Spinal anaesthesia is still widely performed using a landmark guided approach. This being a blind technique may lead to multiple attempts causing pain, paraesthesias and injury to the neural structures, increasing morbidity and decreasing overall patient satisfaction [1,2]. Real time ultrasound guided neuraxial blockade has the advantage of visualisation of needle trajectory and ability to adjust according to changes in patient position, but it is technically challenging [3]. PUS has been shown to increase the success rate of dural puncture at first attempt [4]. There is still scarcity of data to recommend routine use of ultrasound for neuraxial blockade with conflicting results in different studies [5-8]. Of the various views, Parasagittal Oblique (PSO) view and the Transverse Interspinous (TI) view offer a wide window of the anatomy of spine. Furthermore, the acoustic window of PSO view is better than TI view [9].
In the current study, it was hypothesised that PUS guided paramedian technique can increase the success rate at first attempt when compared to landmark based midline approach. The primary outcome of this study was the rate of successful dural puncture at first attempt and secondary outcomes were number of needle insertion attempts and passes required for successful dural puncture, time taken for the entire procedure, block associated pain and periprocedural comfort of the patient and any complication like blood in spinal needle, radicular pain or paraesthesia during the procedure. The relation between the quality of acoustic window and success of dural puncture was also analysed.
Materials and Methods
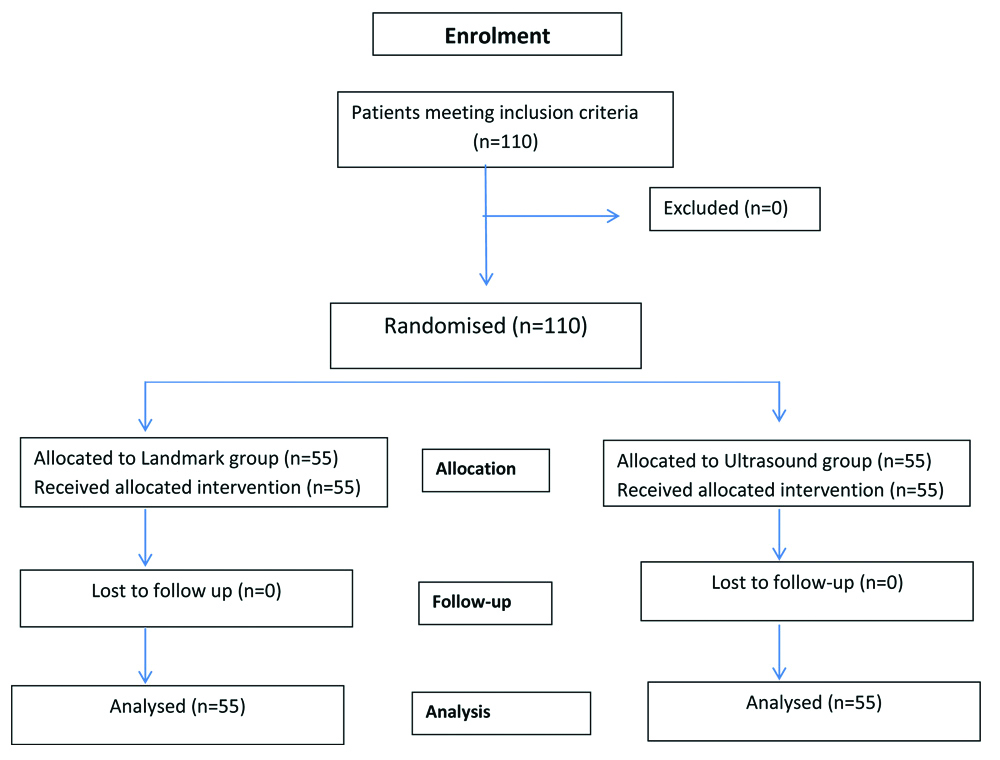
This was a randomised clinical study, conducted at a Tertiary Care Hospital during May 2017-December 2018. Hospital Ethics Committee approval (S.No.IEC/VMMC/SJH/Oct/2016) was taken. A total of 110 patients were enrolled in the study.
Inclusion criteria: American Society of Anaesthesia (ASA) physical status I-III patients, aged 18-60 years of either sex, with Body Mass Index (BMI) less than 35 kg/m2 undergoing lower limb orthopaedic surgery.
Exclusion criteria: BMI ≥35 kg/m2, previous spine surgery, coagulopathy and any other contraindication to neuraxial blockade.
After obtaining written informed consent, they were randomised into two groups: group LM, landmark based midline approach and group US, PUS guided technique with paramedian approach, using block randomisation technique. Patients were randomised in blocks of ten i.e., for every ten patients randomised, five received landmark based midline spinal block and five received PUS guided paramedian spinal block. In the operation theatre, monitors were attached to record vital parameters like electrocardiogram, non-invasive blood pressure and pulse oximeter, and an intravenous line was secured.
The PUS was performed by a resident anaesthesiologist in all cases, under the guidance of an experienced anaesthesiologist with atleast two years experience in spine ultrasound. Spinal anaesthesia was performed in both the groups by the same resident anaesthesiologist to avoid bias caused by difference in expertise and experience. The observations were recorded by an observer different from the resident and the supervisor. Blinding could not be done due to the nature of study.
Landmark group: Spinal anaesthesia was performed in sitting position. The quality of surface landmarks was graded according to age, Body Mass Index (BMI), ability to palpate bony landmarks and spinal bony deformity, if any, using MM Atallah difficulty score [10]. The interspace below L2 vertebra, that appeared widest on manual palpation, was chosen for the first attempt. The subarachnoid block was performed with 25 gauge Quincke’s needle. Once dural puncture was confirmed by flow of clear Cerebrospinal Fluid (CSF) from the needle hub, 15 mg (3 mL) of hyperbaric 0.5% bupivacaine was injected.
Ultrasound group: PUS was performed in sitting position using a portable ultrasound system equipped with a 2-5 MHz curved array probe (KONTRON). The PSO view was used to identify sacrum as a linear hyperechoic structure followed by the first dip allowing definitive identification of the L5-S1 level. Using this level as a starting point, we identified the L4-L5, L3-L4 and L2-L3 level subsequently.
Interlaminar spaces were identified as soft tissue acoustic windows that allowed imaging of deeper midline structures such as Ligamentum Flavum-Dura mater (LFD) complex and the Posterior Longitudinal Ligament (PLL), which represented the anterior and posterior limit of the intrathecal space, respectively. The level at which the soft tissue structures of the vertebral canal were best visualised, four points were marked, two coinciding with the centre of upper and lower horizontal surface of the probe and the other two points coinciding with the midpoint of the right and left lateral vertical surface of the probe. The puncture site was determined by the intersection of the four marks on skin. The level at which the best parasagittal view was obtained, the probe was rotated 90° and centered on the midline to obtain transverse views of spine. Using TI view, the midline of the spine was marked, which helped in directing the needle towards midline [Table/Fig-1].
a,b: L3-L4 interlaminar space.
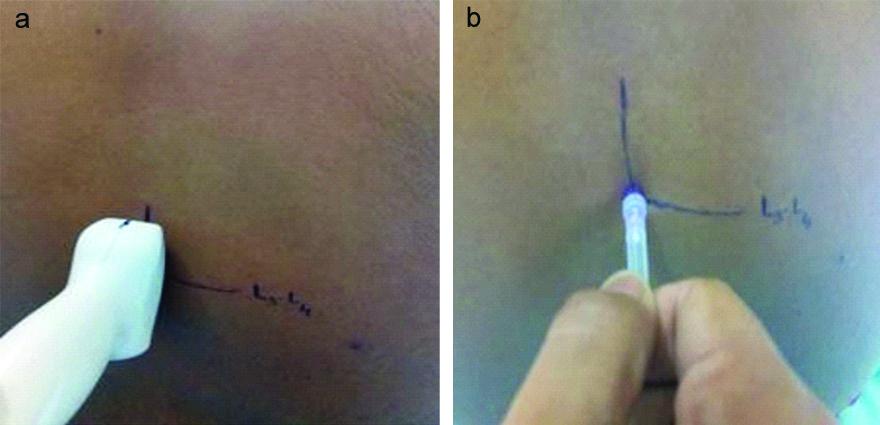
Spinal needle was inserted through the marked point, keeping in mind the angulation of the probe in PSO view. After successful dural puncture, same anaesthesia procedure was followed as described in landmark based midline group.
Primary outcome: Success rate of dural puncture at first attempt was the primary outcome. It was analysed as the percentage of cases in which free flow of CSF was obtained in first attempt out of total (n=55) in each group.
Secondary outcomes:
1) Total number of needle insertion attempts and passes required for dural puncture were recorded for each case in both the groups.
2) Time taken to establish landmarks: In LM group, this was the period beginning when the operator first touched the patient and ended when operator declared the examination to be complete. In US group, this was defined as the period beginning when the probe was first placed on the patient and ended when the operator declared the examination as complete.
3) Time taken to perform spinal anaesthesia was the period between the insertion of the needle through the skin, till withdrawal of spinal needle after injection of the anaesthetic solution.
4) Total procedure time was the sum of the time taken to establish landmarks and that taken to perform the spinal anaesthesia.
5) Block associated pain score was rated by patients on an 11 point numerical scale (0-10) with taking zero as no pain, and ten as worst possible pain.
6) Patient satisfaction with the block procedure, was rated by the patient on a 5 point numerical scale (5=very good, 4=good, 3=satisfactory, 2=unpleasant, 1=very unpleasant).
7) Quality of the images at each intervertebral level was defined in terms of the ability to visualise the LFD and PLL. If both the LFD and PLL were visible, the view was classified as good. If only the PLL or LFD was visible, the view was classified as intermediate. If neither the LFD nor the PLL was visible, the view was classified as poor [4]. The quality of surface landmarks was graded accordingly [10].
8) Any complications like blood in spinal needle, incidence of radicular pain or paraesthesia while performing the block were noted.
Statistical Analysis
Using the observations of a previous study as reference, where success rate at first attempt was 60% in landmark group and 84% in ultrasound group, the minimum required sample size with 80% power of study and 5% level of significance was 52 patients in each study group [7]. Categorical variables are presented as numbers and percentages (%) and continuous variables as mean±SD and median. Quantitative variables were compared using unpaired t-test/Mann-Whitney U test. Qualitative variables were compared using Chi-Square test/Fisher’s exact test. A p-value <0.05 was considered as statistically significant. The data was entered in MS Excel spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
Results
A total of 110 patients were enrolled with 55 patients in each group [Table/Fig-2]. The distribution of demographic data and Atallah MM difficulty score was similar in two groups. The success rate of dural puncture at first attempt was 89.09% in US group and 76.36% in LM group, p=0.077. The mean number of needle insertion attempts in LM group was 1.31±0.63 versus 1.11±0.31 in US group, p=0.066 [Table/Fig-3]. Successful dural puncture was achieved in all the cases within 8 needle passes in US group as compared to 13 passes in LM group [Table/Fig-4].
Age, BMI, Atallah score, number of attempts and time to landmark identification were analysed using Unpaired t-test. Gender and first attempt success rates were compared using Chi-square test.
| Variables | Group LM (mean±SD) | Group US (mean±SD) | p-value |
|---|
| Age (years) | 38.96±14.59 | 38.87±13.75 | 0.938 |
| Sex | Male | 39 (29.09%) | 38 (30.91%) | 0.835 |
| Female | 16 (70.91%) | 17 (69.09%) |
| BMI (kg/m2) | 25.32±2.96 | 25.56±3.38 | 0.76 |
| Atallah difficulty score | 1.82±1 | 1.84±1.18 | 0.949 |
| Time for landmark identification (minutes) | 0.38±0.2 | 9.39±1.28 | 0.0001 |
| Number of successful dural puncture in first attempt | 42 (76.36%) | 49 (89.09%) | 0.077 |
| Number of needle insertion attempts | 1.31±0.63 | 1.11±0.31 | 0.066 |
p<0.05 considered significant
Number of needle passes for successful dural puncture in group LM and group US.
| Successful dural puncture | Group | p-value |
|---|
| LM | US |
|---|
| On 1st needle pass | 15 (27.27%) | 23 (41.82%) | 0.109 |
| Within 5 needle passes | 45 (81.82%) | 51 (92.73%) | 0.151 |
| Within 8 needle passes | 53 (96.36%) | 55 (100.00%) | 0.495 |
| Within 13 needle passes | 55 (100.00%) | 55 (100.00%) | - |
| No. of passes (mean±SD) | 3.11±2.48 | 2.24±1.60 | 0.047 |
Were analysed using Unpaired t-test; p<0.05 considered significant
The time taken to establish landmarks in US group (9.39±1.28 minutes) was significantly higher than that in LM group (0.38±0.2 minutes) with p=0.0001. The time taken for spinal anaesthesia in LM group (2.88±0.52 minutes) was higher as compared to that in US group (2.59±0.5 minutes), p=0.004, which was statistically significant. The total procedure time in LM and US group was 3.26±0.68 minutes and 11.96±1.55 minutes, respectively, p=0.0001.
The pain score was lower in US group (1.74±0.67) as compared to LM group (2.09±0.65), p=0.007. The patient satisfaction score was comparable between LM group (4.02±0.68) and US group (4.09±0.65), p=0.63 [Table/Fig-5]. First attempt success rate was found to be 95.83% if the quality of PSO view was good and 42.86% if the quality of PSO view was intermediate (p=0.001) [Table/Fig-6]. None of the patients had any complications like blood in CSF, radicular pain or paraesthesia.
Comparison of periprocedural pain and patient satisfaction scores between group LM and US.
| Variable | Group LM | Group US | p-value |
|---|
| Periprocedural pain score (0-10) | Mean±SD | 2.09±0.65 | 1.74±0.67 | 0.007 |
| Median | 2 | 2 |
| Min-Max | 1-4 | 1-3 |
| Interquartile range | 2-2 | 1-2 |
| Periprocedural comfort score (1-5) | Mean±SD | 4.02±0.68 | 4.09±0.65 | 0.63 |
| Median | 4 | 4 |
| Min-Max | 2-5 | 3-5 |
| Interquartile range | 4-4 | 4-4.75 |
Were analysed using Unpaired t-test; p<0.05 considered significant
Correlation between the quality of PSO view and successful dural puncture in US group.
| PSO view | Total | p-value |
|---|
| Good | Intermediate |
|---|
| Total no. of attempts | 01 | 46 | 03 | 49 | 0.001 |
| 02 | 02 | 04 | 06 |
| Total | 48 | 07 | 55 |
Was analysed using Fischer’s exact test; p<0.001 considered highly significant
Discussion
The primary aim of this study was to examine whether PUS guided paramedian approach leads to a higher success rate of dural puncture in first attempt as compared to the conventional landmark guided midline approach. The PUS guided paramedian approach did not increase the rate of successful dural puncture in first attempt in patients undergoing lower limb orthopaedic surgery, the time taken for the procedure was much longer than the conventional midline landmark approach, periprocedural pain was lower in US group and patient comfort level was comparable between the two groups.
In a previously conducted study, the first attempt success rate was significantly greater in ultrasound group (paramedian approach) versus landmark group with a midline approach (84% versus 60%, p=0.0075) [11]. This could be due to the fact that the study involved older population (mean=68.2 years) where the degenerative changes in spine like calcified ligaments and reduced intervertebral spaces make an ultrasound guided paramedian approach more feasible than midline blind approach. Another study compared PUS guided paramedian technique with landmark guided paramedian approach due to the fact that paramedian approach is considered easier in elderly population due to midline calcified ligaments. They also observed that the first attempt success rate was much higher in PUS guided group than conventional group (65% versus 17.5%, respectively) [12]. This study showed that the acoustic window provided by the ultrasound is helpful in accurately guiding the needle insertion site and path, leading to lesser number of attempts. This is in contrast to the findings in a study where the preprocedural USG- guided paramedian approach at L5-S1 level was compared with conventional landmark guided midline technique in elderly population. It was reported that the first pass success rate was higher in conventional as compared to ultrasound guided technique (43% versus 22%, p=0.02) [5]. This observation can be attributed to L5-S1 space, being the widest and least affected by positioning. Also, during ultrasound, it is the most misidentified space due to various reasons. These reports suggest that PUS could be useful in elderly patients where landmark technique becomes difficult due to age related anatomical changes in spine.
In another study, midline landmark technique was compared with PUS guided midline and PUS guided paramedian approach in elderly (>60 year) population. They observed a comparable first attempt success rate in midline landmark and PUS guided midline technique (77% and 73%, respectively) and a lower success rate in PUS guided paramedian technique (42%, p<0.001). The fact that the procedure in this study was conducted by residents (with experiance less than a year) could have a bearing on the lower success rate of PUS guided paramedian approach. Also, the nature of surgery was not necessarily orthopaedic, hence the difficulty encountered in positioning might have not been there, limiting the advantage of ultrasound in midline technique and leading to comparable results [13].
The study population in the current study was much younger (mean age=39 years), so the anatomical difficulties encountered were not as seen in the elderly age group. The MM Atallah difficulty score was also comparable between the two groups.
Lim YC et al., also conducted a trial of ultrasound guided (paramedian) spinal anaesthesia wherein there was no significant difference in first attempt success rates between ultrasound and conventional group (62% versus 52%, p=0.16), which was similar to our study. Their study population was older but included a variety of surgeries and not just joint replacements [6].
Abdelhamid SA and Mansour MA, on the other hand found a significant difference in first attempt success rates (80% in ultrasound guided midline versus 37% in conventional midline) in a rather young population (mean age=34 years) but they have not mentioned the nature of surgery [7]. They also reported quality of landmark assessed to be significantly better in their ultrasound group as compared to landmark group, which could be the cause of these skewed results. Bias could also have occured due to difference in experience and level of expertise of the anaesthetist performing ultrasound guided as well as landmark guided technique which is not mentioned in the study.
Dhanger S et al., reported a higher success rate in first attempt and first pass (96% and 74%, respectively) in ultrasound group as compared to landmark group (30% and 18%, respectively). They also reported decreased incidence of paraesthesia in ultrasound group as compared to conventional method. Their study population included obstetric patients scheduled to undergo elective caesarean section in whom spinal anaesthesia is technically difficult due to exaggerated lumbar lordosis and difficult patient positioning [8].
The total number of attempts (needle withdrawn completely from the skin and reinsertion) were comparable in both the groups whereas the total number of needle passes for successful dural puncture was significantly lower in US group i.e., 2.24±1.6 in US versus 3.11±2.48 in LM group, p=0.47, in the present study. Srinivasan KK et al., also observed less number of passes in ultrasound group than conventional group (8 versus 4, p=0.01) [11]. Similar finding was recorded by a study wherein the mean number of passes were lower in PUS guided group as compared to traditional landmark group (1 versus 4.5, respectively) [12].
The time taken for landmark assessment in present study was 9.39 minutes in US group as compared to 0.38 min in LM group which resulted in increased duration of total procedure in US group [Table/Fig-1]. This can be explained by the fact that, US was performed in PSO view and TM view in all the lumbar intervertebral spaces by a resident with a limited experience in spinal ultrasound. In the study by Lim YC et al., time taken for the procedure was less in ultrasound group as compared to landmark group (2.9 minutes versus 3.9 minutes, p=0.007) [6]. The difference is reflective of the ongoing learning curve in performing ultrasound guided procedures and is expected to decrease with more experience in future. Dhanger S et al., noticed a significantly higher time to locate the interspinous space but decrease in total procedure time in USG group. This could be probably due to difficulty in accurately identifying the interspinous space in obstetric patients [8].
In the current study, block associated pain score was significantly less in US group as compared to LM group (1.74±0.67 versus 2.09±0.65). This may be attributed to the fact that, the needle insertion point and the needle direction were identified by pre-procedural US and required less number of needle passes in US group as compared to LM group.
Previous two studies documented that the peri-procedural numerical score for pain was comparable between the two groups, with p-value of 0.99 and 0.59, respectively [5,11]. The number of passes and attempts were similar in the two groups in one study [5] and in the other, though statistically significant the number of attempts were clinically similar (1.98 in LM and 1.28 in US group) [11].
In this study, patient satisfaction scores (5=very good, 1=very unpleasant) were comparable in both groups. Similar results were seen in previous studies [5,11]. None of the patients had vascular puncture, paraesthesia or postdural puncture headache.
In this study, it was found that the success rate of dural puncture at first attempt was 95.8% when the acoustic window was good (both LF and PLL visible) as compared to intermediate (LF or PLL only), which yielded 42.8% success rate at first attempt. This observation has the implication that if a good PSO view of the vertebral canal (defined as visualisation of both LF and PLL) can be obtained with ultrasound at a given intervertebral level, it is highly probable that dural puncture via a paramedian approach can be achieved without significant technical difficulty. This is not surprising, given that the presence of good ultrasound view implies a sufficiently large interlaminar and interspinous soft tissue acoustic window into the vertebral canal, through which a needle should pass without difficulty [4].
Limitation(s)
The main limitation of this study is that the scan was performed before the procedure for marking the needle insertion site. Patient re-positioning during the actual procedure leads to inaccuracy due to the change in the position of skin marking with respect to the actual path as seen by ultrasound. A real time performance of ultrasound during the needle insertion may improve the accuracy of puncture site. Another limitation is that blinding could not be done due to the difference in approach (paramedian in US and midline in LM group) and presence of skin markings in the ultrasound group. Furthermore, the experience of the anaesthesiologist performing the ultrasound and spinal anaesthesia was limited; with more experience, the time required to perform the PUS guided spinal block may reduce and may also have an increased rate of successful dural puncture at first attempt.
Conclusion(s)
Pre-procedural USG guided paramedian approach does not increase the success rate at first attempt as compared to midline landmark guided approach, in patients without any anatomic spinal abnormality.
p<0.05 considered significant
Were analysed using Unpaired t-test; p<0.05 considered significant
Were analysed using Unpaired t-test; p<0.05 considered significant
Was analysed using Fischer’s exact test; p<0.001 considered highly significant