A Cadaveric Study on Lumbar Spinous Process Fusion: Risk Factor for Wrong Level Spinal Surgeries
Priyanka N Sharma1, Manoj M Kulkarni2, AR Gandotra3
1 Ph.D. Scholar (Assistant Professor), Department of Anatomy, Smt. B.K. Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth, Vadodara, Gujarat, India.
2 Professor, Department of Anatomy, Smt. B.K. Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth, Vadodara, Gujarat, India.
3 Professor and Head, Department of Anatomy, Smt. B.K. Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth, Vadodara, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manoj M Kulkarni, Professor, Department of Anatomy, Smt. B.K. Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth, Vadodara-391760, Gujarat, India.
E-mail: drmanojkulkarni999@gmail.com
Introduction
The fusion of Lumbar Spinous Processes (LSP) of adjacent vertebrae may lead to errors in determining the correct spinal level. This may result in wrong level spinal surgeries around the lumbar region.
Aim
To determine the prevalence of fusion between adjacent LSP.
Materials and Methods
This study was a prospective observational study done in the Department of Anatomy, Smt. B.K. Shah Medical Institute and Research Centre, Vadodara, Gujarat, India. The present study had examined the lumbar spines in 30 formalin preserved cadavers. The fusion between the LSP of adjacent vertebrae was recorded after the removal of soft tissue from L1 to S1 vertebrae.
Results
The present study found the fusion between the adjacent LSP in 11 (36.67%) cadavers (08 males; 03 females). The fusion between the adjacent LSP, from L4 to S1 vertebrae, was found in 10% of cadavers and was the most common pattern. The fusion between the adjacent LSP was more common in males (53.3%) compared to females (20%).
Conclusion
The occurrence of fusion between the adjacent LSP is not uncommon.
Ligation, Lumbar vertebra, Neurosurgeon, Sacralisation, Vertebra column
Introduction
Lumbar vertebra has a vertebral body and a vertebral arch. The vertebral arch consists of a pair of pedicles and a pair of laminae, which encircles the vertebral foramen. A lumbar vertebra has a thick and stout vertebral body, a blunt, quadrilateral Spinous Process (SP) for the attachment of strong lumbar muscles, and articular processes.
Spine surgery at the wrong level is an unintended, yet not so uncommon mistake committed by surgeons around the world. This not only requires the patients to undergo additional surgeries but many times results in litigations. This type of error can cost very dearly to the financial and professional well-being of the surgeons [1]. Jhawar BS et al., have reported the incidence of wrong level lumbar spinal surgeries to be 12.8 per 10,000 surgeries [2]. Many researchers have tried to enlist the factors that have the potential to mislead the surgeons to commit this error [1-3]. Anatomical variations are major risk factors that make the determination of the correct spinal level very challenging [3-6].
The LSP is relatively superficial and easy to access. However, the fusion of SP of adjacent lumbar vertebrae is one such factor that may cause errors in counting of lumbar vertebrae which in turn may result in operating at the wrong spinal level [3]. Other anatomical variations which may lead to errors in counting of vertebral level include presence of cervical ribs, absence of thoracic ribs, hemivertebrae, sacralisation of lumbar vertebra etc., [3-6]. The preoperative assessment of patient with respect to these anatomical variations will help to prevent the errors in counting of vertebral level.
Operating at the wrong level is avoidable at least in some cases if the surgeon recognises the risk factors. The present study attempted to determine the prevalence of fusion of SP of adjacent lumbar vertebrae, which is one of the risk factors for wrong level lumbar spinal surgery. The data will be useful to determine the necessity to devise a protocol to look for this variation preoperatively, in patients posted for lumbar spinal surgery.
Materials and Methods
This prospective observational cadaveric study was carried out at the Department of Anatomy at Smt BK Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth, Gujarat, India from August 2018-2020. Ethical approval to undertake the present study was obtained from the Institution Ethical Committee (SVIEC No: Medical/PhD/18005).
The specimens without any obvious externally visible deformity or signs of injury, pathology, or surgical procedures were included. The SP of lumbar vertebrae was examined in 30 formalin-fixed adult human cadavers (15 females and 15 males). The cadavers were placed in a prone position on a flat table with hips extended. With midline incision around the lumbar region, the superficial and deep muscles of the back were identified and removed until the lumbar vertebral column was exposed. The SP of all the lumbar vertebrae was cleaned in each specimen and was observed to find out the occurrence of fusion amongst adjacent SP.
Statistical Analysis
The data was recorded and analysed using Statistical Package for the Social Sciences (SPSS) version 23. Data was presented as absolute numbers and percentages.
Results
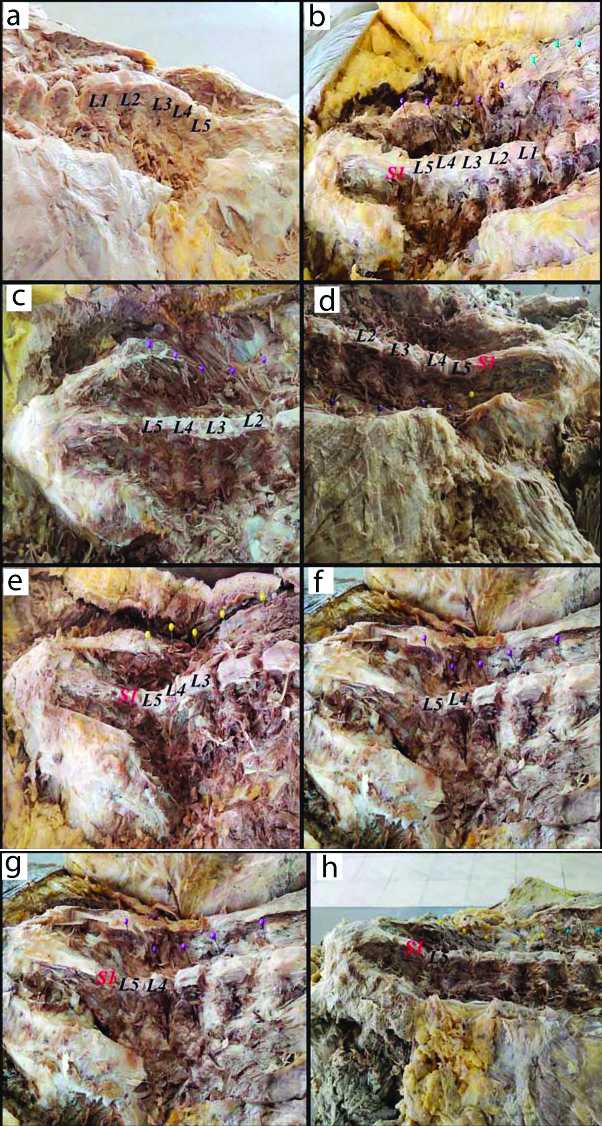
The present study has examined the lumbar spine in 30 adult cadavers (range of 60-95 years, mean of 77.5 years). The fusion between adjacent SP was noted in 11 cadavers (36.67%). The fusion of the SP of L4 to S1 was most common and was found in three specimens [Table/Fig-1]. The fusion of the adjacent LSP was more common in males (53.3%) compared to females (20%) [Table/Fig-2].
Showing fusion of spinous process of lumbar vertebra: a) Fusion of L1 to L5 spinous process; b) Fusion of L1 to S1 spinous process; c) Fusion of L2 to L5 spinous process; d) Fusion of L2 to S1 spinous process; e) Fusion of L3 to S1 spinous process; f) Fusion of L4 to L5 spinous process; g) Fusion of L4 to S1 spinous process; h) Fusion of L5 to S1 spinous process.
Frequency of fusion of Lumbar Spinous process (LSP).
| Level of fusion of the spinous processes | Sample size (Total no=30, Male 15 and Female 15) |
|---|
| Total no. of the specimen showing fusion (%) | Male specimen showing fusion (%) | Female specimen showing fusion (%) |
|---|
| L1 to L5 | 1 (3.3%) | 1 (6.7%) | 0 (0%) |
| L1 to S1 | 1 (3.3%) | 1 (6.7%) | 0 (0%) |
| L2 to L5 | 1 (3.3%) | 1 (6.7%) | 0 (0%) |
| L2 to S1 | 1 (3.3%) | 1 (6.7%) | 0 (0%) |
| L3 to S1 | 1 (3.3%) | 0 (0%) | 1 (6.7%) |
| L4 to L5 | 1 (3.3%) | 0 (0%) | 1 (6.7%) |
| L4 to S1 | 3 (10%) | 3 (20%) | 0 (0%) |
| L5 to S1 | 2 (6.7%) | 1 (6.7%) | 1 (6.7%) |
The fusion of the SP was so complete that no trace of the line of fusion was evident in any specimen. The transverse processes of none of the adjacent lumbar vertebrae were found to be fused.
Discussion
The problem of Wrong Level Spinal Surgery (WLSS) is a unique surgical problem with detrimental consequences for both the patient and the surgeon. WLSS occurs when a surgeon performs decompression, resection, or reconstructive procedure on an unintended anatomic location along the spinal axis [7]. The knowledge of anatomical variations of spine may help in reducing the incidence of WLSS. The present study has attempted to determine the prevalence of fusion of LSP in cadavers at the Department of Anatomy at the study institute.
Although the exact incidence of WLSS remains unknown, most researchers agree that the lumbar level is more prone to WLSS. Mody M et al., had done a questionnaire-based survey among members of the American Academy of Neurosurgeons [8]. They reported that the prevalence of wrong level spinal operations to be 1 in 3110 procedures. Also, out of these wrong level operations, majority were performed on the lumbar region (71%), followed by the cervical (21%), and the thoracic (8%) regions. Jhawar BS et al., have also reported that the WLSS are more common in the lumbar region (12.8/10 000) than that of the cervical region (7.6/10 000) [2]. Ammerman JM et al., [9] have reported the incidence of wrong level lumbar spinal surgeries to be as high as 15% while Barrios C et al., have reported it to be around 3.3% [10].
Abnormal anatomy is one of the risk factors for WLSS [4]. The SP of vertebrae, because of its readily accessible location, is commonly used for counting vertebral level. However, their fusion can very easily misguide the surgeon. The aetiology of fusion may be congenital, acquired, or surgical.
There is a wide variation in the prevalence of lumbar vertebral fusion reported by various researchers [Table/Fig-3] [11-14]. This is partly due to the methods used for calculation of prevalence rate. The denominator used for calculation of prevalence rate by Sar M et al., and Vikani S and Javia MD, was the number of vertebrae [11,12]; while the studies of Deepa M and Rajasekar SS, and Sharma M et al., have used number of vertebral columns as the denominator [13,14]. The present study has observed fusion between adjacent LSP in 36.67% of the specimen, which is quite higher than other studies. This may be illusory as the findings are not confirmed by the X-rays.
Comparison of the index study with literature [11-14].
| Study | Sample | Data for fusion (%) |
|---|
| Present study | 30 Lumbar spine specimens | 36.67 |
| Sar M et al., [11] | 399 Dry vertebrae | 0.75 |
| Vikani SK and Javia MD [12] | 185 Dry vertebrae | 1.08 |
| Deepa S and Rajasekar SS [13] | 50 Dry vertebral columns | 2 |
| Sharma M et al., [14] | 48 Dry vertebral columns | 2.08 |
The present study has also found that there are wide variations in the number of adjacent LSP involved in fusion. Both these factors viz., high prevalence and the variable pattern of fusion of LSP may make the counting of the lumbar level extremely difficult for clinicians. This can very easily lead to WLSS having profound medical and legal consequences [10,15].
Considering the wide variations amongst study reports about prevalence of lumbar vertebral fusion in the Indian population, the authors recommend preoperative and intraoperative imaging in each patient to reduce the incidence of WLSS.
Limitation(s)
The findings were not confirmed with the X-ray of the concerned region. So, the higher prevalence may be illusory.
Conclusion(s)
The fusion between the LSP is common among the Indian adult population. The number of lumbar vertebrae involved in fusion also varies amongst individuals. Preoperative and intraoperative imaging in patients is recommended to reduce the incidence of wrong level lumbar spinal surgeries.
The authors also suggest that a large sample sized multicentric, prospective study among Indian adult population, with use of X-ray of lumbar spine, will help to determine the exact prevalence of the fusion of adjacent LSP in the population.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 26, 2020
Manual Googling: Nov 17, 2020
iThenticate Software: Dec 11, 2020 (15%)
[1]. Hsiang J, Wrong-level surgery: A unique problem in spine surgerySurg Beurol Int 2011 2:4710.3171/SPI-07/11/46717977186 [Google Scholar] [CrossRef] [PubMed]
[2]. Jhawar BS, Mitsis D, Duggal N, Wrong-sided and wrong-level neurosurgery: A national surveyJ Neurosurg Spine 2007 7(5):467-72. [Google Scholar]
[3]. Shah M, Halalmeh DR, Sandio A, Tubbs RS, Moisi MD, Anatomical variations that can lead to spine surgery at the wrong level: Part i, cervical spineCureus 2020 12(6):e866710.7759/cureus.8667 [Google Scholar] [CrossRef]
[4]. Lindley EM, Botolin S, Burger EL, Patel VV, Unusual spine anatomy contributing to wrong level spine surgery: A case report and recommendations for decreasing the risk of preventable ‘never events’Patient Saf Surg 2011 5(1):3310.1186/1754-9493-5-3322168745 [Google Scholar] [CrossRef] [PubMed]
[5]. Malanga GA, Cooke PM, Segmental anomaly leading to wrong level disc surgery in cauda equina syndromePain Physician 2004 7(1):107-10.10.36076/ppj.2004/7/107 [Google Scholar] [CrossRef]
[6]. Kubavat D, Nagar SK, Malukar O, Shrimankar P, Patil S, A study of sacralization of fifth lumbar vertebra in GujaratNat J Med Res 2012 2(2):211-13. [Google Scholar]
[7]. Palumbo MA, Bianco AJ, Esmende S, Daniels AH, Wrong-site spine surgeryJ Am Acad Orthop Surg 2013 21:312-20.10.5435/JAAOS-21-05-31223637150 [Google Scholar] [CrossRef] [PubMed]
[8]. Mody M, Nourbakhsh A, Stahl D, Gibbs M, Alfawareh M, Garges K, The prevalence of wrong level surgery among spine surgeonsSpine 2008 33:194-98.10.1097/BRS.0b013e31816043d118197106 [Google Scholar] [CrossRef] [PubMed]
[9]. Ammerman JM, Ammerman MD, Dambrosia J, Ammerman BJ, A prospective evaluation of the role for intraoperative x-ray in lumbar discectomy. Predictors of incorrect level exposureSurg Neurol 2006 66:470-73.10.1016/j.surneu.2006.05.06917084188 [Google Scholar] [CrossRef] [PubMed]
[10]. Barrios C, Ahmed M, Arrótegui J, Björnsson A, Gillström P, Microsurgery versus standard removal of the herniated lumbar disc: A 3-year comparison in 150 casesActa Orthop Scand 1990 61:399-403.10.3109/174536790089935492239161 [Google Scholar] [CrossRef] [PubMed]
[11]. Sar M, Mishra SK, Behera S, Bara DP, Dehury MK, Vertebral synostosis: A study in dried vertebrae of western odisha populationIOSR Journal of Dental & Medical Science 2017 16(8):44-48. [Google Scholar]
[12]. Vikani SK, Javia MD, Vertebral synostosis and its clinical importance: Study in dried vertebrae of gujarat populationInternational Journal of Anatomy, Radiology and Surgery 2019 8(2):AO33-37. [Google Scholar]
[13]. Deepa S, Rajasekar SS, Series of vertebral synostosis-Clinically impliedIJHBMR 2014 03(1):36-40. [Google Scholar]
[14]. Sharma M, Baidwan S, Jindal AK, Gorea RK, A study of vertebral synostosis and its clinical significanceJ Punjab Acad Forensic Med Toxicol 2013 13(1):20-24. [Google Scholar]
[15]. Bono CM, Vaccaro AR, Interspinous process devices in the lumbar spineJ Spinal Disord Tech 2007 20(3):255-61.10.1097/BSD.0b013e318033135217473649 [Google Scholar] [CrossRef] [PubMed]