Worldwide, burden of prostatic carcinoma is expected to grow to 1.7 million new cases and 0.5 million new deaths by 2030 simply due to the growth and ageing of the global population. Incidence of prostate cancer is increasing due to changing lifestyles, increased awareness and access to medical facility. It is coming to the knowledge that we (India) are not very far behind from western countries [1]. True incidence of prostate cancer is not known for India as it is neither a notifiable disease nor much community-based studies are available [2].
Current medical treatment include surgery, radiotherapy, chemotherapy, hormonal therapy, cryosurgery, and other modalities. Usually, in a suspected case of prostate cancer, the use of biomarkers, Prostate-Specific Antigen (PSA), PSA Velocity (PSA-V), percentage free PSA is done which can result in increased detection at an earlier stage and decreasing the number of metastatic patients.
The most common histologic type in prostate carcinoma is adenocarcinoma, followed by basal cell carcinoma, intraductal carcinoma, ductal adenocarcinoma and many more. Gleason grading International Society of Urological Pathology (ISUP 2016) is used to grade prostatic carcinoma histologically and collectively a group grade is given based on primary and secondary Gleason score [3].
Various markers used in prostate carcinoma are PAP, PSA, PSMA, androgen and progesterone receptors, HER2-neu, low molecular weight keratins and many more [4].
HER2-neu is a member of the proto-oncogene tyrosine kinase receptor family that is localised to chromosome 17 and is homologous to the neu rat gene [5]. HER2-neu expression has been widely studied in a significant proportion of breast cancer, ovarian cancer, and gastric cancer and better prognosis have been documented with the help of Trastuzumab (the humanised monoclonal anti-HER2 antibody) in the treatment of breast carcinoma.
There are studies about HER2-neu overexpression in prostatic carcinoma and many recent studies have suggested its importance in progression to a more aggressive disease [6]. So in this study, we aimed to assess the expression of HER2-neu in different histopathological grades of prostatic carcinoma in patients from a Tertiary Care Centre.
Materials and Methods
Study Design
A prospective study was carried out in the Department of Pathology of SRMSIMS, Bareilly, Uttar Pradesh, over a period of 18 months (November 2017 to April 2019) and included 41 histopathologically proven cases of prostatic carcinoma. Institutional Ethical Committee Clearance was obtained prior to the study. (IEC No. SRMSIMS/2017-18/108). All the Trans-Urethral Resection of Prostate (TURP)/ core biopsy specimen submitted to the department of pathology during the above mentioned period, were collected from the patients diagnosed as prostatic carcinoma, admitted under the department of surgery (urology) were included in the study. A Written consent was obtained from all the patients. All nonmalignant cases, inadequate biopsies and autolysed specimens were excluded from the study.
Sample size calculation: Sample size was calculated with the help of the formula
n=Z2(1-α/2) p(1-p)/d2
where Z2(1-α/2) = (1.96)2, d=0.01 and p=prevalence within institute is 10.7% according to which minimum number of cases calculated was 37 [7,8].
Study Procedure
A detailed clinical history was obtained from the patient records along with details of radiological investigations. All formalin fixed specimen were processed and were subjected to H&E stain. Stained sections were examined under light microscopy for histopathological diagnosis and tumour was classified according to the Gleason grading system according to ISUP 2016 [3].
Selected sections were subjected to immunohistochemical staining for HER2-neu. The Anti-HER2-neu antigen, IHC kit of BioGenex RTU was used. Positive (known HER2+breast carcinoma) and negative controls (primary antibody omitted) were used.
A golden brown membrane staining was considered as a positive reaction [Table/Fig-1].
Grading of the IHC staining for HER2-neu overexpression[4].
| Staining pattern | Score | HER2-neu protein overexpression assessment |
|---|
| No staining observed or membrane staining observed in <10% of the tumour cells | 0 | Negative |
| A faint/barely perceptible membrane staining is detected in >10% of the tumour cells. The cells are only stained in part of their membrane | +1 | Negative |
| Weak to moderate complete membrane staining observed in >10% of the tumour cells | +2 | Equivocal |
| Strong complete membrane staining observed in >30% of the tumour cells (formerly 10%) | +3 | Strongly positive |
A score of 3+ HER2-neu was considered positive for immunostaining, 2+ was considered equivocal while the score of 1+ and 0 were considered negative. If the immune test gives a result of 2+, Fluorescence In Situ Hybridization (FISH) was recommended which was not done due to non availability.
Data Compilation
Collected data include all 41 cases of prostatic carcinoma with their age, presenting complaints, ultrasonographic findings (wherever available), Serum PSA levels (wherever available), histological diagnosis, and HER2-neu expression, were compiled in pre-structured proforma and tabulated on Microsoft Excel spreadsheets for further analysis.
Statistical Analysis
Microsoft Excel spreadsheets and statistical tests (Student’s t test) were applied, statistical software Statistical Package for the Social Sciences (SPSS) version 21.
Results
The study comprises 41 cases of histologically proven prostatic carcinoma, which was correlated with their age, histological type, histologic grade, Serum PSA levels, ultrasonographic findings and HER2-neu status.
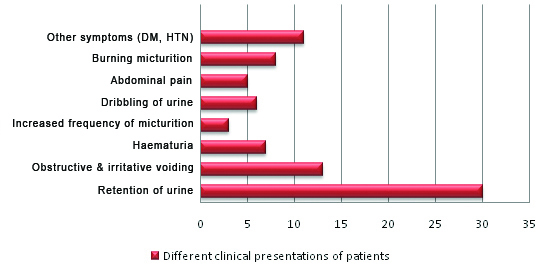
Following observations were noted- Most common presenting symptom was retention of urine (30,73.1%), followed by obstructive and irritative voiding (13,31.7%), burning micturition (8,19.5%), haematuria (7,17.0%), dribbling of urine (6,14.6%) and abdominal pain (5,12.19%). Few other clinical complaints like generalised body ache, pain, and swelling in lower limbs, fever, anaemia were also noticed in some patients collectively contributing to 30% retention of urine [Table/Fig-2].
Different clinical presentations of patients.
Age wise distribution of prostate carcinoma is shown in [Table/Fig-3]. Out of 39 (in two cases ultrasound was not done) cases that were subjected to ultrasonography, almost similar number of cases i.e., 16 and 15 cases had grade III prostatomegaly and grade II prostatomegaly, respectively and there were four cases that had grade I and IV prostatomegaly each [Table/Fig-4].
Age wise distribution of prostate carcinoma.
| S. No. | Age group (years) | No. of cases | Percentage |
|---|
| 1 | 41-50 | 1 | 2.4 |
| 2 | 51-60 | 5 | 12.2 |
| 3 | 61-70 | 14 | 34.1 |
| 4 | 71-80 | 17 | 41.5 |
| 5 | 81-90 | 4 | 9.8 |
| Range of distribution | 45-83 years |
| Mean age of presentation | 70.58 years |
| Standard deviation | 8.18 years |
Distribution of cases based on Ultrasound findings.
| S. No. | USG finding | No. of cases (39) | Percentage (%) |
|---|
| 1 | Grade I Prostatomegaly | 4 | 10.2 |
| 2 | Grade II Prostatomegaly | 15 | 38.5 |
| 3 | Grade III Prostatomegaly | 16 | 41.1 |
| 4 | Grade IV Prostatomegaly | 4 | 10.2 |
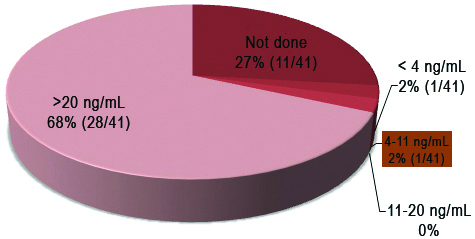
Only thirty of the forty-one cases had S. PSA levels measured before the biopsy/surgery. It was observed that the maximum number of cases that were 28 had S. PSA levels of >20 ng/mL. S. PSA levels of one case each fall in the category of <4 ng/mL and 4-11 ng/mL, respectively. None of them had the S. PSA levels of 11-20 ng/mL. In eleven cases S. PSA levels were not available [Table/Fig-5].
Distribution of cases based on Serum PSA level.
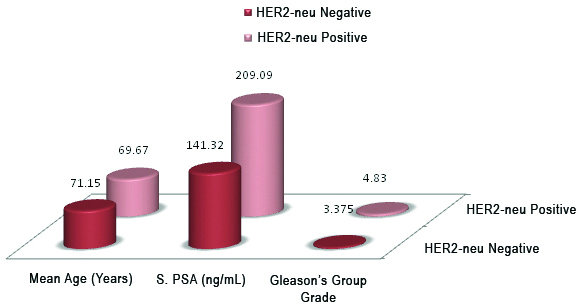
Comparison of mean age, mean S. PSA levels and mean Gleason Group Grade based on over expression of HER2-neu is shown in [Table/Fig-6].
Comparison of mean age, mean S. PSA levels and mean Gleason Group Grade based on over Expression of HER2-neu.
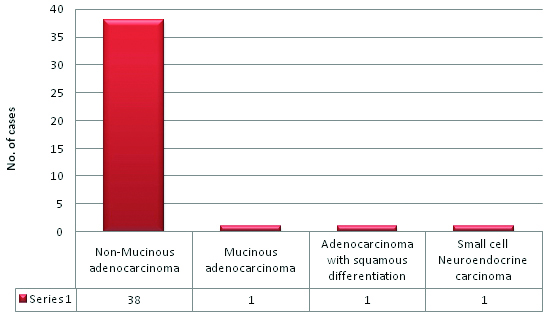
Out of forty-one cases, the maximum number of cases i.e., 92.7% (38/41) was reported as prostatic adenocarcinoma of nonmucinous type. A 2.43% (1/41) cases were reported as mucinous adenocarcinoma and small cell neuroendocrine carcinoma each respectively. One (2.43%) case even reveals squamous differentiation [Table/Fig-7,8,9,10 and 11].
Distribution of cases according to histological type.
a) Prostatic adenocarcinoma Gleason 3+3=6 (H&E,100x). b) Prostatic adenocarcinoma Gleason 4+4=8 (H&E,400x).
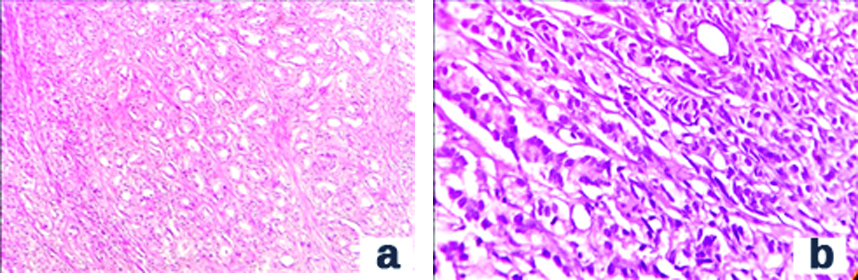
(a) Prostatic adenocarcinoma Gleason 4+4=8: Cribriform Pattern (H&E,400x). (b) Prostatic adenocarcinoma Gleason 5 +5=10: Solid Pattern (H&E,100x).
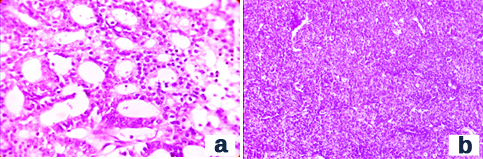
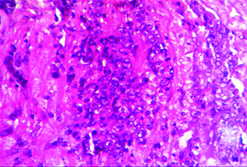
a) Prostatic adenocarcinoma Gleason 5+5=10: Comedonecrosis (H&E,100x). b) Mucinous Prostatic adenocarcinoma (H&E,400x).

Small cell neuroendocrine carcinoma (H&E,400x).
[Table/Fig-12] shows distribution of cases as per Gleason grading system. One case was reported as neuroendocrine carcinoma in which Gleason grading was not done (but was included in the study because as per topic we have to include all prostatic carcinoma cases). As shown in [Table/Fig-13], 42.5% were grouped under grade group 5, 27.5% under grade group 3, Four (10%) cases were grouped under grade groups 1,2 and 4 each.
Distribution of cases according to Gleason grading.
| S. No. | Gleasons grading | No. of cases (40) | Percentage (%) |
|---|
| 1 | 6 (3+3) | 4 | 10 |
| 2 | 7 (3+4) | 4 | 10 |
| 3 | 7 (4+3) | 11 | 27.5 |
| 4 | 8 (4+4) | 4 | 10 |
| 5 | 8 (3+5) | 0 | 0 |
| 6 | 8 (5+3) | 0 | 0 |
| 7 | 9 (4+5) | 10 | 25 |
| 8 | 9 (5+4) | 6 | 15 |
| 9 | 10 (5+5) | 1 | 2.5 |
| 10 | TOTAL | 40 | 100 |
| One case was reported as neuroendocrine carcinoma in which gleason grading was not done |
Distribution of cases according to Grade grouping.
| S. No. | Grade Groups | | No. of cases (40) | Percentage (%) |
|---|
| 1 | Grade Group 1 | 6 (3+3) | 4 | 10 |
| 2 | Grade Group 2 | 7 (3+4) | 4 | 10 |
| 3 | Grade Group 3 | 7 (4+3) | 11 | 27.5 |
| 4 | Grade Group 4 | 8 (3+5) | 4 | 10 |
| 8 (5+3) |
| 8 (4+4) |
| 5 | Grade Group 5 | 9 (5+4) | 17 | 42.5 |
| 9 (4+5) |
| 10 (5+5) |
| 6 | Total | 40 | 100 |
| One case was reported as neuroendocrine carcinoma in which gleason grading was not done |
A 14.6% cases show a membrane positivity of +3 [Table/Fig-14a] and thus they were considered as positive and in 80.5% cases were negative [Table/Fig-14b] for HER2-neu expression. A 4.9% cases demonstrated +2 [Table/Fig-14c] membrane positivity which is considered as equivocal and needs to be confirmed with the help of FISH method. Due to the unavailability of FISH method these two cases were considered as unequivocal and were kept separately [Table/Fig-15].
HER2-neu expression(400x); 3+: Strong complete membrane staining seen in >30% of the tumour cells. (b) HER2-neu expression(400x):1+: Faint membrane staining in >10% of the tumour cell. (c) HER2-neu expression(400x); 2+: Weak to moderate complete membrane staining in >10% of the tumour cells.
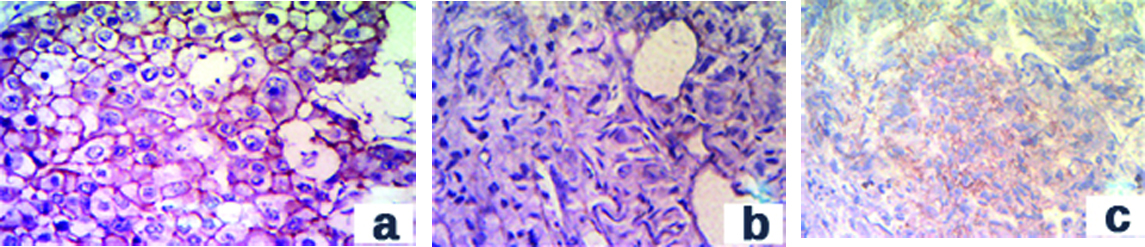
HER2-neu expression in cases.
| S. No. | HER2-neu expression | No. of cases (41) | Percentage (%) |
|---|
| 1 | Negative | 0, +1 | 33 | 80.5 |
| 2 | Equivocal | +2 | 2 | 4.9 |
| 3 | Positive | +3 | 6 | 14.6 |
| Total | 41 |
In cases with positive HER2-neu expression, mean group grade was calculated to be 4.83±0.40 and in patients with negative HER2-neu expression, mean prostatic volume was 3.38±1.40. There was a significant statistical difference (p=0.00003668) found between the Gleason Group Grade in HER2-neu positive and negative patients as HER2-neu positivity is seen in higher group grades [Table/Fig-16].
Comparison of mean of Gleason Group Grade with HER2-neu expression (mean of gleason group grades in HER2-neu positive and negative cases were calculated).
| S. No. | HER2-neu expression | Mean | p-value |
|---|
| Gleason Group Grade | Positive | 4.83±0.40 | 0.00003668 |
| Negative | 3.38±1.40 |
Discussion
According to recent studies, prostate cancer is responsible for nearly 6% of all male cancer death. Almost 95% of the patients are in an advanced stage at the time of diagnosis. Overexpression of HER2-neu oncogene has been widely studied and frequently detected in breast, ovarian, lung, bladder and gastric cancers. In prostate cancer, the role of HER2-neu overexpression remains uncertain since conflicting results emerge from various studies.
In the present study, a total of 41 histopathologically proven cases of prostatic carcinoma were evaluated. HER2-neu overexpression by the IHC method was observed in 6 (14.6%) cases. HER2-neu overexpression is higher than the study done by the United States National Cancer Institute conducted in 2002. They found overexpression of HER2-neu in 5 cases out of 62 i.e., 8.0% where 1 case was 3+ and 4 were 2+, which were later confirmed by FISH.
Gu K et al., reported HER2-neu positivity in 62% of cases [9]. HER2-neu overexpression was reported as 29% in Ross JS et al., [10]. These numbers are quite high when compared to the present study. Zahir ST et al., reported HER2-neu overexpression in 4 (10%) cases [11]; Musalam A et al., in 17 (37%) [12]. Overall, in agreement with these studies, Authors found overexpression of HER2-neu in prostate carcinoma in the present study, but the percentage of cases showing HER2-neu overexpression was less when compared to these studies which could be due to nonavailability of FISH and/or low sample size.
S. PSA and HER2-neu immunostaining, In the present study, only thirty of the forty-one cases had S. PSA levels measured before the biopsy/surgery and were evaluated with respect to HER2-neu immunostaining in those thirty cases. Out of 30, six cases were HER2-neu positive and rest 24 were negative. Correlation was found between S. PSA levels and HER2-neu expression (p-value=0.047; r = +0.179). In HER2-neu positive cases, mean S. PSA is quite higher (209.09±48.42) when compared to mean S. PSA in HER2-neu negative cases (141.32±118.73) [Table/Fig-17]. Similar relationship was found in the study conducted by Zahir ST et al., [11], (p= 0.019; r=0.449) [12]. The present study was not in concordance with the study done by Musalam A et al., and Minner S et al., [12,13]. Musalam A et al., [12] showed that there was no significant correlation between total S. PSA and HER2-neu overexpression in prostate carcinoma [Pearson (r)=-0.009, p-value=0.9461] [12]. Similarly, Minner S et al., did not find any correlation between HER2-neu expression and preoperative S. PSA [13].
Comparison of S. PSA Levels (ng/mL) with HER2-neu expression.
| HER2-neu expression | Mean | p-value | Pearson coefficient (29) |
|---|
| S. PSA levels (ng/mL) | Positive | 209.09±48.42 | 0.047 | +0.179 |
| Negative | 141.32±118.73 |
Gleason Group Grade and HER2-neu expression [Table/Fig-18]. In the present study, Gleason grading was done in 40 cases, remaining one case was reported as small cell neuroendocrine carcinoma. There was a significant correlation between Gleason group grading and HER2-neu overexpression (p-value=0.00003668, highly significant).
Correlation between Gleason grading and HER2-neu expression.
| Correlation between Gleason grading and HER2-neu expression (p-value) |
|---|
| Present study | p=0.00003668 |
| Minner S et al., [13] | p<0.0001 |
Similar results were obtained by Minner S et al., as they found a significant correlation between Gleason grading and HER2-neu immunostaining (p<0.0001, each i.e., separately calculated in all groups) [13]. Not many comparative studies are available for group grading system as this system of scoring is recently introduced in 2016 [11].
In the present study, patient age, S. PSA and Gleason group grading shows a positive and significant relationship with HER2-neu expression whereas prostatic volume in cc does not show a significant relationship with HER2-neu expression. The exact role of HER2-neu expression in pathogenesis and treatment of prostate carcinoma is still unknown The question, whether patients of prostatic carcinoma could benefit from monoclonal antibodies therapy targeting HER2-neu receptor is still unresolved till date. Therapeutic effect of Herceptin has been observed in animal models which support the potential utility of such treatment [13].
In the present study, a higher significant relation between HER2-neu expression, and Gleason group grading of prostatic carcinoma, argue in favor of using HER2-neu as a drug target in high grades of prostatic carcinoma.
Limitation(s)
However, there were few limitations in this study. The sample size was low, thus choice for statistical tests was limited and two cases in this study showed equivocal expression on HER2-neu staining which needs to be confirmed by FISH technique, which was unavailable in our institute. Because of this, these two cases were neither classified as positive nor negative.
Conclusion(s)
Compared to low Gleason Group Grade carcinoma, higher percentage of HER2-neu expression is seen in high Gleason Group Grade carcinoma. Statistically significant difference is found between the S. PSA levels (ng/mL) and HER2-neu expression and also between the age group of the patients and HER2-neu expression. No significant statistical difference was found between the prostatic volume on ultrasonography and HER2-neu expression.
Moreover, the effect of trastuzumab was limited in a few clinical prostate cancer trials. It could be argued, nevertheless, that different dosages of trastuzumab or combination therapy would be required to be effective in prostate cancers showing overexpression. Independent of this, it might be interesting to include prostate cancer patients in clinical studies using new generations of more efficient anti-HER2 therapy such as the anti-HER2 recombinant humanised monoclonal antibody 2C4 or antisense approaches. So in future studies with larger sample size and availability of FISH, the role of this receptor in worsening prognosis of prostate cancer can be spoken with great certainty.