fever was the most common (4 cases, 19%) haematuria in 2 cases (9.5%), paralytic ileus in 1 patient (4.8%) and drop in haemoglobin requiring blood transfusion in 1 patient (4.8%).
Complete clearance was obtained in 18 cases (85.7%), while 3 cases (14.3%) had residual calculi for which ancillary procedures were performed. Two patients underwent RIRS at the time of stent removal and complete clearance obtained, 1 patient underwent single session of postoperative ESWL. Major complications like bowel, splenic or liver injury were not noted in any of the cases or conversion to open surgery was not required in any of the cases. Outcomes of PCNL are summarised in [Table/Fig-9]. As per institutional protocol patients are followed-up with physical examination and ultrasound KUB and no symptoms and recurrence of stone detected till one year.
| PCNL outcomes | Mean±SD || Median (IQR) || Min-Max || Frequency (%) |
|---|
| Stone site, (%) | |
| Pelvis | 12 (57.1%) |
| Upper calyx | 6 (28.6%) |
| Isthmus | 1 (4.8%) |
| Staghorn | 3 (14.3%) |
| Access site | |
| Upper calyx | 16 (76.2%) |
| Upper calyx, Additional puncture | 5 (23.8%) |
| Procedure time (minutes) | 46.76±16.78 || 40.00 (14.00) || 25.00-90.00 |
| Intraoperative complications | |
| None | 19 (90.5%) |
| Bleeding | 2 (9.5%) |
| Postoperative complications: Any (Present) | 8 (38.1%) |
| Fever (Present) | 4 (19.0%) |
| Haematuria (Present) | 2 (9.5%) |
| Paralytic Ileus (Present) | 1 (4.8%) |
| Haemoglobin Fall+Blood transfusion (BT) (Present) | 1 (4.8%) |
| Duration of hospital stay (Hours) | 48.57±12.86 || 48.00 (12.00) || 36.00-72.00 |
| Pain score (postoperatively)Visual analogue pain score | 3.71±1.31 || 4.00 (1.00) || 2.00-6.00 |
| Ancillary procedure | |
| None | 16 (76.2%) |
| ESWL (2 pre op, 1 post op) | 3 (14.3%) |
| RIRS (post op) | 2 (9.5%) |
| Result | |
| Complete clearance | 18 (85.7%) |
| Incomplete clearance | 3 (14.3%) |
Discussion
Many different minimal invasive treatment modalities have been used to treat stones in HSKs, including SWL, ureteroscopy, PCNL, and open surgery. Although adequate fragmentation can be achieved by ESWL, yet the anatomic abnormalities may prevent fragment passage in a substantial number of patients. The overall stone-free rate has been only around 53% (range 50% to 79%) [9].
In various studies, PCNL is considered as the preferred treatment modality with minimal complications for large stones in HSK [13-15]. Because of its anatomical position upper pole and mid renal, but not the lower pole calyces, which are located posteriorly, are recommended for entry into pelvicalyceal system during PCNL [14]. In previous studies, the upper pole puncture was the first preference, because it allows access to the upper pole calices, renal pelvis, lower pole calices, pelviureteric junction and proximal ureter, thereby minimising nephroscope torque on renal tissue during manipulation [9,13]. Middle and lower calyceal manipulation is difficult and may require additional puncture for stone clearance. Flexible nephroscope is also recommends for PCNL in HSK [14]. Here supracostal puncture is a relatively safe access because upper pole lies below twelfth ribs. In the present study, the access to the kidney was through upper calyx in 76.2% of cases; whereas additional puncture was resorted to in 23.8% of cases, mostly through middle calyx. For stone fragmentation pneumatic swiss lithoclast was used and at times, holmium laser.
The chance of stone clearance by PCNL in HSK varies between 71.40% to 93% [17,19]. In present study, the preference for stone treatment in HSKs has been very much towards PCNL and the stone-clearance rate of 85.7%, with minimal complications, shows the safety and success of this approach at the study institution.
Three patients had residual stone fragment for which one patient had undergone ESWL and two patients had undergone RIRS before JJ stent removal.
Major complications such as colonic perforation, gall bladder injury, splenic injury and liver injury were stated in various studies [20-23]. The present study did not encounter any major complication. Only four patients developed postoperative pyrexia (Clavien Grade 1) [18] which were managed conservatively with antipyretics; in two patients intraoperative bleeding is encountered. Postoperatively, two patients had haematuria and one patient required blood transfusion. One patient developed paralytic ileus which was resolved conservatively.
There were no significant complications noted in the study. One of the patients had residual isthmic stones; that were in accessible using the regular rigid nephroscope. With use of extra long nephroscope and amplatz sheath chances of complete clearance are increased.
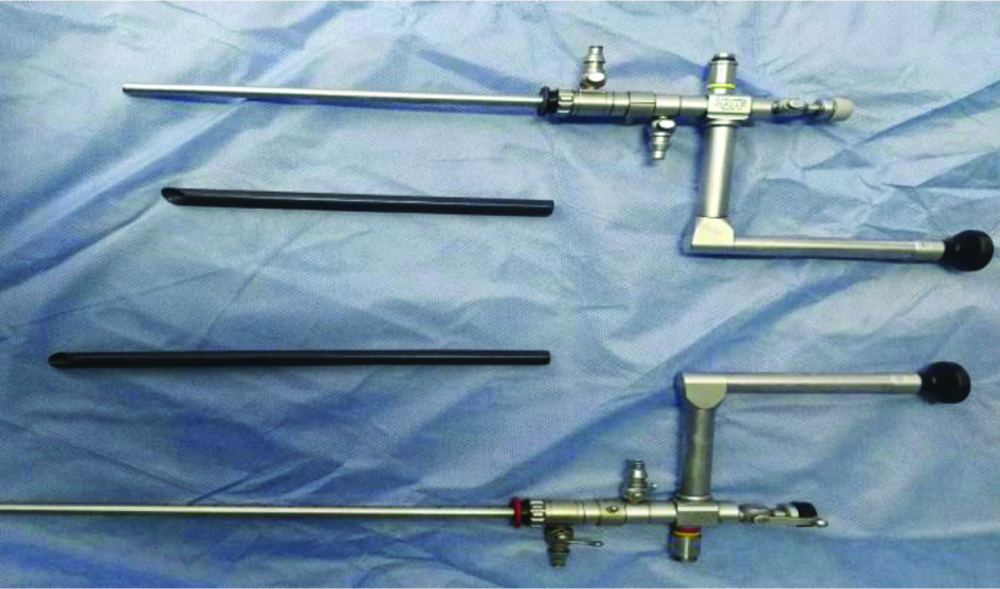
In HSK particularly for clearance of stone at isthmus extra long nephroscope and amplatz sheath needed [Table/Fig-10]. Razvi S and Zaidi Z performed PCNL in 16 patients, of which 12 patients (80%) achieved complete stone clearance after primary PCNL. Of the remaining 4 kidneys, 2 underwent re-look PCNL via the same tract and one more kidney was rendered stone-free. Hence, they achieved a stone clearance rate of 81% after primary and secondary PCNL and after auxiliary procedure to 93.7% [24]. Comparison of previously published series of PCNL in HSK with present series [Table/Fig-11] [19,24-27].
Extralong nephroscope and extralong amplatz sheath as compared to conventional ones.
Comparison of previously published series of Percutaneous Nephrolithotomy (PCNL) in Horseshoe Kidney (HSK) with present series
| Reference studies | Number of kidney units | Percentage upper pole access | Percentage complications (minor/major) | Percentage initial stone-free rate (without ancilliary procedure) |
|---|
| Symons S et al., [25] | 55 | 48 | 15/3 | 88 |
| Etemadian M et al., [19] | 21 | 66.64 | 14.28/0 | 85.68 |
| Razvi S et al., [24] | 14 | 80 | 21/0 | 81 |
| Jones DJ et al., [26] | 15 | Not available | 26 (20/6) | 72.3 |
| Vikram S et al., [27] | 23 | 100 | 3/0 | 87.50 |
| Present study | 21 | 76.2 | 7/1 | 85.7 |
A study by Symons S et al., PCNL in HSK showed the stone-free rate of 88%. The authors studied 67 renal units in 47 patient [25]. Etemadian M et al., performed PCNL on 21 patients with HSK stone. The stone-free rate with single session and rigid nephroscope was 71.40% [19]. Jones DJ et al., in 1991 performed PCNL on 18 renal unit of HSK and the stone free rate was 88.8% [26] In 2009, El Ghoneimy MN et al., had performed PCNL in 21 renal units of HSK, with higher SFR of 85.7% [14]. The study done in Mansoura University by Shokeir AA et al., presented their experience on 34 patients with 45 stone-bearing HSKs treated by PCNL in a period of 8 years, with higher SFR of 88% [28].
In 2018, Vikram S et al., had performed PCNL in 23 renal unit of HSK, with SFR of 87.50% [27]. There were no significant complications noted in the present study, with SFR of 85.7%; hence, it can be concluded that PCNL is efficacious in the management of nephrolithiasis in HSK.
Limitation(s)
The sample size is small, limiting the interpretations.
Conclusion(s)
PCNL can be recommended as the first line of management in the treatment of HSKs with large stone burden, considering its higher clearance rate and minimal complications. With use of extra long nephroscope and amplatz sheath chances of complete clearance are increased as with such instruments isthmus calculus also can be reached easily. However, external validation is required on a larger study.