Primary Small Cell Neuroendocrine Carcinoma of Urinary Bladder: Case Series of a Rare Entity
Noushad Aryadan1, Sithara Aravind2, Akhil Suresh3, Sangeetha Keloth Nayanar4
1 Assistant Professor, Department of CLSTR, Division of Oncopathology, Malabar Cancer Centre, Thalassery, Kerala, India.
2 Associate Professor, Department of CLSTR, Division of Oncopathology, Malabar Cancer Centre, Thalassery, Kerala, India.
3 Assistant Professor, Department of Radiation Oncology, Malabar Cancer Centre, Thalassery, Kerala, India.
4 Professor, Department of CLSTR, Division of Oncopathology, Malabar Cancer Centre, Thalassery, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sithara Aravind, Associate Professor, Department of CLSTR, Division of Oncopathology, Malabar Cancer Centre, Thalassery-670103, Kerala, India.
E-mail: sitharaaravind@gmail.com
Small cell Neuroendocrine Carcinoma (SmNEC) is defined as the malignant neoplasm with Neuroendocrine (NE) differentiation. SmNEC of urinary bladder is a rare entity accounting for 0.3 to 0.7% of all malignant bladder tumours. The largest case series to date includes 64 cases from multiple hospitals across the world. In the present series author undertook a retrospective analysis of clinicopathological and survival characteristics of all cases with immunomorphological diagnosis of primary SmNEC of bladder treated at our centre from 2015-2019. Indian literature describing this entity is still sparse, and to the best of our knowledge present study is the first of its kind from Southern India. Of the total 569 cases of bladder carcinomas reported in our institution, during the five year period, six cases (0.8%) were of primary SmNEC. All the cases were at stage III/IV at the time of diagnosis. Along with characteristic histopathological features, Immunohistochemistry (IHC) for p16 and for NE differentiation- IHC-CD56 was positive in all cases leading to a definite diagnosis. Different modalities of treatment were offered owing to the lack of specific treatment guidelines. Median survival time was found to be seven months.
Histology, Immunohistochemistry, Radiology, Survival, Treatment
Introduction
SmNEC is a malignant neoplasm with NE differentiation. Lower respiratory tract is the most common site of origin of SmNEC. Extrapulmonary small cell carcinomas have been reported to arise in almost all body sites except Central Nervous System (CNS). Primary SmNEC of urinary bladder is a rare neoplasm which accounts for 0.3 to 0.7% of all primary bladder cancers [1] first described by Cramer SF et al., in 1981 [2]. Male gender and cigarette smoking are the accepted risk factors with chemical exposure, bladder calculi, and chronic cystitis being proposed aetiologies [3]. It is a highly aggressive malignancy with poor survival - most of the patients present at an advanced stage and exhibit metastatic disease at the time of diagnosis. For a tumour to be classified as SmNEC, the small cell histology must constitute the majority of the tumour. The characteristic NE differentiation are demonstrated by electron microscopy or IHC. The most common immunohistochemical stains used in the diagnosis of NE differentiation are synaptophysin, chromogranin and Neuron Specific Enolase (NSE) [4]. There are no established management protocols at present for this entity in view of its rarity. Background of the present study is that to the best of our knowledge there is no literature describing primary SmNEC of urinary bladder in South Indian population.
Case Series
After getting clearance from Institutional Ethical Committee (1616/IRB-SRC/13/MCC/12-10-2019/7), this retrospective single centre study was undertaken and analysed the data of all cases with immunomorphological diagnosis of primary SmNEC of urinary bladder treated at the institution Malabar Cancer Centre, Kerala, India, from a period of January 2015-December 2019. Haematoxylin and Eosin (H&E) stained sections of formalin fixed praffin embedded sections of tumour was analysed for histomorphological parameters and IHC findings were documented. Clinico-radiological and immunomorphological details of the cases are described in [Table/Fig-1,2,3,4,5,6 and 7]. Details of the treatment given, outcome and survival details of each case and kaplan meier curve for survival analysis is shown in [Table/Fig-8,9].
Details of the clinical, radiological, histopathological and Immunohistochemistry (IHC) of each case.
| Case No. | Age | Sex | Symptom at presentation | Habit history | Radiological features | Provisional diagnosis | Histological features | IHC†-Positive markers | IHC negative markers |
|---|
| 1 | 68 | M | Dysuria | Smoker | Well defined heterogeneously enhancing polypoidal lesion from right lateral wall | Urothelial carcinoma | Diffuse growth scanty cytoplasm stippled chromatincrush artefact necrosis | SyPCD56CK€p16 | CgA*p63 |
| 2 | 70 | F | Obstructive symptoms | Nil | Heterogeneously enhancing polypoidal lesion from posterior wall | Urothelial carcinoma | Diffuse growth scanty cytoplasm stippled chromatincrush artefact necrosis | SyP≠CD56CKp16 | CgAp63 |
| 3 | 56 | M | Painless haematuria | Smoker | Large polypoidal lesion in the anterior and right lateral wall filling the lumen | Urothelial carcinoma | Diffuse growth scanty cytoplasm stippled chromatincrush artefact necrosis | SyPCD56CKp16 | p63CD45 |
| 4 | 71 | M | Painless haematuriaHypercalcaemia | Smoker | Irregular wall thickening on anterior wall | Urothelial carcinoma | Diffuse+ nested growth scanty cytoplasm stippled chromatin crush artefactnecrosis mixed, SmNEC+ High grade UCC (Minor component) | CD56p16CgACK | p63 |
| 5 | 71 | M | Obstructive symptoms | Smoker | Heterogenously enhancing polypoidal lesion in the right lateral wall | Urothelial carcinoma | Diffuse growth scanty cytoplasm stippled chromatincrush artefact necrosis | CD56p16CK | SyPp63CgACD 45 |
| 6 | 76 | M | Painless haematuria | Smoker | Irregular polypoidal lesion in the right lateral wall extending to anterior wall | Urothelial carcinoma | Diffuse growth scanty cytoplasm stippled chromatincrush artefact necrosis | SyPCD56p16CK | p63 |
SmNEC: Small cell neuroendocrine carcinoma; UCC: Urothelial carcinoma; CD: Cluster of differentiation; ≠Syp-synaptophysin; €CK: Cytokeratin, *CgA: Chromogranin A; †IHC: Immunohistochemistry
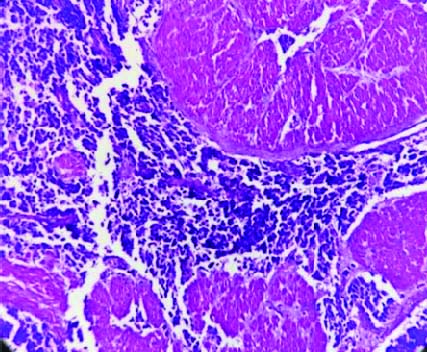
H&E, stained section shows neoplastic cells arranged diffusely and invade muscle bundle (40x).
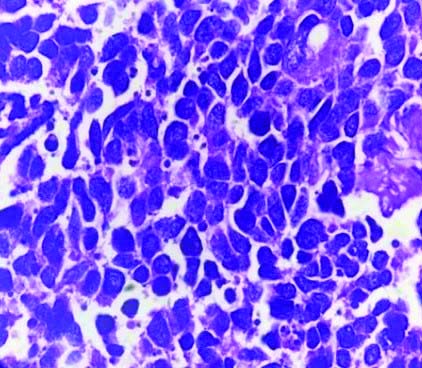
H&E, stained section shows neoplastic cells showing nuclear molding (40X).
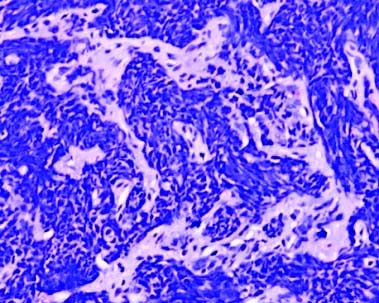
H&E, stained section shows cells with crush artefact (10X).
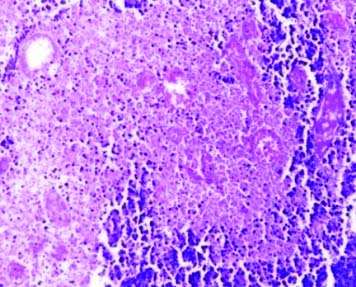
H&E, stained section shows necrotic areas (40X).
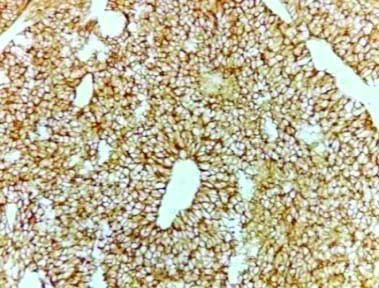
Immunohistochemical stain showing diffuse CD56 expression.
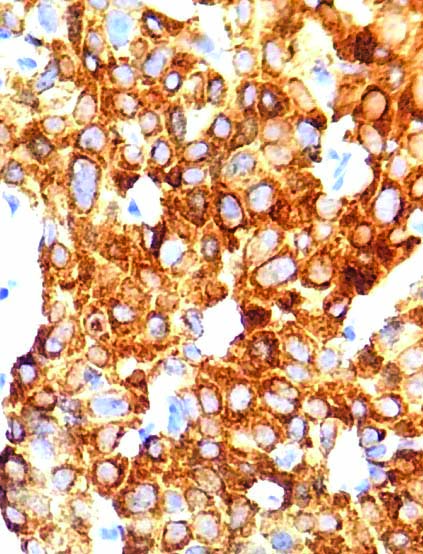
Immunohistochemical stain showing diffuse synaptophysin expression.
Details of the treatment given and survival details of each case.
| Patient | Stage | Treatment | Outcome | Survival (Days) |
|---|
| 1 | III | TURBT + Radical CT RT | Alive | 724 |
| 2 | III | TURBT+ Pall RT | Died | 211 |
| 3 | III | Radical cystoprostatectomy | Died | 78 |
| 4 | III | TURBT+ Pall RT | Died | 16 |
| 5 | III | Radical cystoprostatectomy | Died | 56 |
| 6 | III | TURBT + Radical CTRT | Alive | 106 |
TURBT: Transurethral resection of bladder tumour; CT: Chemotherapy; RT: Radiotherapy; Pall RT: Palliative radiotherapy
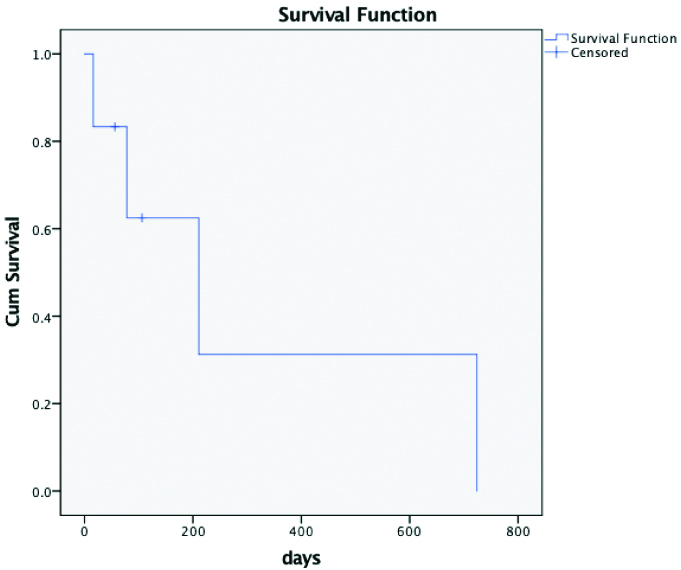
Kaplan Meier curve for survival analysis.
Discussion
Primary SmNEC of urinary bladder is an extremely rare, highly aggressive, treatment refractory tumour with high metastatic potential [5] accounting for less than 1% of all bladder tumours. Patients usually present at a later stage than urothelial carcinomas [6]. Several hypothesis have been put forward regarding cell of origin of primary SmNEC of bladder, and the most accepted one is origin from a multipotent stem cell that has the ability to differentiate into various cell types depending on the influence of specific transformation or progression-related gene. This could explain the coexistence of mixed tumours- SmNEC with other bladder carcinoma subtypes [7]. Literature reviews show that male patients in their sixth to seventh decades of life are the most common group affected [8]. Mean age was found to be 69 years in present study. Male gender and cigarette smoking are accepted risk factors with chemical exposure, bladder calculi, and chronic cystitis being proposed aetiologies. In present study, factors like the age of presentation, gender distribution (male: female ratio 5:1) and association with smoking, were in concordance with the reported literature. None of the patients in present study had any significant past medical history.
Presenting symptoms of SmNEC are similar to urothelial carcinoma, Painless haematuria being the most common symptom [9]. Half of the patients (n=3) presented with the same. One of the patients had paraneoplastic syndrome in the form of hypercalcaemia at the time of presentation [10]. According to study by Liu XJ et al., polypoidal mass was the most common gross presentation. Polypoidal growth in bladder was the gross presentation in 83% of the cases in present study [10]. Most of the western literature shows a higher incidence of mixed tumours [11]. Interestingly, in our experience mixed aetiology was low in present study population, amounting to only 16% (n=1). Histological features noted were identical to small cell carcinomas of pulmonary/non-pulmonary sites. Diffuse growth was the commonest cell pattern observed. Individual cells have increased nuclear cytoplasmic ratio, irregular nuclei with finely stippled chromatin and inconspicuous nucleoli. Nuclear moulding, brisk mitosis, tumour necrosis and crush artefact were common findings and serve as diagnostic aid. Histological details of the cases are shown in [Table/Fig-2,3,4 and 5].
Regarding IHC, the sensitivity of conventional NE markers like Synaptophysin, Chromogranin A, NSE and CD56 are usually low in bladder SmNEC. Hence, the World Health Organisation (WHO) permits the diagnosis of SmNEC of bladder based on the morphological features alone. Though the sensitivity of usual NE markers are low, study by Ismaili N showed CD56 as the most sensitive marker [12]. A 92.8% of bladder SmNEC also shows positivity for p16 [13]. In present study, 100% cases showed diffuse positivity for CD56 [Table/Fig-6] and p16. All cases were negative for p63. Other markers like synaptophysin [Table/Fig-7] were found positive in four of the five cases tested (80%) and chromogranin A in one out of four cases. Since lymphoproliferative disorder was the close differential diagnosis in two cases, IHC CD45 was performed and was found to be negative. SmNEC is associated with poor survival and a high frequency of distant metastasis when compared to age and gender matched urothelial carcinomas [14]. Most of the studies show a median survival of 20 months [15]. Pure SmNEC is seen to have worse prognosis when compared to mixed histology [15]. In present study, the median survival was found to be very low-seven months [Table/Fig-8,9]. One reason for this observation might be the small sample size.
Owing to rarity of the lesion, there are no accepted standard treatment guidelines and so it is difficult to define an optimum management. The treatment followed at our centre [Table/Fig-8] and elsewhere includes multimodal approach involving surgery, chemotherapy and radiotherapy [16]. Platinum based chemotherapy is the mainstay of treatment and studies show that it improves the overall survival [16]. In present study, though all patients presented at the same stage, a better survival was seen in patients who underwent surgery followed by adjuvant radical radio and chemotherapy.
Conclusion(s)
To conclude, primary SmNEC of urinary bladder is a rare aggressive disease with poor survival. Elderly male smokers are most commonly affected. Histomorphological differentials include high grade urothelial carcinoma and lymphoproliferative disorder. Immunohistochemical confirmation by CD56 is preferred over other NE markers and p16 IHC can be used as diagnostic aid. Owing to the rarity of tumour, definite treatment protocol has not yet been established. Multicentric studies are warranted to explore the molecular characteristics of this entity so as to develop diagnostic markers and identify specific therapeutic targets.
SmNEC: Small cell neuroendocrine carcinoma; UCC: Urothelial carcinoma; CD: Cluster of differentiation;
≠Syp-synaptophysin;
€CK: Cytokeratin, *CgA: Chromogranin A;
†IHC: Immunohistochemistry
TURBT: Transurethral resection of bladder tumour; CT: Chemotherapy; RT: Radiotherapy; Pall RT: Palliative radiotherapy
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 05, 2020
Manual Googling: Oct 21, 2020
iThenticate Software: Dec 12, 2020 (12%)
[1]. Koay EJ, Teh BS, Paulino AC, Butler EB, A surveillance, epidemiology, and end results analysis of small cell carcinoma of the bladder: Epidemiology, prognostic variables, and treatment trendsCancer 2011 117(23):5325-33.10.1002/cncr.2619721567387 [Google Scholar] [CrossRef] [PubMed]
[2]. Cramer SF, Aikawa M, Cebelin M, Neurosecretory granules in small cell invasive carcinoma of the urinary bladderCancer 1981 47(4):724-30.10.1002/1097-0142(19810215)47:4<724::AID-CNCR2820470417<3.0.CO;2-2 [Google Scholar] [CrossRef]
[3]. Church DN, Bahl A, Clinical review- Small cell carcinoma of the bladderCancer Treat Rev 2006 32(8):588-93.10.1016/j.ctrv.2006.07.01317008012 [Google Scholar] [CrossRef] [PubMed]
[4]. Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE, The 2016 WHO classification of tumours of the urinary system and male genital organs-Part B: Prostate and bladder tumoursEur Urol 2016 70(1):106-19.10.1016/j.eururo.2016.02.02826996659 [Google Scholar] [CrossRef] [PubMed]
[5]. Ismaili N, Heudel PE, Elkarak F, Kaikani W, Bajard A, Ismaili M, Outcome of recurrent and metastatic small cell carcinoma of the bladderBMC Urol 2009 9:04-09.10.1186/1471-2490-9-419500382 [Google Scholar] [CrossRef] [PubMed]
[6]. Ghervan L, Zaharie A, Ene B, Elec FI, Small-cell carcinoma of the urinary bladder: Where do we stand?Clujul Med 2017 90(1):13-17.10.15386/cjmed-67328246491 [Google Scholar] [CrossRef] [PubMed]
[7]. Christopher ME, Seftel AD, Sorenson K, Resnick MI, Small cell carcinoma of the genitourinary tract: An immunohistochemical, electron microscopic and clinicopathological studyJ Urol 1991 146(2):382-88.10.1016/S0022-5347(17)37800-X [Google Scholar] [CrossRef]
[8]. Montie JE, Small cell carcinoma of the urinary bladder. A clinicopathologic analysis of 64 patientsJ Urol 2005 173:1920-21.10.1097/01.ju.0000161245.95285.b215879778 [Google Scholar] [CrossRef] [PubMed]
[9]. Choong NW, Quevedo JF, Kaur JS, Small cell carcinoma of the urinary bladder. The Mayo Clinic experienceCancer 2005 103(6):1172-78.10.1002/cncr.2090315700264 [Google Scholar] [CrossRef] [PubMed]
[10]. Liu XJ, Liu C, Liu D, Yao DW, Primary small cell carcinoma of the urinary bladder: A 10-year retrospective review of treatment and survival at a single institutionBiomedical Research 2018 29(9):1815-21.10.4066/biomedicalresearch.29-17-2157 [Google Scholar] [CrossRef]
[11]. Abrahams NA, Moran C, Reyes AO, Siefker-Radtke A, Ayala AG, Small cell carcinoma of the bladder: A contemporary clinicopathological study of 51 casesHistopathology 2005 46(1):57-63.10.1111/j.1365-2559.2004.01980.x15656887 [Google Scholar] [CrossRef] [PubMed]
[12]. Ismaili N, A rare bladder cancer- Small cell carcinoma: Review and updateOrphanet J Rare Dis 2011 6:7510.1186/1750-1172-6-7522078012 [Google Scholar] [CrossRef] [PubMed]
[13]. Buza N, Cohen PJ, Pei Hui, Parkash V, Inverse p16 and p63 expression in small cell carcinoma and high-grade urothelial cell carcinoma of the urinary bladderInt J Surg Pathol 2010 18(2):94-102.10.1177/106689690935991420164052 [Google Scholar] [CrossRef] [PubMed]
[14]. Mukesh M, Cook N, Hollingdale AE, Ainsworth NL, Russell SG, Small cell carcinoma of the urinary bladder: A 15-year retrospective review of treatment and survival in the Anglian Cancer NetworkBJU Int 2009 103(6):747-52.10.1111/j.1464-410X.2008.08241.x19076139 [Google Scholar] [CrossRef] [PubMed]
[15]. Zhao X, Flynn EA, Small cell carcinoma of the urinary bladder: A rare, aggressive neuroendocrine malignancyArch Pathol Lab Med 2012 136(11):1451-59.10.5858/arpa.2011-0267-RS23106592 [Google Scholar] [CrossRef] [PubMed]
[16]. Moretto P, Wood L, Emmenegger U, Management of small cell carcinoma of the bladder: Consensus guidelines from the Canadian Association of Genitourinary Medical Oncologists (CAGMO)Can Urol Assoc J 2013 7:44-56.10.5489/cuaj.22023671508 [Google Scholar] [CrossRef] [PubMed]