Acute pancreatitis is an inflammatory disease of the pancreas, and is one of the most common causes of hospitalisation among gastrointestinal diseases [1]. The inflammation may be localised to pancreas, or disseminate to adjacent tissues and can also involve other organ systems [2]. AP is capable of a wide clinical presentation, ranging from mild abdominal pain to death [3]. Early prediction in severity of pancreatitis would help in decision on mode of management thereby reducing the complications and organ dysfunction [4].
There are various scoring systems which are helpful in identifying the severity of the disease and patients at high risk for complications. Haematocrit, a low cost and easily accessible test is considered as an early predictor for identifying the severity of AP. It is also helpful in assessing risk stratification and early transfer to ICU [5]. The fall in haematocrit of more than 10% within 48 hours in AP has been documented as a diagnostic predictor in few studies [5-7].
The use of Glasgow scoring in assessing the prognosis of AP is well known. However, Modified Glasgow scoring, when compared in predicting the severity of pancreatitis with other scoring systems, has failed to produce statistically significant results [8-10]. CT of abdomen done at 48-72 hours after the acute attack gives an accurate extent of pancreatic necrosis and its complications with a CTSI score. CTSI score is calculated based on pancreatic inflammation, necrosis and extra-pancreatic complications. CTSI scoring has significant correlation with clinical outcome parameters, as well as good concordance with grading of severity in AP as per revised Atlanta classification [11].
Although, Haematocrit, Modified Glasgow scoring and CT abdomen have been employed in the past to assess the severity of AP with good outcomes, no single study has been done comparing these three prognostic indicators on the same patient at a given time. The aim of this study was to evaluate and compare the efficacy of Haematocrit, Modified Glasgow scoring and CT abdomen as prognostic markers in prediction of LOHS, need for ICUA, OF, and mortality in AP.
Materials and Methods
A prospective longitudinal study was done on 120 patients diagnosed with AP over a period of 18 months between April 2018 to September 2019 in a tertiary care hospital. The study was commenced after Institutional Ethics Committee clearance with ethical approval number (IEC-1385) dated 25th April, 2018. The sample size was calculated as per the formula n=4pq/L2; taking prevalence as 45% based on a study conducted by Yadav D and Lowenfels AB, on the epidemiology of pancreatitis and pancreatic cancer [12]. The study has been reported according to the STROCSS criteria [13].
Inclusion criteria: Patients diagnosed as AP with onset of pain in 24 hours were included in the study.
Exclusion criteria: Patients with chronic pancreatitis, recurrent pancreatitis, known pancreatic anomalies and those that presented after 24 hours from the onset of pain were excluded from the study.
Haematocrit was done at admission and at 48 hours. A fall in haematocrit of more than 10% was considered sensitive. Modified Glasgow score comprising of nine variables were assessed at admission and at 48 hours as follows:
At admission:
Age in years >55 years
WBC count >15000 cells/mm3
Blood glucose >10 mmol/L (with no history of diabetes)
Serum urea >16 mmol/L (no response to intravenous fluids)
Arterial oxygen saturation PaO2 <8 kPa (60 mmHg)
At 48 hours:
Serum calcium <2.0 mmol/L (<8.0 mg/dL)
Serum albumin <32 gm/L
LDH >600 U/L
AST/ALT >600 U/L.
A modified Glasgow score of ≥3 was considered sensitive [14].
CT of abdomen was done at 72 hours to assess pancreatic inflammation, pancreatic necrosis, associated complications and a CTSI score was given as follows:
Pancreatic inflammation:
0: normal pancreas
2: intrinsic pancreatic abnormalities with or without inflammatory changes in peripancreatic fat
4: pancreatic or peripancreatic fluid collection or peripancreatic fat necrosis
Pancreatic necrosis:
0: none
2: 30% or less
4: more than 30%
Extrapancreatic complications:
2: one or more of pleural effusion, ascites, vascular complications, parenchymal complications and/or gastrointestinal involvement.
CTSI scores of 0-3 are considered as mild, 4-6 as moderate and 7-10 as severe pancreatitis [15]. In this study, CTSI score of ≥4 was considered sensitive. The results of each prognostic marker were graphed and compared to assess LOHS, need for ICUA, OF, mortality.
Statistical Analysis
The statistical analysis was done using SPSS software version 21. The statistics were done using Levene’s test for equality of variances, t-test for equality of means and ROC curves. A p-value less than 0.05 was considered as statistically significant.
Results
A total of 120 patients were included in the study. The mean (SD) age of the study group was 38.68 (11.939) years of which 108 were males (90%) and 12 were females (10%).
Length of Hospital Stay (LOHS)
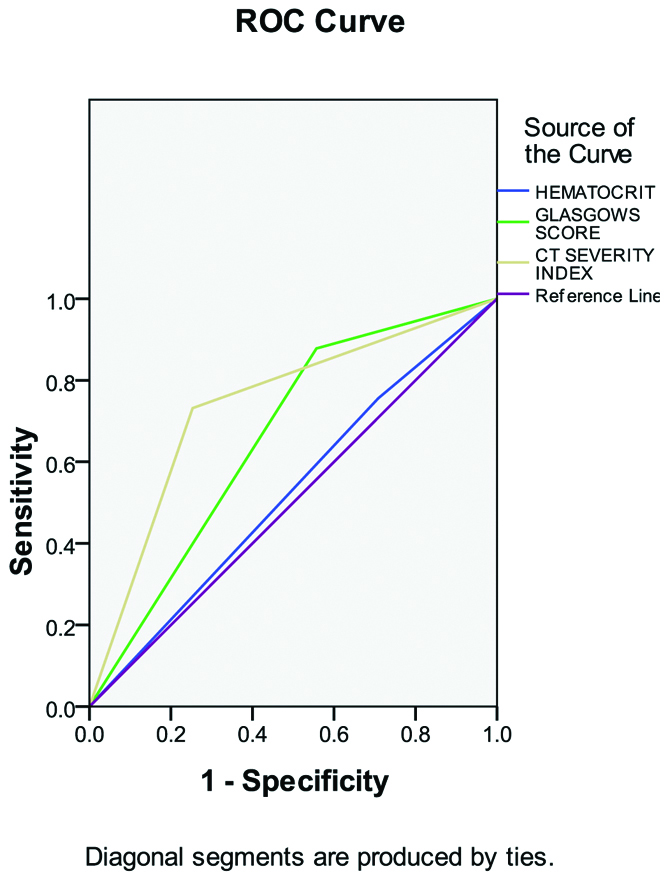
The mean LOHS was six. Haematocrit was sensitive in 23 of 79 patients who stayed in hospital for >6 days. Modified Glasgow scores were sensitive in 35 of 79 patients. CT of abdomen was sensitive in 59 out of 79 patients. The Area Under the Curve (AUC) is 0.524 for haematocrit, 0.661 for Glasgow score and 0.739 for CT abdomen as seen in [Table/Fig-1]. The sensitivity, specificity, PPV and Negative Predictive Value (NPV) of the above data is shown in [Table/Fig-2].
ROC curve- Assessment of Length of Hospital Stay (LOHS) showing more AUC for CTSI.
ROC curve: Receiver operating characteristic curve; AUC: Area under the curve; CTSI: Computed tomography severity index
Summary statistics- Length of Hospital Stay (LOHS).
| Marker | Sensitivity | Specificity | PPV | NPV |
|---|
| Haematocrit | 29.1 | 75.6 | 69.7 | 35.6 |
| Modified Glasgow score | 44.3 | 87.8 | 87.5 | 45 |
| CTSI | 74.4 | 73.2 | 84.3 | 60 |
CTSI: Computed tomography severity index; PPV: Positive predictive value; NPV: Negative predictive value
Need for Intensive Care Unit (ICU) Admission
Twenty-nine out of 120 patients were admitted in the ICU. Among 29 patients, fall in haematocrit was sensitive in 14 patients, Modified Glasgow score of ≥3 was seen in 14 patients and CTSI scores were sensitive in 22 patients. The AUC is 0.637 for haematocrit, 0.599 for Glasgow score and 0.616 for CT abdomen as seen in [Table/Fig-3].
ROC curve- Assessment of need for ICU care.
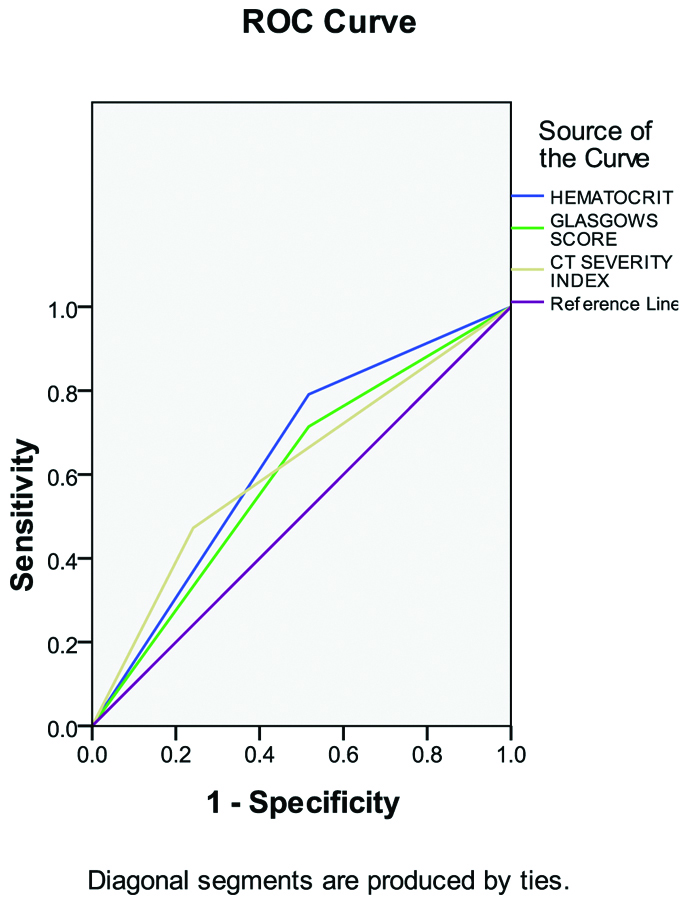
The sensitivity, specificity, PPV and NPV of the above data is shown in [Table/Fig-4].
Summary statistics- Need for ICU care.
| Marker | Sensitivity | Specificity | PPV | NPV |
|---|
| Haematocrit | 48.3 | 79.1 | 42.4 | 82.8 |
| Modified Glasgow score | 48.3 | 71.4 | 35 | 81.3 |
| CTSI | 75.9 | 47.3 | 31.4 | 86 |
CTSI: Computed tomography severity index; PPV: Positive predictive value; NPV: Negative predictive value
Organ Failure (OF)
Total 12 out of 120 patients developed OF. All 12 patients showed a sensitive Modified Glasgow score of ≥3 and CTSI ≥4 whereas only five patients were sensitive for haematocrit. The AUC is 0.579 for haematocrit, 0.870 for Glasgow score and 0.731 for CT abdomen as seen in [Table/Fig-5].
ROC curve- Assessment of Organ Failure (OF) showing more AUC for Glasgow’s score.
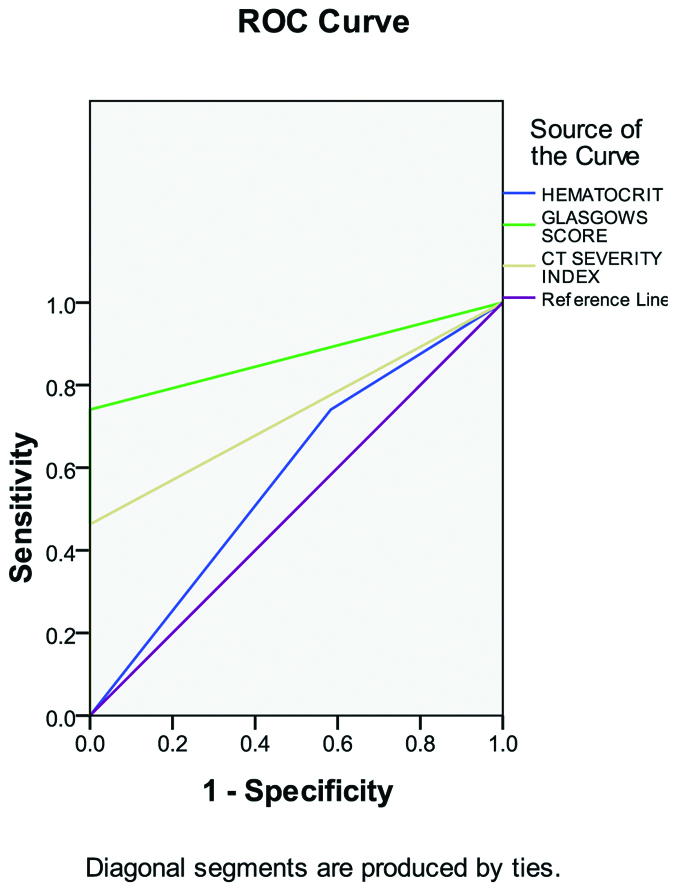
The sensitivity, specificity, PPV and NPV of the above data is shown in [Table/Fig-6].
Summary statistics- Organ Failure (OF).
| Marker | Sensitivity | Specificity | PPV | NPV |
|---|
| Haematocrit | 41.7 | 74.1 | 52.2 | 92 |
| Modified Glasgow score | 100 | 74.1 | 30 | 100 |
| CTSI | 100 | 46.3 | 17.1 | 100 |
CTSI: Computed tomography severity index; PPV: Positive predictive value; NPV: Negative predictive value
Mortality
Five patients died during the study. All the five patients were sensitive for change in haematocrit Glasgow’s scores and CT abdomen. Among the prognostic markers, haematocrit showed 100% sensitivity, specificity and PPV than the other prognostic markers making haematocrit the better prognostic marker. The AUC is 0.878 for haematocrit, 0.848 for Glasgow score and 0.717 for CT abdomen as shown in [Table/Fig-7]. The sensitivity, specificity, PPV and NPV of the above data is shown in [Table/Fig-8].
ROC curve- Assessment of mortality showing more AUC for Haematocrit.
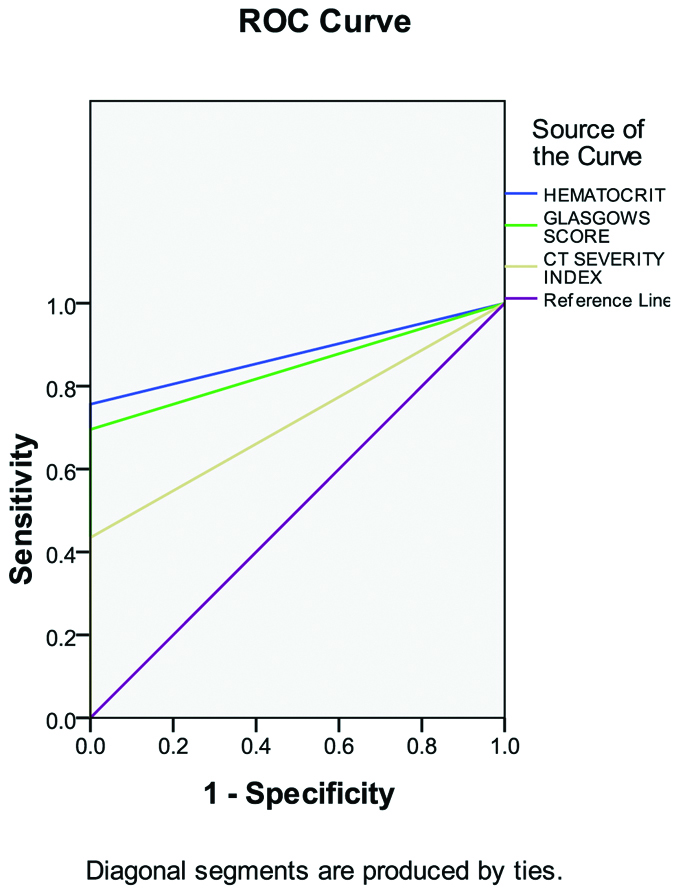
Summary statistics- Mortality.
| Marker | Sensitivity | Specificity | PPV | NPV |
|---|
| Haematocrit | 100 | 75.7 | 15.2 | 100 |
| Modified Glasgow score | 100 | 79.6 | 12.5 | 100 |
| CTSI | 100 | 43.5 | 7.1 | 100 |
CTSI: Computed tomography severity index; PPV: Positive predictive value; NPV: Negative predictive value
Discussion
The early identification of severe AP paves way for selection of patients requiring more intensive and invasive methods of treatment. Various modalities of predicting the severity of pancreatitis and identifying its outcomes were done comparing the results of this study.
In this study, CT abdomen with CTSI score of ≥4 showed more sensitivity than the other two prognostic markers in prediction of LOHS proving CT abdomen to be the most reliable marker. Banday IA et al., in a similar study revealed that patients with higher modified CTSI had poor outcomes with a longer hospital stay and higher incidence of complications [16]. The need for intervention was also higher in such patients.
On patients requiring ICU care, CT abdomen with CTSI scores of ≥4 was seen in 22 of 29 patients while fall in haematocrit and Glasgow’s score of ≥3 were seen in 14 of 29 patients. CT abdomen was the most sensitive marker; while haematocrit, although less sensitive was more specific in terms of assessing the need for ICU care. Jeevangi BA et al., in a study on management of AP using modified CTSI, found to have similar results as seen in this study with a significant p-value <0.001 in predicting the patients requiring ICU care [2].
Glasgow scoring showed 100% sensitivity and more specificity than CT abdomen and haematocrit for assessment of OF. Similarly, in a study by Mounzer R et al., comparing various existing scoring systems to predict persistent OF showed Glasgow score the best predictor among all [17]. Miko A et al., in a meta-analysis done on 5988 patients with AP showed similar results to present study. CTSI have the least prognostic value in assessing the mortality of the patient when compared to the other prognostic indices used in that study [1].
In this study, it was found that not all the markers (Haematocrit, Glasgow score and CT abdomen) are equally sensitive or specific in prediction of LOHS, need for ICU care and mortality in AP. However, all the three were sensitive in predicting mortality in such patients.
Limitation(s)
The complications observed in this study were acute manifestations of pancreatitis while long term complications of pancreatitis were not studied. Larger sample size with multi-center study would have yielded accurate results on comparison.
Conclusion(s)
CT of abdomen was a sensitive prognostic marker in terms of assessment of LOHS, need for ICU care and mortality. Haematocrit was specific in assessing the need for ICU care and in predicting the mortality with a PPV among the other prognostic markers. Modified Glasgow’s score was accurate in assessing OF in AP.