Heat Intolerance and Hyperhidrosis as the only Presenting Manifestations of Acromegaly: A Case Report
TN Kamalesh1, HA Vijaya Sarathy2, NT Sreedevi3
1 Assistant Professor, Department of General Medicine, KVG Medical College and Hospital, Sullia, Karnataka, India.
2 Professor, Department of Endocrinology, Vydehi Institute of Medical Sciences and Research Centre (VIMS & RC), Bangalore, Karnataka, India.
3 Assistant Professor, Department of Otorhinolaryngology, KVG Medical College and Hospital, Sullia, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. TN Kamalesh, Assistant Professor, Department of General Medicine, KVG Medical College and Hospital, Kurnjibhag, Sullia-574327, Karnataka, India.
E-mail: tnkamalesh@gmail.com
Acromegaly is a state of Growth Hormone (GH) excess characterised by coarse facial features, acral enlargement, hyperhidrosis, headache, visual disturbances and visceromegaly. The most common cause of acromegaly is pituitary adenoma. The average delay between onset of symptoms and diagnosis is about six years in acromegaly owing to its subtle clinical features at the disease onset. Early diagnosis is important to reduce the morbidities and mortality associated with acromegaly. Familiarisation of physicians with the signs and symptoms of the disease is an effective strategy for the early diagnosis of acromegaly. Here, the authors report a case of 38year-old female patient. After proper clinical examination, history and series of relevant investigations, the serum GH level was estimated and was found to be elevated (40 ng/mL). GH secreting pituitary macroadenoma presenting with heat intolerance and hyperhidrosis without the classical manifestations of acromegaly.
Excessive sweating, Growth hormone, Headache, Sellar mass
Case Report
A 38-year-old house maker, a mother of two children, presented to Department of General Medicine with troublesome heat intolerance for five years, even forcing her to sleep on the floor, even during cold climate and which was persistent throughout the day and across all the seasons. This was accompanied by excessive sweating, not profuse though. There was no accompanying fever, increased anxiety, increased bowel movement, decreased sleep, weight loss and menstrual irregularities. On enquiry, she also had diffuse dull headache for last 10 years with no visual or otorhinologic disturbances or clear aggravating and relieving factors. Recently, she was diagnosed to have pre-diabetes and was on life style modification for the same. She did not have any other comorbidities. She had uneventful obstetric history and no similar illness in the family.
On examination, she was well-built and well-nourished with a body mass index of 26.45 kg/m2. Her palpebral conjunctiva was pale and she was normothermic and normotensive with a regular normovolemic pulse rate of 86 beats per minute. She appeared diaphoretic with sweaty hands and forehead. Thyroid gland was diffusely enlarged with no bruit. There were no clinical signs of thyrotoxicosis. Thorough examination did not reveal any clinical abnormalities except for doubtful stubby nature of fingers of both the hands [Table/Fig-1] and mild coarsening of face.
Clinical photograph of both hands of the patient demonstrating subtle acral enlargement.

She had been previously (one year ago) investigated thoroughly which revealed iron deficiency anaemia as the only laboratory abnormality. Euthyroid state of the patient had been documented several times. So, it was decided to evaluate for other causes of her symptoms. Haemogram revealed haemoglobin of 9.2 g/dL with microcytic hypochromic erythrocytes with normal leucocyte and platelet count. Erythrocyte sedimentation rate was normal. Random plasma glucose and glycosylated haemoglobin were 148 mg/dL and 6.4% respectively. Patient had low serum iron (28 μg/dL) and ferritin (7.9 ng/mL) levels and increased Total Iron Binding Capacity (TIBC) (536 μg/dL) and transferrin (436 mg/dL) levels. Stool test for occult blood was negative. Renal function tests and serum electrolyte levels were unremarkable. Patient was non-reactive for retroviral infection. Ultrasonography of thyroid showed enlargement of the gland with increased vascularity with no nodules. In view of subtle evidence of acromegaly, serum GH level was estimated and was found to be elevated (40 ng/mL). Further workup was performed with estimation of serum Insulin-like Growth Factor (IGF-1) and serum prolactin levels and GH suppression with 75g oral glucose load. The test results (which were done preoperatively in our hospital) were suggestive of GH excess and are summarised in [Table/Fig-2].
Summary of Preoperative laboratory evaluation for Growth Hormone (GH) excess state.
| Test | Observed value | Normal reference range |
|---|
| S. IGF-1 | 784.06 ng/mL | 109.00-284.00 ng/mL |
| S. Prolactin | 33.15 ng/mL | 2.80-29.20 ng/mL |
| S. Growth hormone (75g oral glucose suppression test) | Basal | 40.00 ng/mL | 0.00-18.00 ng/mL |
| 1 hour | 28.60 ng/mL | <1 ng/mL |
| 2 hour | 23.00 ng/mL | <1 ng/mL |
S.IGF: Serum insulin-like growth factors; S. Prolactin: Serum prolactin
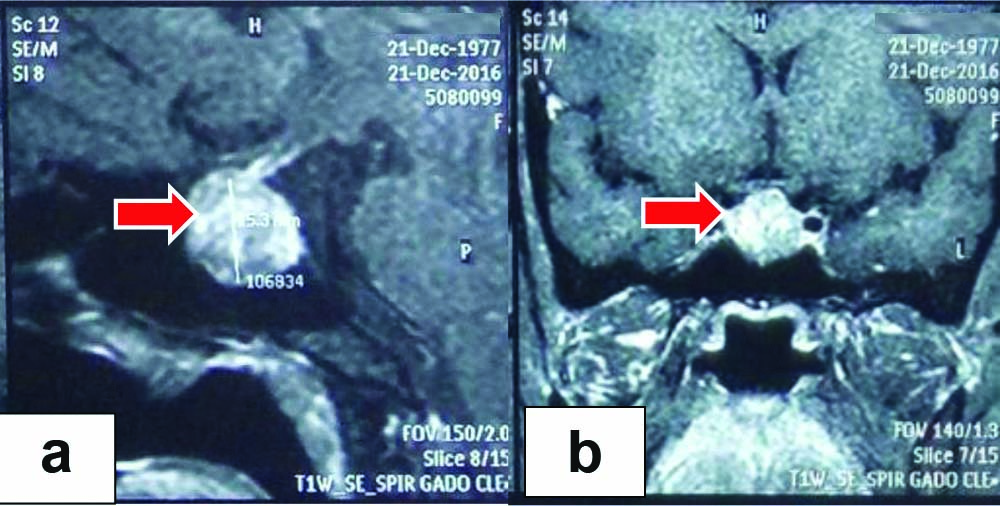
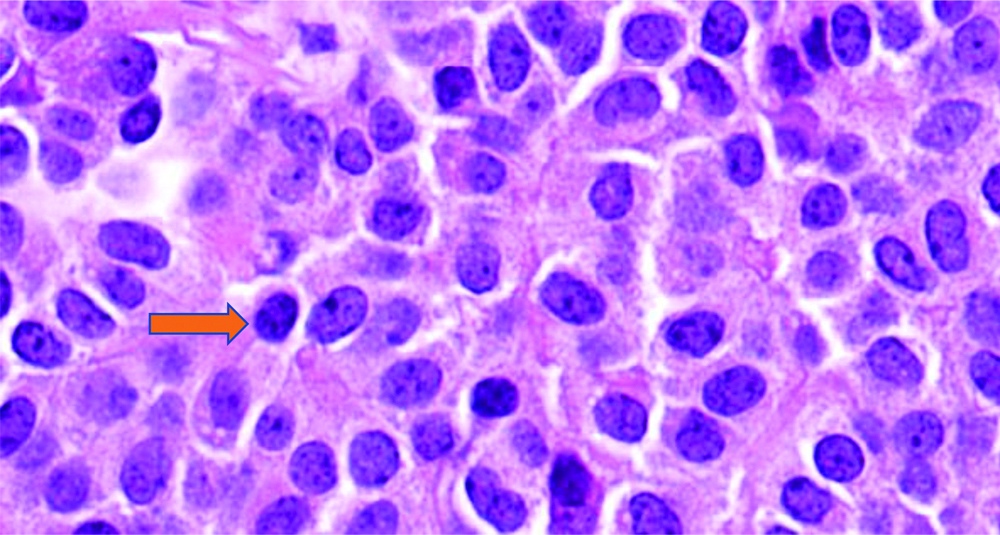
Magnetic Resonance Imaging (MRI) of pituitary revealed a well-defined sellar mass lesion measuring 20×15×40 mm and suggestive of pituitary macroadenoma [Table/Fig-3a,b]. Visual field analysis (perimetry) was normal. One week later, patient underwent trans-sphenoidal excision of the mass after confirming the suitable nose and paranasal anatomy by Computed Tomography (CT) of the paranasal sinuses. Surgery was uneventful and histopathology confirmed the lesion as pituitary adenoma [Table/Fig-4]. Patient had a dramatic relief from the symptoms. Random serum GH level, a month later was 3.07 ng/mL. Further evaluation with serum IGF-1 and MRI pituitary were advised three months later. Patient was discharged with oral corticosteroids (to continue) and acetazolamide (for one week). On follow-up after three months, patient had significant resolution of symptoms with normal serum IGF-1 (201.02 ng/mL) and no residual pituitary sellar mass lesion on MRI.
Magnetic resonance imaging of the pituitary revealing sellar mass (shown by arrows) which heterogeneously enhanced after gadolinium contrast (sagittal: 3A, coronal: 3B).
Histopathology of excised tissue which revealed densely eosinophilic somatotropes on 400X resolution microscopy.
Discussion
The GH is produced by somatotropes of anterior pituitary and its excess results in insidious onset of manifestations related to soft tissue and bone [1]. GH excess can result in gigantism (if it occurs before the closure of epiphyses) or acromegaly (if it occurs after the closure of epiphyses) [2].
Acromegaly is a rare condition with an incidence of 3.3 per million per year [3]. Pituitary adenoma accounts for more than 99% of GH excess [4]. GH stimulates synthesis of IGF-1 from liver which stimulates proliferation of dermal fibroblasts, sebaceous glands and sweat glands [4]. It manifests with a wide range of non-specific signs and symptoms. They include rheumatological (broadening of face, hand and feet, frontal bossing, prognathism, teeth separation, jaw malocclusion, entrapment neuropathies, dorsal kyphosis), the cardiovascular (arterial hypertension, hypertrophic cardiomyopathy and increased risk of valvular disease), the respiratory (obstructive sleep apnea, chest deformities and poor respiratory muscle strength), the metabolic (insulin resistance, hypercalciuria and renal stones), the gastrointestinal (increased risk of colon malignancy, colon polyps and hepatomegaly) and the cutaneous (malodorous sweating and oily skin) manifestations that are due to long term effects of GH/IGF-1 [3,5,6]. Disproportionate enlargement of fingertips leads to a drumstick-like appearance of fingers and toes [7]. Headaches and visual field defects are the most common but late symptoms produced by the local effect of the tumour (usually macroadenoma) [3]. However, all acromegaly patients do not present with classic manifestations. Hence, physicians should have high suspicion for acromegaly even in patients presenting with only few or less-classic manifestations.
Heat intolerance and hyperhidrosis are one of the manifestations of acromegaly [4]. Hyperhidrosis is a frequently described, though rare as the only presenting manifestation whereas heat intolerance is a less frequent manifestation of acromegaly [8,9]. Though this patient had the classical features such as acral enlargement and coarsening of facial features, they were subtle and were missed during multiple presentations to several physicians. The latter classical features were recognised in this patient only after the presenting symptoms remained unexplained by multiple investigations and the rarer causes such as acromegaly were thought of.
Pituitary surgery is the first line treatment in patients with microadenomas as well as macroadenomas [5,10]. Microadenomas (<10 mm) are more amenable for complete excision with high cure rates whereas cure rates for macroadenomas (≥10 mm) are less. Though there was rapid improvement of symptoms and large reduction in random GH levels after surgery, a random GH level of 3 ng/mL a month after surgery indicates the possibility of a residual tumour tissue with persistent disease. However, this requires further evaluation with serum IGF1 and repeat MRI pituitary at three months after surgery. Therapeutic options in patients with persistent disease include repeat surgery, radiotherapy and medical therapy (dopamine agonists, somatostatin analogues or GH receptor antagonists) which should be individualised [11-13].
Patients with acromegaly have increased all-cause mortality, compared with the general population, even after surgical excision [14]. Important determinants of mortality are cardiovascular disease (60%), respiratory disease (25%) and neoplasia (15%) [15]. Association with various morbidities and increased mortality emphasises the needs for early diagnosis of acromegaly but varied and overlapping clinical presentation makes it a challenging task which warrants high degree of clinical suspicion for the disease.
Euthyroid diffuse or multinodular goiter is a common feature in patients with acromegaly. Iron deficiency anaemia in this patient may due to intermittent per-rectal bleeding from colonic polyposis which is more common in acromegaly patients. Hence, this patient has been suggested to undergo colonoscopy to rule out colonic polyposis.
Conclusion(s)
The authors reported a case of acromegaly, due to pituitary macroadenoma, who presented with heat intolerance and hyperhidrosis with very subtle clinical evidence of acromegalic features. We suggest that patients with heat intolerance and/or excessive sweating should be evaluated for GH excess status despite no/subtle features of acromegaly, especially in those with euthyroid status.
S.IGF: Serum insulin-like growth factors; S. Prolactin: Serum prolactin
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 05, 2020
Manual Googling: Nov 09, 2020
iThenticate Software: Dec 14, 2020 (7%)
[1]. Lause M, Kamboj A, Fernandez Faith E, Dermatologic manifestations of endocrine disordersTransl Pediatr 2017 6(4):300-12.10.21037/tp.2017.09.0829184811 [Google Scholar] [CrossRef] [PubMed]
[2]. Abe T, Tara LA, Lüdecke DK, Growth hormone-secreting pituitary adenomas in childhood and adolescence: Features and results of transnasal surgeryNeurosurgery 1999 45(1):01-10.10.1227/00006123-199907000-00001 [Google Scholar] [CrossRef]
[3]. Caron P, Brue T, Raverot G, Tabarin A, Cailleux A, Delemer B, Signs and symptoms of acromegaly at diagnosis: The physician’s and the patient’s perspectives in the ACRO-POLIS studyEndocrine 2018 63(1):120-29.10.1007/s12020-018-1764-430269264 [Google Scholar] [CrossRef] [PubMed]
[4]. Jabbour SA, Cutaneous manifestations of endocrine disorders: A guide for dermatologistsAm J Clin Dermatol 2003 4:315-31.10.2165/00128071-200304050-0000312688837 [Google Scholar] [CrossRef] [PubMed]
[5]. Chanson P, Salenave S, Kamenicky P, AcromegalyHandb Clin Neurol 2014 124(5):197-219.10.1016/B978-0-444-59602-4.00014-925248589 [Google Scholar] [CrossRef] [PubMed]
[6]. Renehan AG, O’Connell J, O’Halloran D, Shanahan F, Potten CS, O’Dwyer ST, Acromegaly and colorectal cancer: A comprehensive review of epidemiology, biological mechanisms, and clinical implicationsHorm Metab Res 2003 35:712-25.10.1055/s-2004-81415014710350 [Google Scholar] [CrossRef] [PubMed]
[7]. Rustin MH, Andrews’ diseases of the skin-clinical dermatologyPostgrad Med J 1990 66(781):98410.1136/pgmj.66.781.984 [Google Scholar] [CrossRef]
[8]. Martín Suárez I, Carrasco Sánchez FJ, Suárez Marrero MC, Cuesta López F, Pujol de la L, Lave E, Hiperhidrosis severa como forma de presentación de la acromegalia [Acromegaly presenting with severe hyperhidrosis]An Med Interna 2003 20(12):659-60.10.4321/S0212-7199200300120001914697096 [Google Scholar] [CrossRef] [PubMed]
[9]. Kjellberg RN, Shintani A, Frantz AG, Kliman B, Proton-beam therapy in acromegalyN Engl J Med 1968 278(13):689-95.10.1056/NEJM1968032827813014966299 [Google Scholar] [CrossRef] [PubMed]
[10]. Adelman DT, Liebert KJ, Nachtigall LB, Lamerson M, Bakker B, Acromegaly: The disease, its impact on patients, and managing the burden of long-term treatmentInt J Gen Med 2013 6:31-38.10.2147/IJGM.S3859423359786 [Google Scholar] [CrossRef] [PubMed]
[11]. Abs R, Verhelst J, Maiter D, Acker KV, Nobels F, Coolens JL, Cabergoline in the treatment of acromegaly: A study in 64 patientsJ Clin Endocrinol Metab 1998 83:374-78.10.1210/jcem.83.2.45569467544 [Google Scholar] [CrossRef] [PubMed]
[12]. Bruns C, Lewis I, Briner U, Meno-Tetang G, Weckbecker G, SOM230: A novel somatostatin peptidomimetic with broad somatotropin release inhibiting factor (SRIF) receptor binding and a unique antisecretory profileEur J Endocrinol 2002 146:707-16.10.1530/eje.0.146070711980628 [Google Scholar] [CrossRef] [PubMed]
[13]. Kopchick JJ, Parkinson C, Stevens EC, Trainer PJ, Growth hormone receptor antagonists: Discovery, development, and use in patients with acromegalyEndocr Rev 2002 23(5):623-46.10.1210/er.2001-002212372843 [Google Scholar] [CrossRef] [PubMed]
[14]. Dekkers OM, Biermasz NR, Pereira AM, Romijn JA, Vandenbroucke JP, Mortality in acromegaly: A metaanalysisThe Journal of Clinical Endocrinology & Metabolism 2008 93(1):61-67.10.1210/jc.2007-119117971431 [Google Scholar] [CrossRef] [PubMed]
[15]. Holdaway IM, Rajasoorya RC, Gamble GD, Factors influencing mortality in acromegalyJournal of Clinical Endocrinology and Metabolism 2004 89(2):667-74.10.1210/jc.2003-03119914764779 [Google Scholar] [CrossRef] [PubMed]