Co-existing Tubercular Pleural Effusion and Visceral Larva Migrans in a Patient with Hypereosinophilia: A Rare Case
Taranpreet Kaur1, Nitin Kumar Bansal2, Kuldeep Goyal3, Jaykrat Chaudhary4
1 Assistant Professor, Department of Medicine, Sri Guru Ram Rai Institute of Medical and Health Sciences, Dehradun, Uttarakhand, India.
2 Professor, Department of Medicine, Sri Guru Ram Rai Institute of Medical and Health Sciences, Dehradun, Uttarakhand, India.
3 Resident, Department of Medicine, Sri Guru Ram Rai Institute of Medical and Health Sciences, Dehradun, Uttarakhand, India.
4 Resident, Department of Medicine, Sri Guru Ram Rai Institute of Medical and Health Sciences, Dehradun, Uttarakhand, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Taranpreet Kaur, G-20, Sri Guru Ram Rai Institute of Medical and Health Sciences Campus, Patel Nagar, Dehradun, Uttarakhand, India.
E-mail: taran30jul@gmail.com
Eosinophilic pleural effusions accounts for 5-16% of all the cases of pleural effusion. Here the authors present a case of 21 years old male patient, with right-sided chest pain in whom peripheral blood eosinophilia along with eosinophilic pleural effusion were found after a series of relevant investigations and two causative factors were found for same i.e., Visceral Larva Migrans (VLM) and tubercular pleural effusion. Both of them individually can cause hypereosinophilia, but presence of them together makes this case rare and interesting.
Chest x-ray, Eosinophilic pleural effusion, Tuberculosis
Case Report
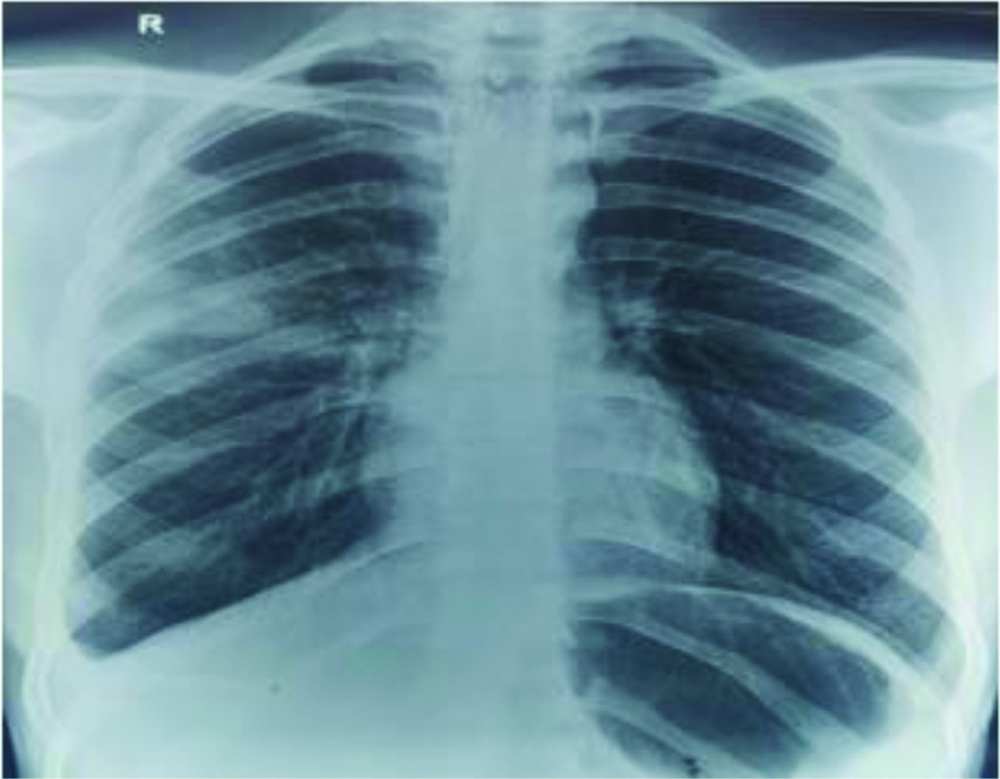
A 21-year-old male, student, presented with the complaint of right-sided chest pain and low grade fever since one month. There was no history of night sweats, cough, weight loss, rash, exposure to pets, drug intake or any allergy. He was vegetarian with no history of any addictions. No past history of any chronic illness or tuberculosis. Family history was not significant. On examination, he had average built with BMI of 18.2. Chest examination revealed dull note in right infrascapular area with decreased air entry on auscultation. His preliminary investigations revealed: Haemoglobin (Hb): 13.4 g/dL, Total Leucocyte Count (TLC): 24,310/cumm with 53% eosinophils, Absolute Eosinophil Count (AEC): 15,200/cumm, Chest X-ray: right-sided pleural effusion [Table/Fig-1]. Ultrasonography (USG) guided thoracocentesis revealed Glucose: 98 g/dL, proteins: 4.7 g/dL, TLC: 1300/cumm, Differential Leucocyte Count (DLC): Polymorphs 15%, Lymphocytes 56% and Eosinophils 29%, Adenosine Deaminase (ADA): 49.15. Mantoux test skin of induration was 18 mm. Anti Nuclear Antibody (ANA) profile was negative.
Chest X ray showing mild right-sided pleural effusion on presentation.

On the basis of these reports, patient was started on Anti-Tubercular Treatment (ATT) consisting of Isoniazid 300 mg, Rifampicin 450 mg, Ethambutol 800 mg and Pyrazinamide 1500 mg along with steroids (prednisolone 1 mg/kg/day).
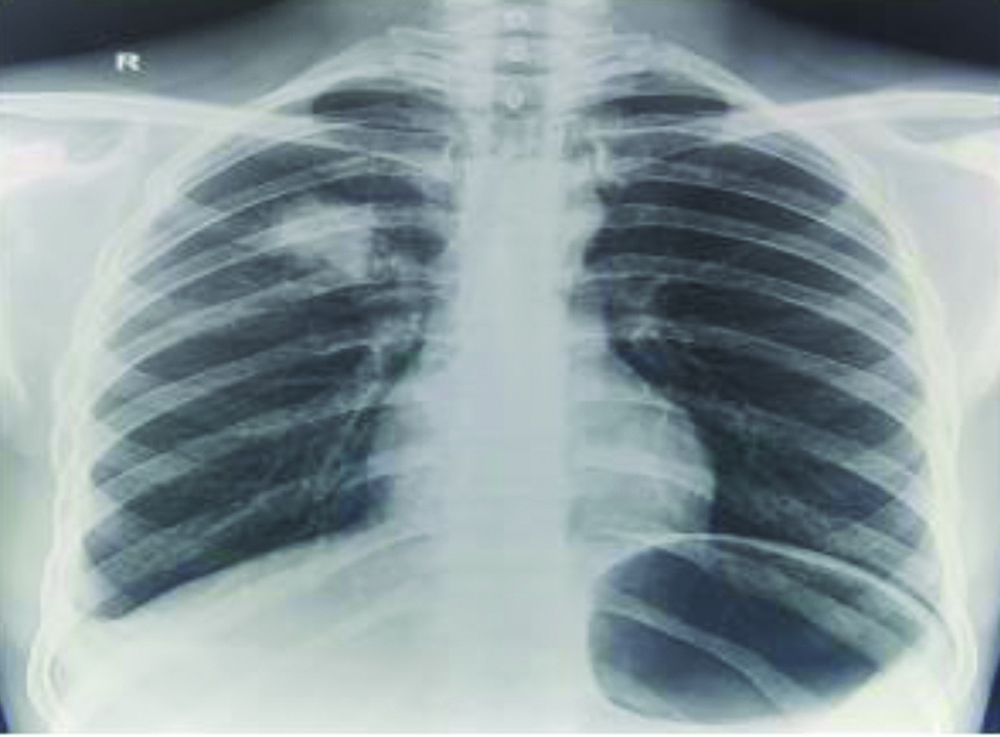
Follow-up: After one month, when the patient came for follow up, he was complaining of right-sided chest pain. On examination, there was dull note and decreased air entry in the right basal area. His AEC had come down to 4500/cumm from 15,200/cumm earlier. His CXR (Chest X-ray) showed a peripheral homogenous opacity in right upper zone besides right pleural effusion [Table/Fig-2]. Contrast Enhanced Computed Tomography (CECT) chest was done which revealed linear parenchymal opacities with surrounding patchy ground glass haziness involving anterior segment of right upper zone, superior and postero-basal segment of right lower zone suggesting the possibility of VLM [Table/Fig-3]. Serology (Antibody against Toxocara and Ascaris) could not be sent due to financial reasons. Stool for ova/cyst was negative. So the patient was started on Tab Albendazole 400 mg BD along with steroids. ATT was stopped considering this whole picture to be due to VLM.
Chest X-ray showing peripheral homogenous opacity in right upper zone and right-sided pleural effusion after one month.
CECT chest showing linear opacity in superior and postero-basal segment of right lower lobe at one month of follow-up.

After one month and 10 days, the right-sided chest pain had decreased in intensity but on examination the air entry was still reduced in right basal area. Patient’s AEC further declined to 3400/cumm and CXR showed a homogenous opacity in right upper zone which was different from the previous one which could no more be visualised now and right pleural effusion was also there [Table/Fig-4]. High Resolution CT chest revealed a new lesion with linear peri-bronchial opacity with area of consolidation and minimal surrounding ground glass haziness in posterior segment of right upper lobe and superior segment of right lower lobe. Previous lesion showed significant interval reduction with near complete resolution of ground glass haziness. Right pleural effusion showed mild interval reduction. Albendazole was continued for two weeks and steroids for four weeks.
Chest X ray showing homogenous opacity in right upper zone along with right-sided pleural effusion after one month and 10 days.
After two months, patient had only mild right-sided chest pain along with constitutional symptoms like low grade fever, malaise and decreased appetite. Air entry was also reduced in right basal area. His AEC was 164/cumm and CXR was showing only right-sided pleural effusion [Table/Fig-5]. So again USG guided thoracocentesis was done which revealed Glucose: 20 mg/dL, Protein: 8.1 mg/dL, TLC: 4000/cumm, DLC: Polymorphs 20%, Lymphocytes 75% and Eosinophils 5%, ADA was 65. These reports were strongly suggestive of tubercular picture. Therefore, the patient was started on Anti-Tubercular Therapy consisting of Isoniazid 300 mg, Rifampicin 450 mg, Ethambutol 800 mg and Pyrazinamide 1500 mg.
Chest X ray showing right-sided pleural effusion after two months on follow-up.

After four months, patient was asymptomatic and feeling better. Air entry was equal on both sides and no dull note was there. Chest X-ray revealed blunting of right costophrenic angle but on USG thorax, no fluid was there and it was most likely some pleural thickening. Patient was started on continuation phase of ATT with Isoniazid 300 mg, Rifampicin 450 mg and Ethambutol 800 mg.
After eight months, patient was completely relieved of his symptoms and completed his ATT course of six months without any side-effects.
Discussion
Eosinophilic pleural effusion is defined by the presence of >10% of eosinophils in the pleural fluid [1]. Various causes for Eosinophilic pleural effusion are Malignancy, Infections, Post-traumatic, Congestive heart failure and Connective tissue diseases and about 14% remain idiopathic [2,3]. Parasitic infections like filariasis, ascariasis, strongyloidiasis and some trematodes and cestodes can lead to eosinophilic pleural effusion [4].
Differentiating eosinophilic pleural effusion due to tubercular and parasitic can be confusing at times. Although ADA levels are raised in both tubercular and parasitic pleural fluid but, predominant lymphocytes and low eosinophil count favours tubercular and predominant eosinophils with low lymphocytes favour eosinophilic picture of parasitic. Mean ADA levels are higher in tubercular than parasitic [5].
The case described above is also an interesting one in view of the fact that initial eosinophilic pleural effusion along with the migrating nodular lesions in lung can be attributed to be due to VLM. A study by Sakai S et al., found 5 out of 6 patients with Visceral Larval Migrans had normal chest X-ray and it was detected on CT [6]. Similarly in the present case, no lesion was visualised in initial chest X-ray but appeared one month later. VLM is usually diagnosed on clinical history, eosinophilia, histopathologic examination, X-rays and CT [7].
The persistence of constitutional symptoms along with pleural effusion despite giving steroids and albendazole points to some other coincidental cause. Lymphocytic predominant picture in effusion with raised ADA levels leaves little doubt about the effusion being tubercular. Co-infection of Tuberculosis and various parasitic infections like malaria, filariasis, intestinal helminthes, toxoplasma, toxocara etc., have been described [8-10]. But the co-infection of extrapulmonary TB with VLM is very rare.
Certain investigations like serology studies for ascaris, toxocara etc., along with TB PCR of pleural fluid couldn’t be sent due to financial constraints. The diagnosis had to be supported strongly by clinical picture and resolution with treatment at proper regular follow-ups.
Conclusion(s)
Presentation of Visceral Larva Migrans (VLM) is similar to other infectious diseases. However, clinical history and examination supplemented with chest X-rays and CT scans lead us to the diagnosis. Also, this case underlines the importance of regular follow-up of patient as later on, the diagnosis of tubercular pleural effusion unfolded.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 15, 2020
Manual Googling: Nov 20, 2020
iThenticate Software: Dec 11, 2020 (13%)
[1]. Martinez-Garcia MA, Cases-Viedma E, Cordero-Rodriguez PJ, Hidalgo-Ramírez M, Perpiñá-Tordera M, Sanchis-Moret F, Diagnostic utility of eosinophils in the pleural fluidEur Respir J 2000 15(1):166-69.10.1183/09031936.00.1511660010678640 [Google Scholar] [CrossRef] [PubMed]
[2]. Oba Y, Abu-Salah T, The prevalence and diagnostic significance of Eosinophilic pleural effusions: A meta-analysis and systematic reviewRespiration 2012 83:198-208.10.1159/00032720021576924 [Google Scholar] [CrossRef] [PubMed]
[3]. Krenke R, Nasilowski J, Korczynski P, Gorska K, Przybylowski T, Chazan R, Incidence and etiology of Eosinophilic pleural effusionEur Respir J 2009 34:1111-17.Available at: DOI: 10.1183/09031936.0019770810.1183/09031936.0019770819386682 [Google Scholar] [CrossRef] [PubMed]
[4]. Wang J, Luo W, Shen P, He J, Zeng Y, Retrospective study of pleural parasitic infestations: A practical diagnostic approachBMC Inf Dis 2019 19(576):01-07.10.1186/s12879-019-4179-931272486 [Google Scholar] [CrossRef] [PubMed]
[5]. Shuai T, Yu Z, Chaomin W, Distinguishing tuberculosis pleural effusionfrom parasitic pleural effusion using pleural fluid characteristics: A case control studyMedicine 2019 98(5):e1423810.1097/MD.000000000001423830702582 [Google Scholar] [CrossRef] [PubMed]
[6]. Sakai S, Shida Y, Takahashi N, Yabuuchi H, Soeda H, Okafuji T, Pulmonary lesions associated with Visceral Larva Migrans due to Ascaris suum or Toxocara canis: imaging of six casesAm J Roentgenol 2006 186:1697-702.10.2214/AJR.04.150716714661 [Google Scholar] [CrossRef] [PubMed]
[7]. Turrientess MC, Perez DE, Ayala A, Norman F, Navarro M, Perez-Molina JA, Visceral larva migrans in migrants from Latin AmericaEmerg Infect Dis 2011 17(7):1263-65.10.3201/eid1707.10120421762582 [Google Scholar] [CrossRef] [PubMed]
[8]. Li X, Zhou X, Coinfection of tuberculosis and parasitic diseases in humans: A systematic reviewParasites & Vectors 2013 6:7910.1186/1756-3305-6-7923522098 [Google Scholar] [CrossRef] [PubMed]
[9]. Guneratne R, Mendis D, Bandara T, Fernando SD, Toxoplasma, toxocara and tuberculosis co-infection in a four-year-old childBMC Pediatr 2011 11:4410.1186/1471-2431-11-4421615887 [Google Scholar] [CrossRef] [PubMed]
[10]. Manuel Ramos J, Reyes F, Tesfamariam A, Intestinal parasites in adults admitted to a rural Ethiopian hospital: Relationship to tuberculosis and malariaScand J Infect Dis 2006 38(6-7):460-62.10.1080/0036554050052518716798694 [Google Scholar] [CrossRef] [PubMed]