Introduction
Cavernous sinus haemangioma are rare extra-axial parasellar lesions [1]. They may be intracavernous (originating from components of the cavernous sinus) or extra-cavernous (originating from the adjacent tissues) [2]. Dynamic contrast enhanced MRI plays an important role in their diagnosis and obviate the need of additional investigation due to its superior soft tissue resolution and characteristic imaging findings. MRI can also be provided invaluable information about adjacent structures involved, which can help in precise surgical planning.
Case Series
Case I
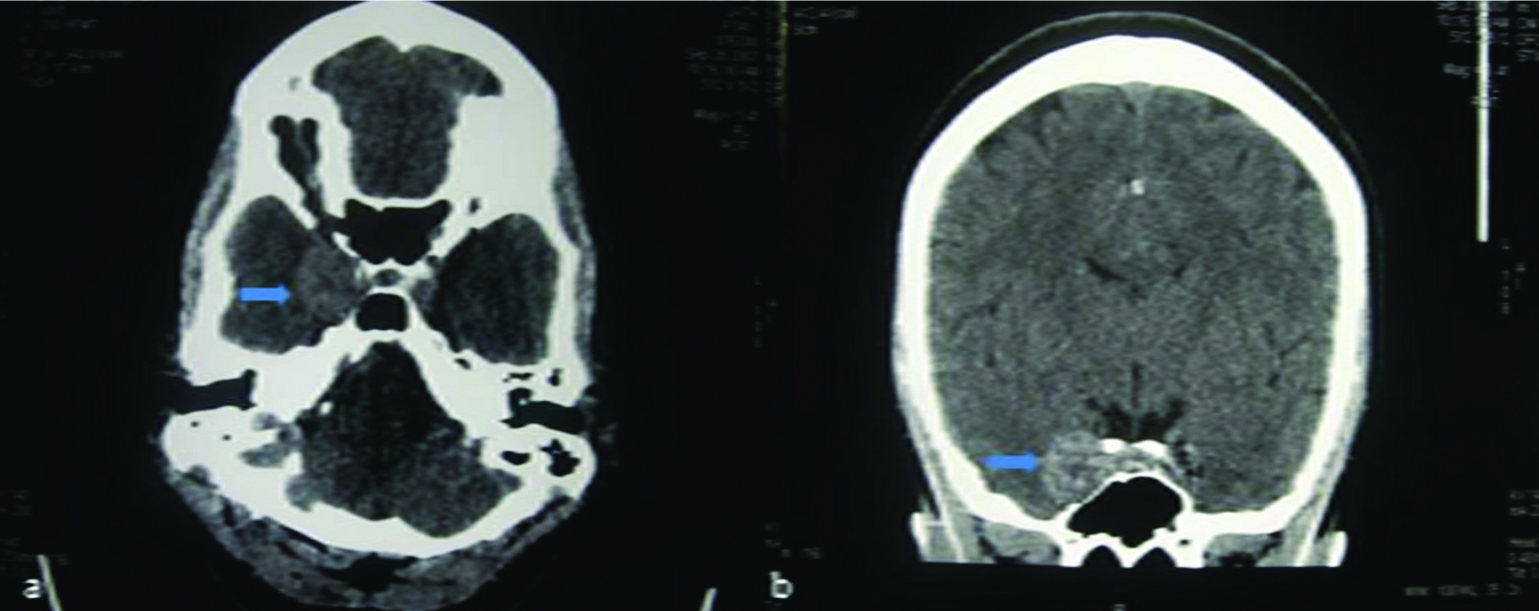
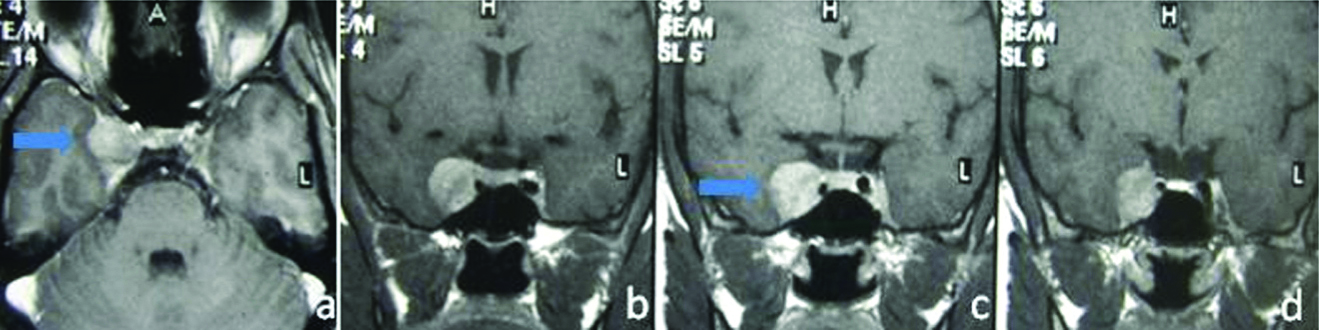
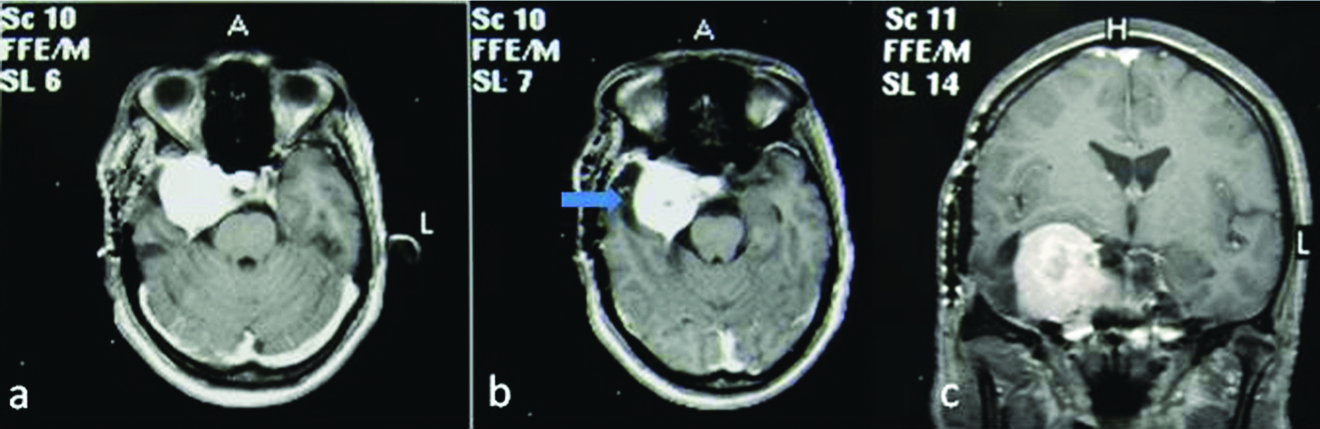
A 34-year-old female presented at the Outpatient Department with the complaint of long-standing intermittent headache. The pain was generalised in nature with mild to moderate severity. There were no trigger factors and was relieved after pain killers. For last few months, pain has increased in severity and duration and response to the pain killers has also reduced. A Contrast-Enhanced Computed Tomography (CECT) scan of the head done at an outside facility had revealed a right parasellar mass, reported as Meningioma [Table/Fig-1]. Magnetic Resonance Imaging (MRI) was done in this institute on a Philips NT Intera 1.5 Tesla system employing axial, coronal and sagittal T1W Spin Echo, T2W Turbo Spin Echo FLAIR (Fluid Attenuated Inversion Recovery) sequences.
Contrast enhanced CT axial (a) and coronal (b) images shows a well-circumscribed heterogeneous enhancing mass lesion (blue arrow) in right cavernous sinus.
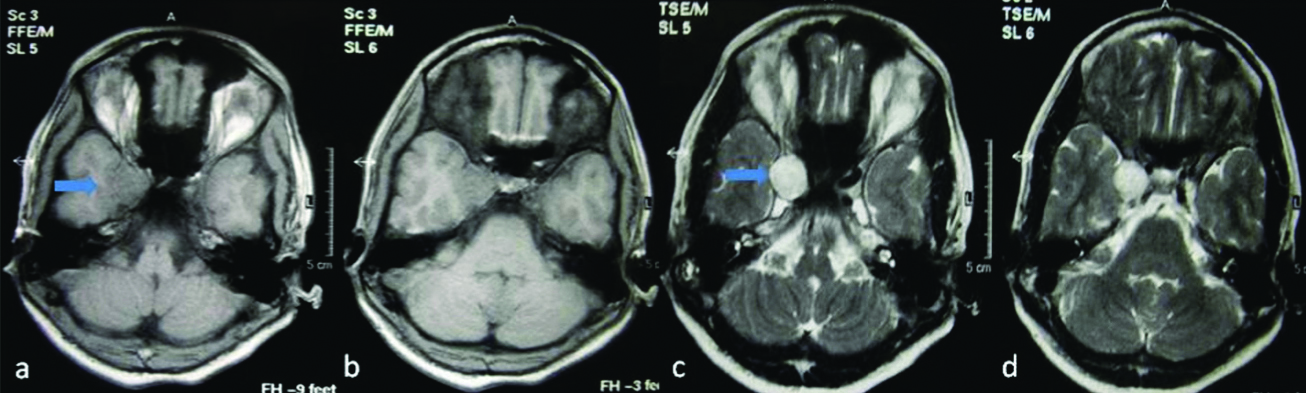
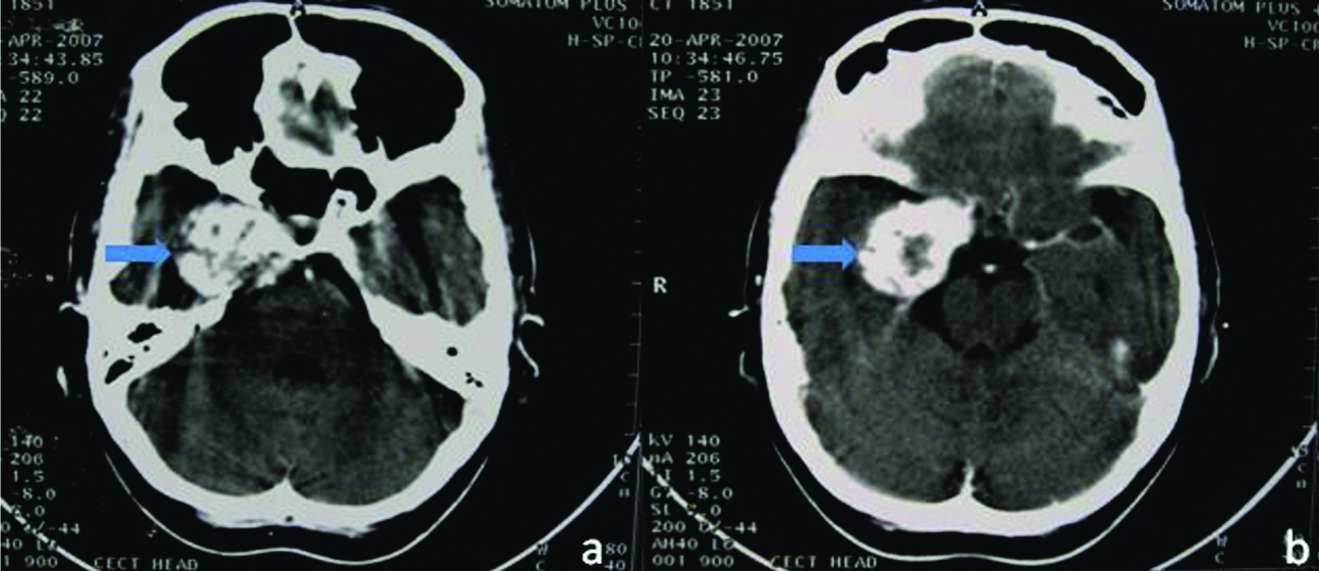
A homogeneous well-defined mass lesion was seen within and expanding the right cavernous sinus. The lesion was iso-hypointense on T1W and showed marked homogeneous hyperintensity on T2W images [Table/Fig-2a]. A dynamic post-contrast T1W study was acquired with a gadolinium contrast dose of 0.1 mmol/kg; after injecting intravenous contrast, images were acquired at 5, 12 and 25 minutes. Immediate post-intravenous contrast images showed peripheral nodular enhancement [Table/Fig-2b], with progressive centripetal filling of the lesion [Table/Fig-2c]. Delayed (25 minutes) images showed complete opacification of the lesion [Table/Fig-2d]. The diagnosis of the haemangioma was made based on the characteristic MRI findings. Given the long duration of the patients’ symptoms, no significant deterioration in the clinical picture, and characteristic findings on MRI, the planned surgery was cancelled, and the patient was treated conservatively. She was given symptomatic treatment (pain killers) for headache.
T1W axial (a,b) images reveals a well-defined, rounded mass lesion (blue arrow) in right cavernous sinus with isointense signal. On T2W (c,d) images the mass lesion shows hyperintense signal.
Dynamic Postcontrast (5 min.) axial (a,b) and coronal (c) images shows peripheral nodular enhancement of the lesion (blue arrow).
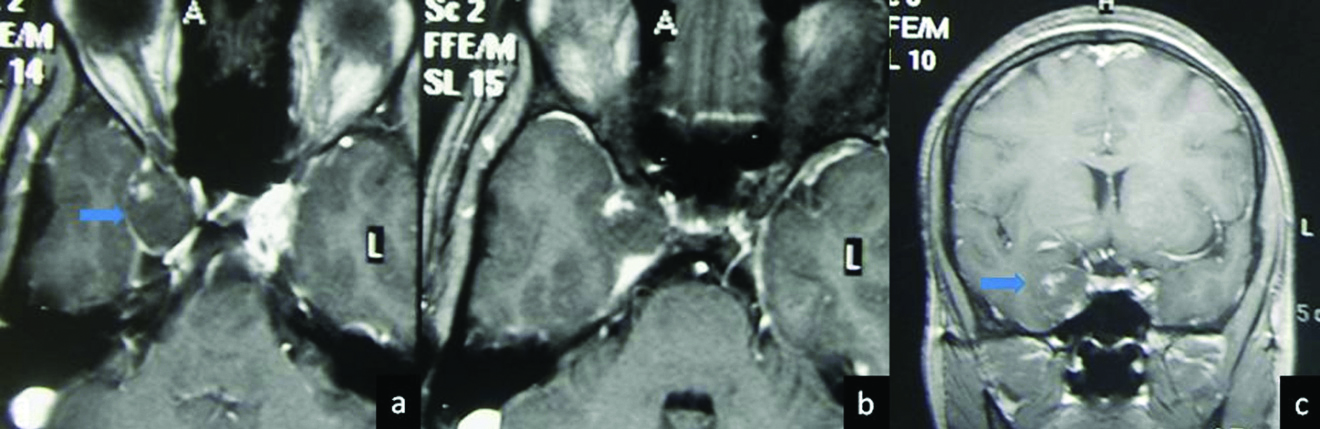
Post-contrast (12 min.) axial (a,b) and coronal (c,d) images shows progressive centripetal filling of the lesion (blue arrow).
Post-contrast (25 min.) axial (a) and coronal (b,c,d) images shows complete homogeneous enhancement of the mass lesion (blue arrow). Note cavernous segment of right Internal Carotid Artery (ICA) is encased and attenuated by the mass lesion.
Case II
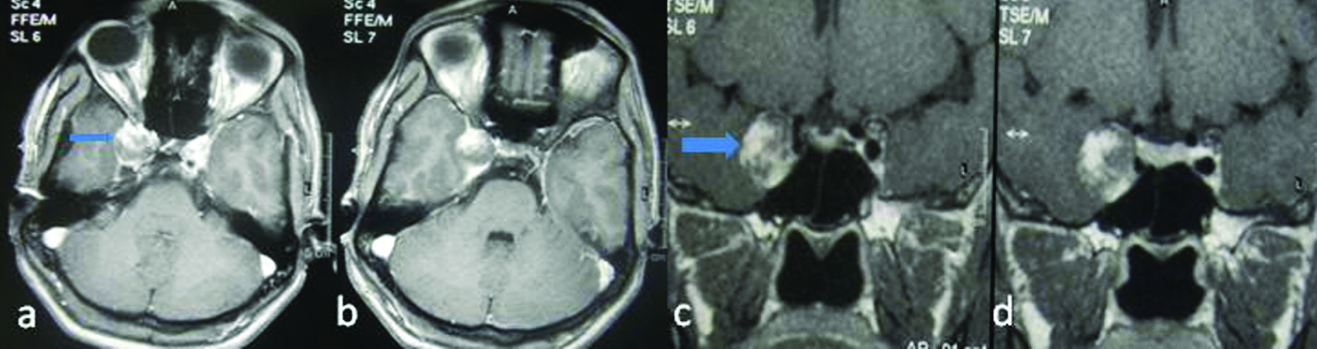
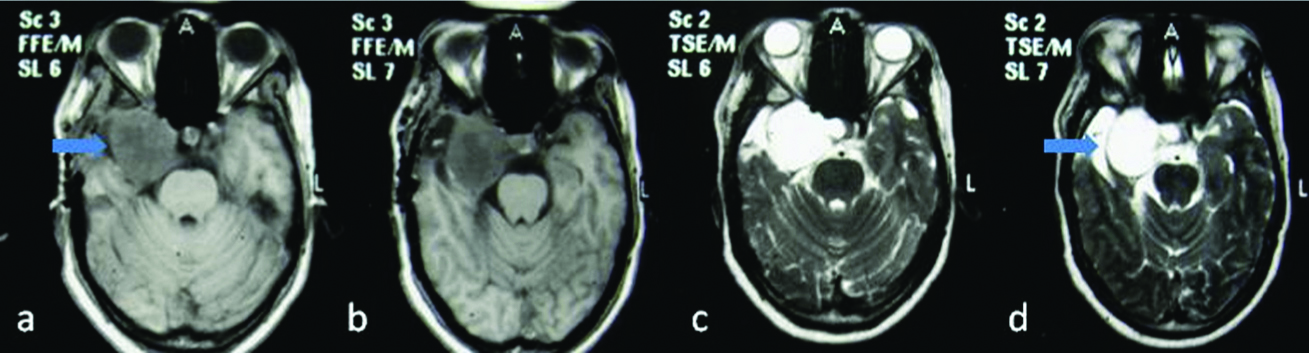
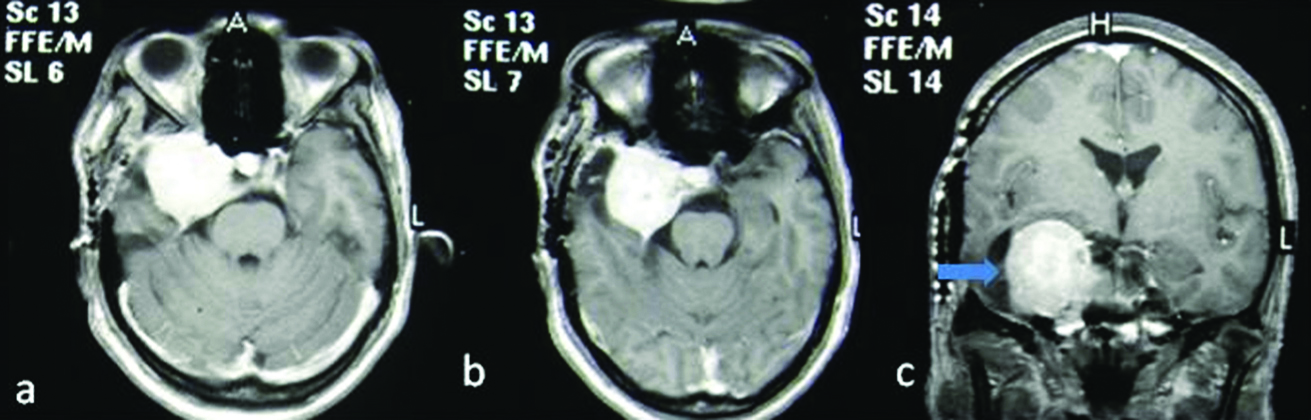
A 45-year-old female presented to the neurology clinic with complaints of persistent headache for six months, lateral deviation and proptosis of the right eye for four months, no visual disturbances were present. Clinical examination showed oculomotor palsy. A computed tomographic scan images of the brain presented by the patient showed a heterogeneously enhancing hyperdense mass in the right parasellar region [Table/Fig-3]. MRI showed a well-defined heterogeneous mass occupying and expanding the right cavernous sinus. The lesion was predominantly iso-hypointense on T1W sequence and markedly hyperintense on T2W sequence [Table/Fig-4a]. The center of the mass appeared hypointense relative to the rest of the lesion on both sequences. The dynamic contrast-enhanced MRI showed marked enhancement of the peripheral component on the initial images [Table/Fig-4b]. Subsequent acquisitions (20 min) showed progressive centripetal filling [Table/Fig-4c], with the delayed enhancement of the center (40 minutes) [Table/Fig-4d]. The diagnosis of haemangioma was suggested based on the characteristic dynamic MRI imaging findings. The patient was fine on two years clinical follow-up. Symptomatic treatment was given for headache.
CECT axial images revealed an intense heterogeneously enhancing mass lesion (blue arrow) in the right parasellar region.
Axial T1W (a,b) and T2W (c,d) images reveal a well-defined mass lesion in right cavernous sinus with iso to hypointense signal on T1W images and markedly hyperintense signal on T2W images.
Post-contrast (immediate) axial (a,b,c) and coronal (d) images reveal strong peripheral enhancement of the lesion with hypodense central area.
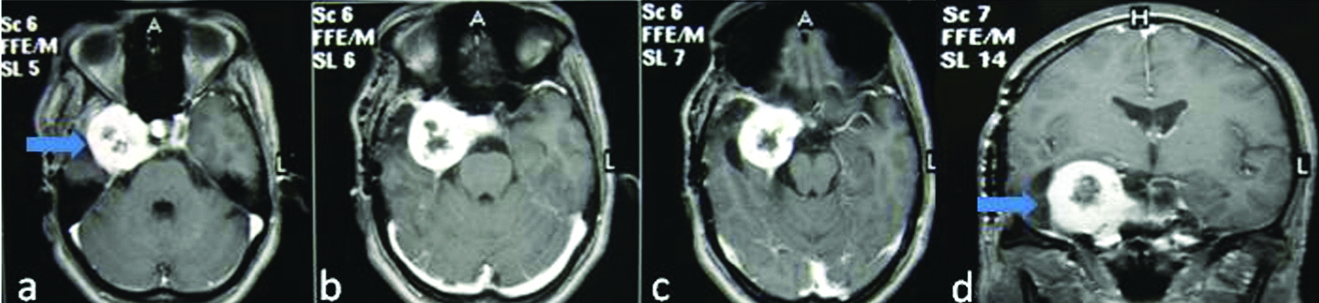
Post-contrast (20 min.) axial (a,b) and coronal (c) images shows near complete filling of the lesion with small non-enhancing central focal area.
Post-contrast (40 min) axial (a,b) and coronal (c) images reveal complete filling with homogeneous enhancement of the lesion.
Case III
A 25-year-old male came with the complaint of headache for last 5-6 months and proptosis for one month. There was no history of trauma and any other co-morbidity. Clinical examination showed redness in the right eye with exophthalmos.
Contrast enhanced MRI showed a well-circumscribed mass lesion in the right cavernous sinus extending to supra-sellar region with contra-lateral displacement of pituitary stalk. The lesion showed characteristic hyperintense signal on T2 and progressive centripetal filling on post-contrast images with delayed homogenous enhancement [Table/Fig-5].
Coronal T2 image (A) shows a well-circumscribed lobulated lesion in right cavernous sinus and extension in supra-sellar extension. Coronal pre-contrast T1 image show hypointense signal, while post-contrast T1 image shows homogenous enhancement.
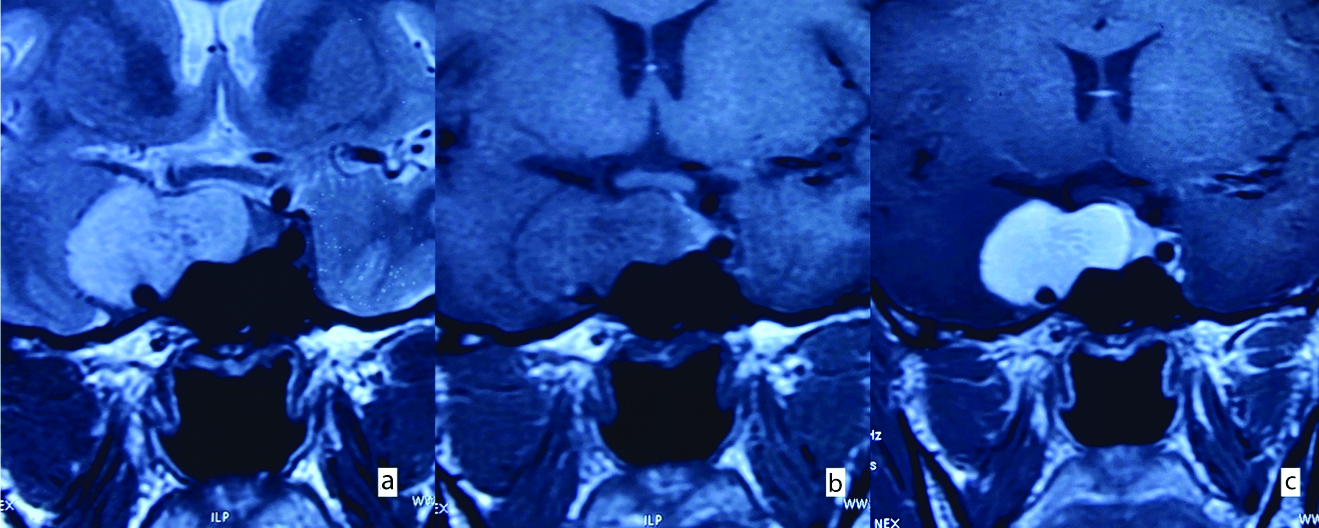
Based on the characteristic MRI findings, diagnosis of haemangioma of cavernous sinus was made. Patient was offered surgery but he refused and lost to follow-up.
Discussion
Cavernous sinus haemangiomas are rare lesions that account for 2-3% of all cavernous sinus mass and less than 1% of all parasellar masses [1, 2]. These lesions are reportedly common in females, probably due to oestrogen playing a role in their formation [1,3]. With increasing size, they grow towards the sellar region and middle cranial fossa and involve adjacent neurovascular structures similar to other neoplasms in this region [3,4]. Progressive ectasia of the blood vessels or their autonomous development at the edges of the lesion is believed to be the likely growth mechanism [5]. Unlike parenchymal haemangioma, the bleeding in the extra-axial haemangioma is rare [1,5].
Clinical symptoms are insidious in onset with progressive clinical deterioration. Common presenting complaints are due to compression upon the optic nerve, optic chiasma, or are related to the involvement of the lateral cavernous sinus wall. The patient may present with retro-orbital pain, visual disturbances, ophthalmoplegia, and other cranial nerve defects. Hypopituitarism, proptosis, anisocoria, obesity, amenorrhoea, and sensory changes in the face may also be seen [2]. Duration of symptoms ranges from a few weeks to 10 years, with an average duration of 20 months [4,6]. Headache was the chief complaint in all three patients in the present study and duration of symptoms varied from six month to one year.
Cavernous haemangiomas consist of a network of dilated thin-walled vessels within no organised elastic lamina and generally are devoid of smooth muscle cells. The vessels are lined by a single layer of endothelium, exhibit variable hyalinisation, and may or may not be separated by intervening fibrous connective tissue. The vessels may be thrombosed consequent to stagnant blood flow, and chronic lesions may show calcification. Often a capsule or pseudo-capsule formed from the duramater may be seen [1]. Large lesions may contain vascular channels with high blood flow. Some haemangiomas may also show evidence of fibrosis, which would represent regressive changes [4].
On CT, haemangiomas appear as an iso to hyperdense mass on the non-contrast study and show marked homogeneous enhancement following contrast administration. Calcification is not common [2,4] and may cause erosion of adjacent bony structures. Without a high degree of suspicion, many of these lesions may be misdiagnosed as meningioma’s, which are common tumours in this region [1,3]. The mass may encase the cavernous part of the ipsilateral Internal Carotid Artery (ICA) with no significant luminal narrowing. This feature helps in differentiating a cavernous haemangioma from a para-sellar meningioma [3,5]. In this series, cavernous ICA showed mild narrowing and medial displacement in all three cases, while in one case, the ICA also appeared encased by the mass lesion.
MRI with contrast-enhanced dynamic imaging remains the gold standard of diagnosis in haemangiomas [2]. These lesions appear as well-defined, well-demarcated mass with hypo to isointense on T1-weighted sequence. Marked homogeneous hyperintensity on T2-weighted sequence is a characteristic feature. On FLAIR sequence, the lesion appears homogeneously hyperintense. The haemangiomas show characteristic pattern of enhancement. Early arterial phase post-contrast sequence typically demonstrate peripheral discontinuous nodular enhancement with progressive centripetal filling-in of the lesion seen in subsequent phases. Delayed images may show complete filling of the lesion with homogenous enhancement. This pattern of progressive centripetal on dynamic MRI differentiate cavernous haemangioma from other lesions seen in this region, and therefore dynamic MRI plays crucial role in the diagnostic work-up of these tumours [7].
Presence of marked tracer accumulation in the lesion in both early and delayed red blood cell pool scintigraphy with 99 mTc-pertechnetate-labeled RBC, similar to hepatic cavernous haemangioma is highly suggestive of cavernous haemangioma of cavernous sinus [8].
Thallium 201 Single-Photon Emission Computerised Tomography (SPECT) shows low uptake within the tumour reflecting its benign nature, while technetium-99m-human serum albumin-diethylenetriaminepenta-acetic acid SPECT shows high uptake within the tumour. Meningioma and malignant tumours usually show very high uptake on Thallium 201 SPECT; thus, SPECT can also be used to differentiate these lesions from other common tumours in this location [9].
Digital Subtraction Angiography (DSA) findings vary. The study may be completely normal or may show an avascular mass obstructing the cavernous sinus [2]. There may also be tumour staining (seen in 2/3rd of all cases) [1,10], with evidence of feeder branches (primarily the meningohypophyseal trunk) arising from the cavernous portion of the ipsilateral ICA, or branches from the External Carotid Artery, such as the accessory middle meningeal artery, being involved. The ICA may or may not be displaced by the lesion [2]. A persistent blush within the lesions has been reported on the arterial phase of angiography due to slow flow [1], the slow flow is responsible for the characteristic hyperintensity seen on proton density and T2 weighted MR images. The venous phase of angiography may show a faint shadow of the lesion [2]. Simard JM et al., in their study demonstrated tumour staining in seven extracerebral cavernous sinus cavernous haemangiomas, while four lesions were reported as avascular masses [11]. On the other hand, Linskey ME and Shekhar LN, reported the appearance of a vascular mass in 20% of cases on angiography [12].
Main differential diagnoses include meningioma, neurofibroma, schwannoma and chondroid lesions. However, neither of these lesions shows progressive centripetal filling on dynamic MRI. Other less common differential includes metastasis, lymphoma, epidermoid, sarcoid granuloma, aspergilloma, Wegener granulomatosis, Tolosa Hunt syndrome, cavernous sinus thrombosis and thrombosed aneurysm of intracavernous ICA [2,13].
This case series demonstrates that cavernous sinus haemangioma can be confidently diagnosed preoperatively by its characteristic MRI features of marked hyperintense signal on T2 weighted sequence, early nodular enhancement, and progressive centripetal filling on dynamic contrast-enhanced MRI which, obviate the need for biopsy.
Conclusion(s)
Extracerebral cavernous sinus haemangiomas are rare lesions that may be misdiagnosed as meningiomas on routine neuroimaging. The sensitivity and specificity of MRI are higher than that of CT and DSA. A parasellar lesion showing a homogeneous markedly increased signal on T2 or proton density-weighted sequences with progressive centripetal “filling-in” with contrast on dynamic imaging should suggest the diagnosis.
[1]. Gonzalez LF, Lekovic GP, Eschbacher J, Coons S, Porter RW, Spetzler RF, Are cavernous sinus hemangiomas and cavernous malformations different entities?Neurosurg Focus 2006 21(1):e610.3171/foc.2006.21.1.716859259 [Google Scholar] [CrossRef] [PubMed]
[2]. Salanitri GC, Stuckey SL, Murphy M, Extracerebral cavernous hemangioma of the cavernous sinus: Diagnosis with MR imaging and labeled red cell blood pool scintigraphyAm J Neuroradiol 2004 25(2):280-84. [Google Scholar]
[3]. Mendonça JL, Viana SL, Matsumine M, Silva RF, Viana MA, Freitas FM, Cavernous angioma of the cavernous sinus: Imaging findingsArq Neuropsiquiatr 2004 62(4):1004-07.Epub 2004 Dec 1510.1590/S0004-282X200400060001315608959 [Google Scholar] [CrossRef] [PubMed]
[4]. Souto AA, Marcondes J, Silva MR, Chimelli L, Sclerosing cavernous hemangioma in the cavernous sinus: Case reportSkull Base 2003 13(2):93-99.10.1055/s-2003-40599 [Google Scholar] [CrossRef]
[5]. Sohn CH, Kim SP, Kim IM, Lee JH, Lee HK, Characteristic MR imaging findings of cavernous hemangiomas in the cavernous sinusAm J Neuroradiol 2003 24(6):1148-51. [Google Scholar]
[6]. Park CK, Lee MS, Kim YG, Kim DH, Cavernous hemangioma in the middle cranial fossa & cavernous sinusJ Korean Neurosurg Soc 2006 40(4):277-80. [Google Scholar]
[7]. Kazumi I, Yoshitaka Y, Yusuke S, Yuko Y, Takuya K, Cavernous sinus cavernous hemangioma suspected by dynamic MRINeuro-Ophthalmology Japan 2000 17(3):315-22. [Google Scholar]
[8]. Ivanov P, Chernov M, Hayashi M, Nakaya K, Izawa M, Murata N, Low-dose gamma knife radiosurgery for cavernous sinus hemangioma: Report of 3 cases and literature reviewMinim Invasive Neurosurg 2008 51(3):140-46.10.1055/s-2008-106534618521784 [Google Scholar] [CrossRef] [PubMed]
[9]. Seo Y, Fukuoka S, Sasaki T, Takanashi M, Hojo A, Nakamura H, Cavernous sinus hemangioma treated with gamma knife radiosurgery: Usefulness of SPECT for diagnosis-Case reportNeurol Med Chir (Tokyo) 2000 40(11):575-80.10.2176/nmc.40.57511109795 [Google Scholar] [CrossRef] [PubMed]
[10]. Yang MS, Chen CC, Chen WH, Hung HC, Lee SK, Radiological appearance of Extra-axial CNS hemangiomasChin J Radiol 2002 27:183-90. [Google Scholar]
[11]. Simard JM, Garcia-Bengochea F, Ballinger WE Jr, Mickle JP, Quisling RG, Cavernous angioma: A review of 126 collected and 12 new clinical casesNeurosurgery 1986 18(2):162-72.10.1227/00006123-198602000-000083960293 [Google Scholar] [CrossRef] [PubMed]
[12]. Linskey ME, Shekhar LN, Cavernous sinus hemangiomas: A series, a review and a hypothesisNeurosurgery 1992 30:101-08.10.1097/00006123-199201000-00018 [Google Scholar] [CrossRef]
[13]. Lee JH, Lee HK, Park JK, Choi CG, Suh DC, Cavernous sinus syndrome: Clinical features and differential diagnosis with MR imagingAJR 2003 181(2):583-90.10.2214/ajr.181.2.181058312876052 [Google Scholar] [CrossRef] [PubMed]