The practice of day care or office-based surgery is expected to grow more rapidly even in limited resources countries because of comparatively lesser costs of surgical care in these settings than hospital based or free-standing ambulatory surgery centres [1,2]. However, such surgical procedures require a well-planned meticulous anaesthesia technique.
The techniques used for day care anaesthesia should be effective, safe with little or no side effects, stable haemodynamics and should allow rapid return of the patient to preoperative status. Rapid emergence from anaesthesia with postoperative recovery of cognitive function is utmost requirements of such techniques [3]. With the availability of rapid, short acting anaesthetic, analgesic, sympatholytic and muscle relaxant drugs, as well as improved monitoring devices, it is now possible to minimise the adverse effects of anaesthesia on the recovery process [4].
Cognition can be defined as the mental activities involved in acquiring and processing information, that is, the mental processes required for everyday living. Postoperative cognitive impairment is a condition characterised by impairment of memory and concentration. It is usually responsible for longer stay in hospital during postoperative period.
The choice of anaesthetic drugs definitely affects postoperative cognition because the residual levels of anaesthetics can produce changes in central nervous system activity. Both propofol and sevoflurane are near ideal anaesthetic agents for day care surgery as they meet the day care anaesthetic criteria (most benefit with least residual side-effects) [5-8].
Sevoflurane has shown early immediate recovery as compared to propofol based anaesthesia [9-11]. But the concept of day-care anaesthesia is beyond just early recover, the cognitive or psychomotor recovery is an important but less studied parameter. Present study was planned to compare psychomotor recovery profile (primary objective) and general (secondary objective) of both intravenous propofol as well as inhaled sevoflurane for day care surgeries using a set of sensitive psychological tests of cognitive dysfunction.
Materials and Methods
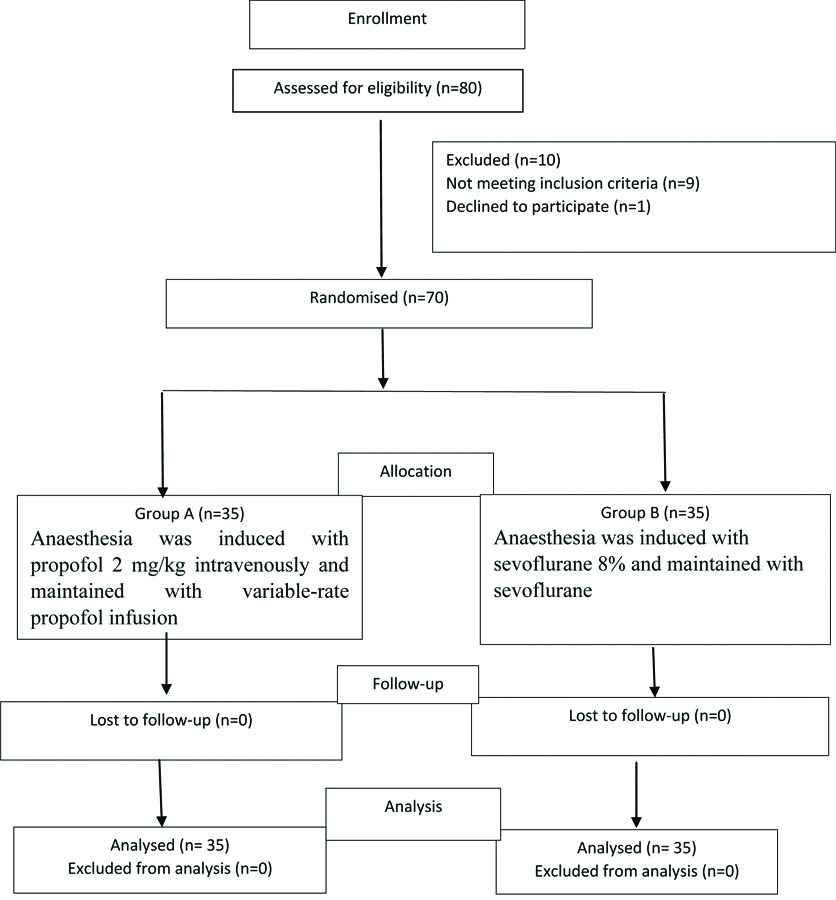
A randomised clinical trial was conducted at GGS Medical College and Hospital, Faridkot, Punjab after approval by Institutional Ethical Committee and was registered with the Clinical Trials Registry India (CTRI NO: CTRI/2018/07/014794). A sample size of 35 patients in each group was calculated and required to provide 80% power (β=0.2) to detect a significant difference in recovery profile [12] taking α error as 0.05.
Inclusion and Exclusion criteria: A total of 70 American society of Anaesthesiologists (ASA) Grade I and II patient’s aged between 18-60 years, scheduled to undergo various elective day care surgical procedures under general anaesthesia were enrolled in the study after taking patients written informed consent. Patients with known allergy to study drugs, pregnant and lactating women, patients with a history of underlying psychological disorder, drug or alcohol abuse were excluded from the study.
Patients were explained about the technique, procedure and were familiarised with the recovery and psychomotor tests to be performed in postoperative period. Patients were randomly allocated into either of 2 study groups of 35 patients each using computer generated randomisation. There were no dropouts from the study [Table/Fig-1].
In the operation room, standard ASA monitoring devices consisting of a noninvasive blood pressure cuff, pulse oximeter probe, and electrocardiogram was placed. An intravenous line was secured with 18-gauge cannula and infusion of crystalloid solution was started.
The pre-induction Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Mean Arterial Pressure (MAP), Oxygen saturation (SPO2) and Heart Rate (HR) were recorded for all patients using monitor. Patients received pentazocine 0.5 mg/kg intravenous (IV) 2 minutes prior to induction of anaesthesia. All patients were preoxygenated for 3 minutes with 100% oxygen with flow rate 8 L/min.
In group A (n=35) anaesthesia was induced with propofol 2 mg/kg intravenously. Anaesthesia was maintained with variable-rate propofol infusion (75-150 μg/kg/min, intravenously) in combination with N2O 67% in oxygen. In group B (n=35) anaesthesia was induced with sevoflurane 8% and N2O 67% in oxygen (at 6 l/min) and maintained with sevoflurane 1-2% and N2O 67% in oxygen (at 3 l/min).
Airway was maintained with Laryngeal Mask Airway (LMA) and patients were maintained on intermittent positive pressure ventilation with target End-tidal CO2 (ETCO2) of 35-40 mmHg. Intraoperatively patients were monitored for SBP, DBP, MAP, SPO2, HR and ETCO2 every 5 minutes till 30 minutes, then every 10 minutes till the end of surgery. Maintenance anaesthetics were discontinued at the end of surgery (up to dressing) and LMA was removed on adequate recovery. Intraoperative time intervals recorded includes total anaesthesia time (from induction of anaesthesia to discontinuation of N2O), total surgery time (from incision to placement of the dressing) and time taken to remove LMA.
At the time of recovery, patients were assessed for recovery parameters. Emergence time was taken from switching-off anaesthetic agent to opening of eyes. Response to commands was taken from switching-off anaesthetic agent to following verbal commands. Orientation time was taken as switching-off anaesthetic agent to orientation i.e., stating his name and present location.
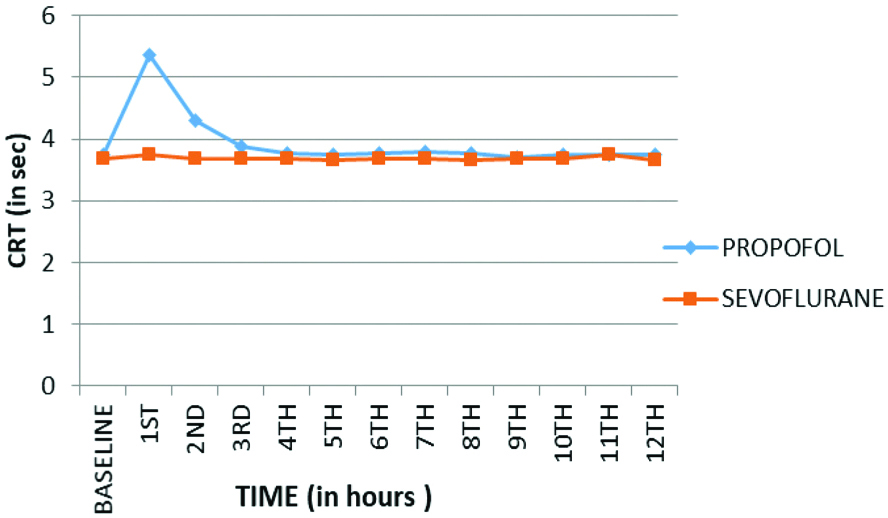
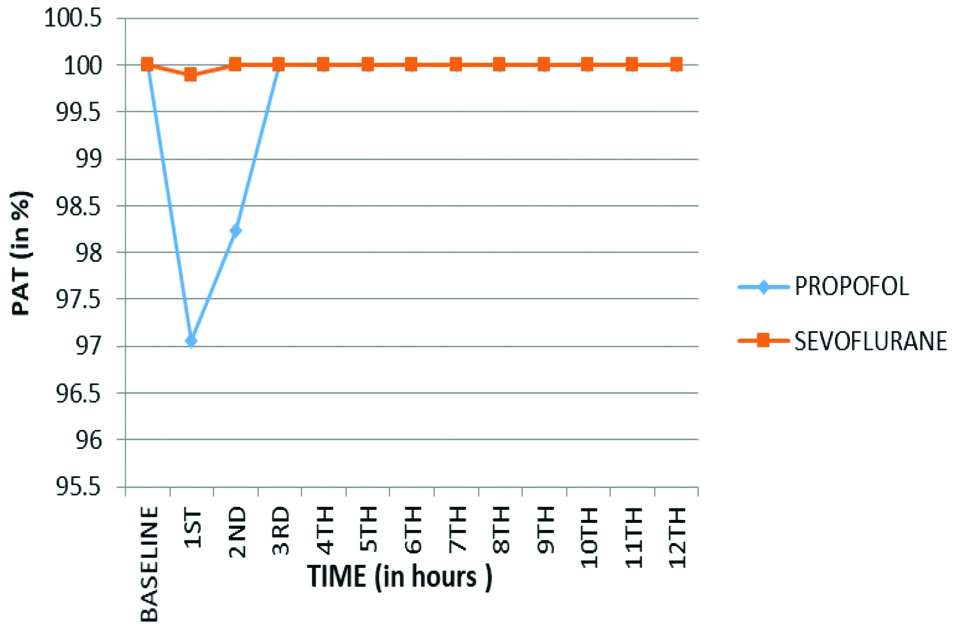
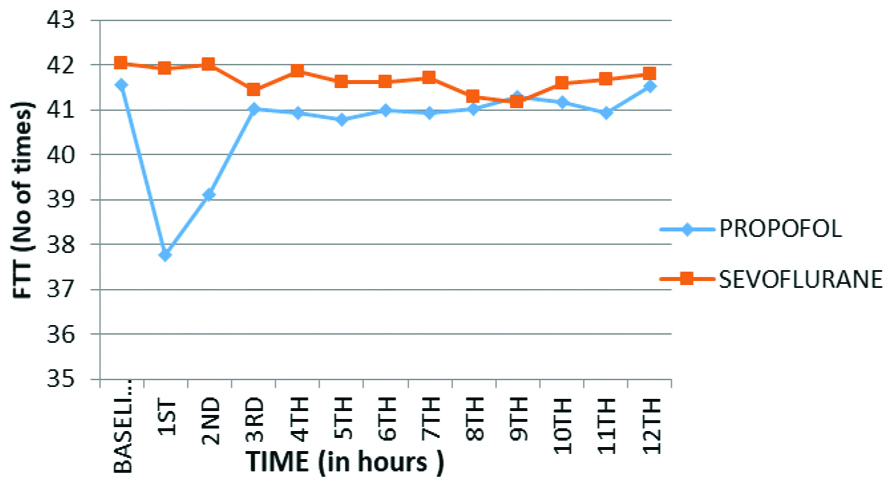
Psychomotor assessment was done preoperatively to get the baseline and assessment was done postoperatively hourly till 12th hour and compared with their baseline and also between the two groups hourly. The test employed in the study was Choice Reaction Time (CRT), Perceptive Accuracy Test (PAT), Finger Tapping Test (FTT), Peg Board Test (PBT), Card test and Trieger Dot Test (TDT). These tests have been used similarly hitherto [13].
In CRT, four different coloured bulbs with corresponding coloured switches were fixed on a wooden board. After switching on a coloured light, patient was asked to switch off the light by using the corresponding coloured switch. The median time of 20 stimuli were taken as the CRT.
In PAT, patients were asked to tell the two or three digits numbers displayed on a calculator. The number of correct answers in a period of two minutes was recorded.
In FTT, patients were asked to tap on the keyboard of the calculator. The number of times the patient taps on the keyboard in 30 seconds was taken as the finger tap score.
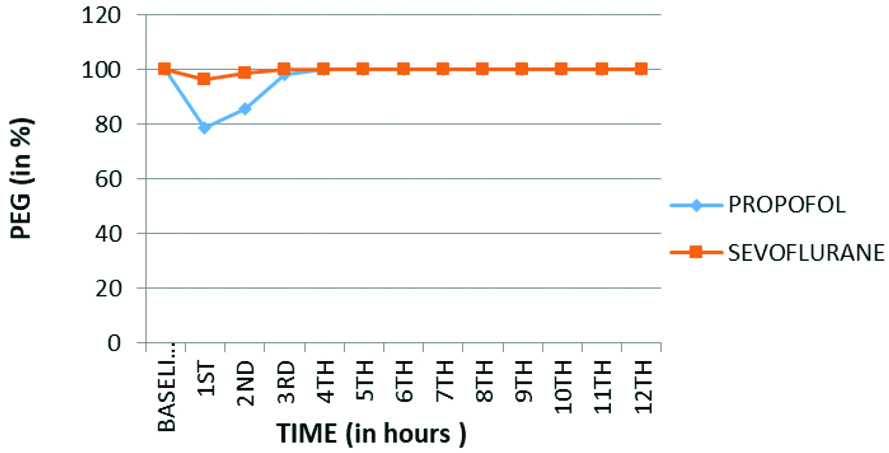
During PBT, a board with the space to fix the pegs was taken. Patients were asked to fix the entire peg in their correct places. The percentage of correct performances to fix the pegs was recorded.
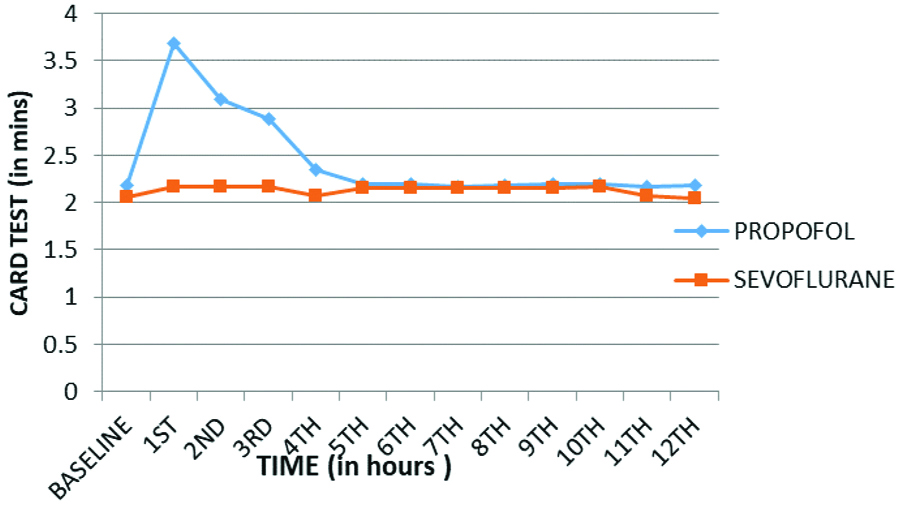
In Comparison of Card Sorting Test (CST), a set (i.e., 52) of playing cards were taken. Patients were asked to separate red and black cards into two bundles. The time taken to separate the total cards was recorded.
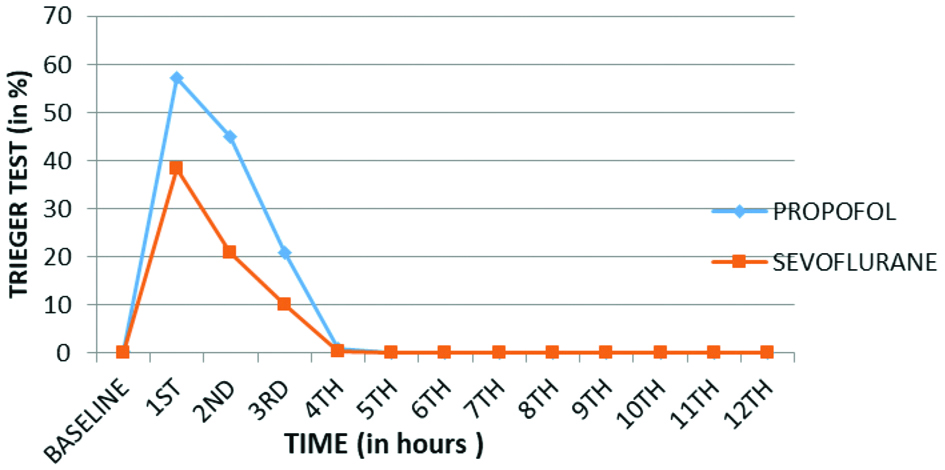
During TDT, a map of flower with 90 dots was given to each patient. Patients were asked to unite the dots and draw the map. The percentage of missing dots out of total dots was recorded.
Statistical Analysis
Data were collected, tabulated, coded in MS excel and then analysed using SPSS, computer software version 16. Continuous variables were presented as mean and Standard Deviation (SD) while categorical variables were presented as percent. As regard continuous variables; unpaired student’s t-test was used. Chi-square test was used to find out association between two categorical variables. p-value was considered as significant if <0.05 and highly significant if <0.001.
Results
In the present study both the groups were comparable in terms of age, weight, gender, ASA status, duration of surgery and duration of anaesthesia (p>0.05) [Table/Fig-2].
The demographic data, anaesthesia and surgery duration.
| Variables | Group A Mean±SD (n=35) | Group B Mean±SD (n=35) | p-value |
|---|
| Age in years | 48.14±9.65 | 46.29±9.14 | 0.411* |
| Weight in kg | 60.54±5.56 | 59.31±4.89 | 0.330* |
| ASA (I/II) | 19/16 | 18/17 | 0.811# |
| Gender (Male/Female) | 17/18 | 18/17 | 0.811# |
| Anaesthesia duration in minutes | 75.40±22.92 | 72.74±23.50 | 0.634* |
| Surgery duration in minutes | 71.77±22.55 | 67.57±23.65 | 0.450* |
Test used- *Student t-test; #-Chi-square test
Primary outcome was psychomotor recovery. Psychomotor assessment of patients was done in recovery period using six special tests which suggested that psychomotor recovery is faster with sevoflurane as compared to propofol. The baseline values for CRT, PAT, FTT, PBT [Table/Fig-3,4,5 and 6] were achieved almost in the 2nd hour of recovery in patients anaesthetised with sevoflurane and in 4th hour in patients anaesthetised using propofol (p<0.001). In CST the baseline values were achieved at 4th hour in sevoflurane group as compared to 5th hour in propofol group (p<0.001) [Table/Fig-7]. In TDT the baseline values were achieved by 5th hour, both in group B and group A (p<0.001) [Table/Fig-8]. Hence, the psychomotor recovery was attained by almost second hour in sevoflurane group and by fourth hour in propofol group.
Comparison of Choice Reaction Time (CRT) between two groups.
Comparison of Perceptive Accuracy Test (PAT) between two groups.
Comparison of Finger Tapping Test (FTT) between two groups.
Comparison of Peg Board Test (PBT) between two group.
Comparison of Card Sorting Test (CST) between two groups.
Comparison of Trieger Dot Test (TDT) between two groups.
Secondary outcome was general recovery. A statistically high significant difference (p<0.001) in terms of General (emergence, responds to commands, orientation, time taken to remove LMA) amongst the two groups was noted [Table/Fig-9]. General recovery was significantly earlier in sevoflurane group (group B) as compared to propofol group (group A). Adverse effects between groups were also comparable [Table/Fig-10].
Recovery characteristics between the two groups.
| Variables | Group A Mean±SD (n=35) | Group B Mean±SD (n=35) | Unpaired t-test p-value |
|---|
| Time taken to remove LMA in minutes | 8.65±2.40 | 5.30±1.23 | <0.001 |
| Emergence time in minutes | 8.87±2.42 | 5.83±1.23 | <0.001 |
| Time to respond to commands in minutes | 10.01±2.52 | 6.81±1.39 | <0.001 |
| Time to orientation in minutes | 10.76±2.61 | 7.15±1.53 | <0.001 |
p-value <0.001-highly significant
Comparison adverse effects between groups.
| Adverse effects | Group A (n=35) | Group B (n=35) | Chi-square test p-value |
|---|
| Number | % | Number | % |
|---|
| Nil | 34 | 97.1 | 31 | 88.6 | 2.472Df=2p=0.291 |
| Nausea | 1 | 2.9 | 2 | 5.7 |
| Vomiting | 0 | 0 | 2 | 5.7 |
| Total | 35 | 100 | 35 | 100 |
Discussion
In the present study, comparing propofol and sevoflurane in day care surgery for recovery characteristics, it was found that Sevoflurane provides a much rapid return of psychomotor and cognitive ability as compared to propofol.
The findings of the present study correlate with the research done by Tilvawala KR and Panchotiya PR, that compared propofol infusion and sevoflurane as the sole maintenance agent in laparoscopic surgery and found that when sevoflurane was used for general anaesthesia, faster emergence can be obtained as compared to propofol [11]. Sevoflurane group was associated with lesser time to spontaneous respiration, eye opening, verbal commands like telling own name by patients.
Results of the present study also correlate well with another similar observation by Orhon ZN et al., who observed recovery profile of propofol and sevoflurane anaesthesia. They used Bispectral Index (BIS) for adjusting sevoflurane concentration and propofol infusion rate and concluded that when sevoflurane is used for maintenance of anaesthesia, it leads to faster recovery as compared to propofol [14].
Khare A et al., also evaluated haemodynamic changes and recovery characteristics with propofol and sevoflurane anaesthesia during laparoscopic cholecystectomies and observed that emergence time after discontinuation of the primary maintenance anaesthesia was significantly less in sevoflurane in comparison to propofol (p<0.001). General recovery to be significantly earlier in sevoflurane group as compared to propofol group [15].
Parida S et al., conducted a comparison of cognitive, ambulatory, and psychomotor recovery profiles after day care anaesthesia with propofol and sevoflurane. In their study only TDT and Digital Symbol Substitution Test (DSST) were used. They observed that recovery especially with regards to cognitive functions was slightly faster in sevoflurane group than propofol group [16]. To increase the sensitivity of psychomotor recovery characteristics, Authors added four more (CRT, PAT, FTT, PEG) above mentioned tests for psychomotor evaluation. So, results of present study very clearly suggest a significantly faster psychomotor recovery in patients when using sevoflurane as compared to propofol.
The postoperative adverse effects [Table/Fig-10] were insignificant (p=0.291) between the sevoflurane and propofol group in the present study. Similarly, in a study done by Chen PN et al., there was no significant difference between the sevoflurane and propofol groups in regards to postoperative vomiting [17].
Thus, this suggests that both propofol and sevoflurane are good day care agents. Sevoflurane provides a much rapid return of psychomotor and cognitive ability as compared to propofol. Sevoflurane is an inhalational agent with Minimum Alveolar Concentration (MAC) of 1.8 and low blood-gas partition co-efficient of 0.69 [7]. A low blood-gas partition coefficient is theoretically associated with rapid induction of anaesthesia and rapid emergence from anaesthesia. Propofol is highly lipophilic and has relatively short context sensitivity half-time. However, some amount of propofol remains present in the less well perfused compartments of the body. Though return of propofol from these compartments generally contributes little to the concentration of drug in the central compartment but when it is compared to another “rapid-offset” drug such as sevoflurane, this amount of residual drug might result in greater sedation which might be the reason for comparatively delayed psychomotor recovery that was observed in our study.
Limitation(s)
Major limitations of this study were that the consciousness-level monitor, such as entropy or BIS, were not used for the study. Facilities were not available for monitoring real time blood levels of the anaesthetic agents. It would be difficult to prove the same anaesthetic depth in both the groups without the above; however, patients in both the groups recovered without any explicit memory. In addition, anaesthesia was provided by experienced anaesthetists according to accepted standards of care.
Conclusion(s)
Both sevoflurane and propofol are useful agents for day care surgery. Sevoflurane provides a much rapid return of psychomotor and cognitive ability as compared to propofol. A sevoflurane based anaesthesia technique may be advantageous over a propofol based technique where lesser depression of cognitive abilities is desired.
Test used- *Student t-test; #-Chi-square test
p-value <0.001-highly significant