Tubercular Iliopsoas Abscess: A Rare Case Report
Sunil Kumar Patanaik1, Chaitali Pattanayak2, Vartika Srivastava3, Sougata Sarkar4
1 Associate Professor, Department of Surgery, Kalinga Institute of Medical Sciences (KIMS), Bhubaneswar, Odisha, India.
2 Professor, Department of Pharmacology, Kalinga Institute of Medical Sciences (KIMS), Bhubaneswar, Odisha, India.
3 Assistant Professor, Department of Pharmacology, Kalinga Institute of Medical Sciences (KIMS), Bhubaneswar, Odisha, India.
4 DM Resident, Department of Pharmacology, School of Tropical Medicine, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Chaitali Pattanayak, Department of Pharmacology, Kalinga Institute of Medical Sciences (KIMS), Campus 5, Patia, Bhubaneswar, Odisha, India.
E-mail: chaitali.pattanayak@kims.ac.in
A psoas (or iliopsoas) abscess is an accumulation of pus in the region of iliopsoas muscle compartment. In regions where Mycobacterium tuberculosis is endemic, this is a frequent cause of psoas abscess. When an inguinal mass in a patient with a psoas abscess is painless, tuberculosis is a more likely cause than a bacterial infection. Here, the author report a rare case of psoas abscess of tubercular origin in a 31-year-old patient who presented with back pain and limping, with features of inflammation. Diagnosis was done based on history, physical examination, ultrasonography, microbiological investigation and Contrast-Enhanced Computed Tomography (CECT) scan of abdomen which revealed a large psoas abscess caused by M. tuberculosis. Patient was diagnosed with a psoas abscess due to Mycobacterium tuberculosis with secondary infection and treated empirically with Directly Observed Treatment Short-Course (DOTS) category I and antibiotics. He presented again with a chest abscess due to Multidrug-Resistant (MDR) tuberculosis.
Contrast-enhanced computed tomography scan, Incision and drainage, Psoas abscess, Tuberculosis
Case Report
A 31-year-old male from Cuttack, Odisha, India presented to the OPD with a history of pain and swelling in the right side of abdomen and upper part of right thigh for 20 days. There was difficulty in walking, gradual loss of weight and appetite. He felt feverish particularly during the evening hours. The pain over the swelling was of throbbing and intermittent nature with no radiation to any other body parts. There was no history of hypertension, diabetes mellitus, bronchial asthma and tuberculosis. There was no previous history of hospitalisation or surgical intervention. He was not addicted to smoking or alcohol.
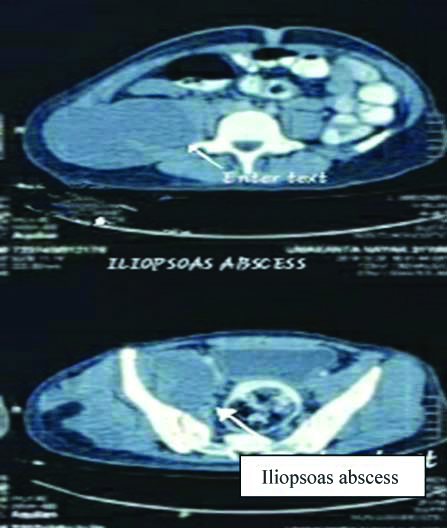
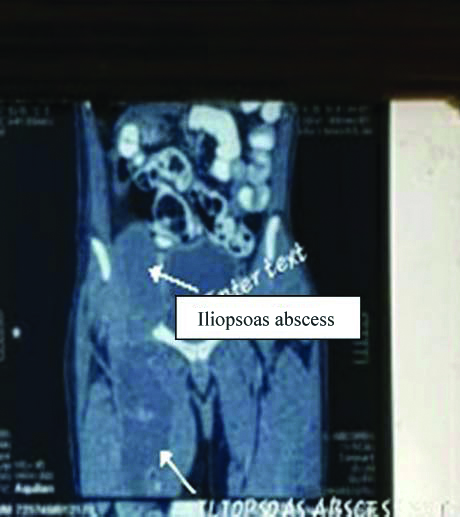
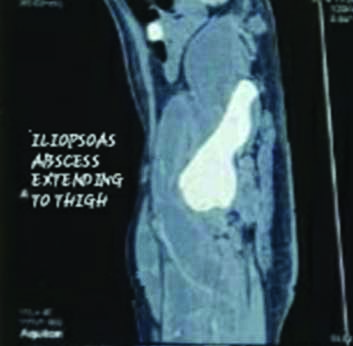
On examination, the patient was febrile (~100°F), blood pressure was within normal limits. His gait was antalgic on the right side. On auscultation, bilateral vesicular breath sounds were heard. No added sounds were found, no adenopathy was detected. A swelling of about 15×6 cm size was present on the right side of abdomen and subinguinal region. There was mild erythema and tenderness over the swelling, it was fluctuant. Examination of his right hip demonstrated a slight limitation in ROM (Range of motion) due to pain. Examination of his right knee was unremarkable. His right lower distal pulses were well felt. No portal of wound entry was found on examination of his lower limbs. His blood tests showed raised inflammatory markers (C-Reactive protein- 14.2 mg/L, ESR- 90 mm/hr), with a white cell count of 22,400/cubic mm with a neutrophil count of 80%. The urea level, electrolytes and liver function tests of the patient were normal. Viral markers were negative. Fine Needle Aspiration Cytology (FNAC) was suggestive of tuberculous lesion. X-ray chest revealed hazy radio opacity in lower zone of right lung with blunting of right Cerebellopontine Angle (CPA), X-ray spine revealed no abnormalities. Ultrasound of abdomen and pelvis showed collection of debris in right paracolic region extending to lower abdomen and right upper thigh, granulomatous in nature. CECT scan of pelvis (done on second day of admission) was suggestive of large right side iliopsoas, gluteal, pelvic muscle wall and upper thigh abscess possibly of tubercular aetiology [Table/Fig-1,2 and 3]. The patient was provisionally diagnosed to be having iliopsoas abscess with extension to right gluteal region which was of tubercular origin with secondary infection. He was planned for surgery following which incision and drainage (I/D) was done under anaesthesia, on the fourth day of admission. Approximately, 2 L of purulent fluid was drained out and sent for culture and sensitivity study. The patient was treated postoperatively with antibiotics (Injection Piperacillin-tazobactum given intravenously) and other supportive measures. He was started empirically with Antitubercular Therapy (ATT) (Isoniazid, Rifampicin, Ethambutol, Pyrazinamide) the very next day i.e., the fifth day. Culture showed presence of mycobacterial and staphylococcal infection, sensitive to Meropenem, Piperacillin-Tazobactam, Vancomycin. He was discharged five days later with appropriate advice, wound dressing and to continue ATT (for two months-intensive phase, four months- continuation phase) and antibiotics (for five days).
Axial view of Contrast-Enhanced Computed Tomography: Lesion seems abutting adjoining bowel, Urinary Bladder wall and iliopubic bone without intraluminal extention or osseous destruction.
Coronal view of CECT: Long segment iliopsoas abscess.
Sagital view of CECT: Hypoattenuating lesion/walled off collection showing mild marginal enhancement appreciated in right iliopsoas muscle extending to anteromedial aspect of thigh.
The patient presented again with a swelling in the right side of the chest wall after two and half months of previous discharge. The swelling was about 6×5 cm, soft in consistency, non-tender and fluctuant. On aspiration, purulent discharge was found. So, it was diagnosed as an abscess and was operated with I/D. The drained fluid was sent for culture and sensitivity study and Cartridge Based Nucleic Acid Amplification Test (CB NAAT). The test revealed the presence of Mycobacterium tuberculosis. The patient was diagnosed as case of multidrug-resistant extrapulmonary tuberculosis as he was already on conventional ATT. He was referred with proper supportive treatment (antibiotics, anti-inflammatory agents, multivitamins) to the Drug Resistant- TB centre, SCB Medical College, Cuttack for conventional MDR regimen.
Discussion
A psoas (or iliopsoas) abscess is an accumulation of pus in the region of iliopsoas muscle compartment [1]. It may arise by the haematogenous route from a distant site (primary abscess) or via contiguous spread from adjacent structures (secondary abscess). Risk factors are diabetes, intravenous drug use, Human Immunodeficiency Virus (HIV) infection, renal failure, and other forms of immunosuppression [1,2].
Psoas abscess presents with back or flank pain, fever, inguinal mass, limping, anorexia, and weight loss. Non-tuberculous bacterial infection, most commonly secondary to an intraabdominal process but at times appearing without an identifiable source, is responsible for majority of psoas abscesses but in developing countries, tuberculosis spine (Pott’s disease) is considered the most common cause of psoas abscess [3,4]. When an inguinal mass in a patient with a psoas abscess is painless, tuberculosis is a more likely cause than a bacterial infection [5]. However, occurrence of psoas abscesses as primary presentation of tuberculosis (as in present case), with an apparent active infective focus in the lungs, has seldom been documented.
Many cases of primary psoas abscess in the past, have presented with good general health but with subacute or chronic symptoms [6]. In this particular case, the patient had symptoms of low-grade fever and pain in the right side of abdomen and corresponding thigh, the features of inflammation were also misleading. These unusual clinical features may also lead to delay in diagnosis. In the index patient, the mentioned investigations led to the diagnosis, which was later confirmed by microbiological and histopathological reports of the drained pus. It was diagnosed as primary tubercular psoas abscess with an apparent source in the lungs with secondary bacterial infection. Tubercular psoas abscesses are usually treated with ultrasound guided Percutaneous Drainage (PCD) and appropriate ATT [7]; however, some patients may require surgery as in our case. According to Vaz AP et al., a patient presented with primary tubercular psoas abcess and responded well to ATT [8] but the present patient did not responded well to ATT (on Rifampicin, Isoniazid, Ethambutol and Pyrazinamide), as he presented again with a chest abscess suggesting multidrug resistant tuberculosis. Diagnosis of primary psoas abscess needs high clinical suspicion. Furthermore, other sources of infection in lungs, spine, hip, genitourinary or gastrointestinal tract must be ruled out [9].
Conclusion(s)
To conclude, tuberculosis is still common in our country, with rising prevalence of multidrug resistant cases and can present with atypical features, as with current case study. Timely diagnosis and intervention can cure the patient and improve the quality of life.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 08, 2020
Manual Googling: Aug 26, 2020
iThenticate Software: Dec 11, 2020 (6%)
[1]. Mallick IH, Thoufeeq MH, Rajendran TP, Iliopsoas abscessesPostgrad Med J 2004 80:45910.1136/pgmj.2003.01766515299155 [Google Scholar] [CrossRef] [PubMed]
[2]. Mückley T, Schütz T, Kirschner M, Potulski M, Hofmann G, Bühren V, Psoas abscess: the spine as a primary source of infectionSpine (Phila Pa 1976) 2003 28:E10610.1097/01.BRS.0000050402.11769.0912642773 [Google Scholar] [CrossRef] [PubMed]
[3]. Roy S, Cold abscess in caries spineJ Ind Med Ass 1969 53:240-44. [Google Scholar]
[4]. Stefanich RJ, Moskowitz A, Hip flexion deformity secondary to acute pyogenic psoas abscessOrthop Rev 1987 16:67 [Google Scholar]
[5]. Procaccino JA, Lavery IC, Fazio VW, Oakley JR, Psoas abscess; difficulties encounteredDis Colon Rectum 1991 34:784-89.10.1007/BF020510711914744 [Google Scholar] [CrossRef] [PubMed]
[6]. Kiran C, Annet D’S, Shyamsunder BN, Chiranjay M, Primary tubercular psoas abscess: a rare presentationJ Infect Dev Ctries 2012 6(1):86-88.10.3855/jidc.2070 [Google Scholar] [CrossRef]
[7]. Gupta S, Suri S, Gulati M, Singh P, Ilio-psoas abscesses: Percutaneous drainage under image guidanceClin Radiol 1997 52:704-07.10.1016/S0009-9260(97)80036-0 [Google Scholar] [CrossRef]
[8]. Vaz AP, Gomes J, Esteves J, Carvalho A, Duarte R, A rare cause lower abdominal and pelvic mass, primary tuberculous psoas abscess: a case reportCases J 2009 2:18210.1186/1757-1626-2-18219946492 [Google Scholar] [CrossRef] [PubMed]
[9]. Yoo JH, Kim EH, Song HS, A case of primary psoas abscess presenting as buttock abscessJ Orthopaed Traumatol 2009 10:207-10.10.1007/s10195-009-0074-219936884 [Google Scholar] [CrossRef] [PubMed]