Introduction
The most frequent severe manifestation of COVID-19 is pneumonia manifesting with fever, cough, myalgia, dyspnoea and bilateral consolidations on chest radiograph. However, gastrointestinal symptoms [1,2] due to an inflammatory process [3] caused by the action of coronavirus on its target angiotensin converting enzyme-2 expressed abundantly in the lung, small bowel and vasculature [4] have also been reported.
Case Series
Present case series analysis has been approved by the Institute’s Ethical Committee (MC/EC/2020 NO.433). Data base records of the COVID-19 wards, surgical wards and Radiology Department from March 22 to May 3 2020 were searched and patients who stayed in COVID ward and those requiring a surgical consult during their hospital stay were included for analysis. Patients with co-morbid medical conditions like cardiac compromise, hypertension, diabetes mellitus, chest pathologies (asthma, bronchiectasis, interstitial lung disease) or acquired immunodeficiency syndrome were excluded. A total of 11 cases were identified and their clinical and radiological records were studied separately and concluded consensually by two surgeons. A brief account of all the cases is being included here to increase prudence among all healthcare workers.
Case 1
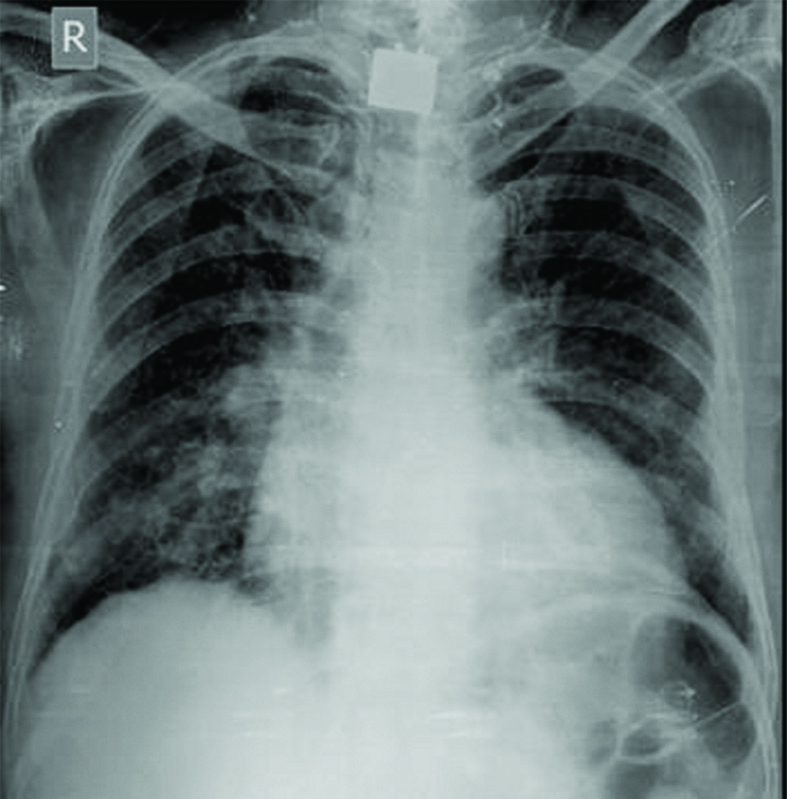
A 22-year-old man presented with acute abdominal pain and constipation since two days. On examination, he was found to be in shock with signs of peritonitis. His blood investigations showed deranged parameters along with a positive COVID-19 Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR). Erect abdominal radiograph showed gas under diaphragm with otherwise clear lung fields [Table/Fig-1a]. Patient underwent exploratory laparotomy and an ileal perforation (2×1 cm), 30 cm from ileocaecal junction was found. The perforated segment was brought out as loop ileostomy. Postoperatively, patient had progressive respiratory distress with appearance of bilateral peripheral opacities in chest radiograph [Table/Fig-1b]. He was reintubated but succumbed to his illness on second postoperative day.
a) X-ray abdomen- erect view showing air under diaphragm (Pneumoperitoneum) and clear visualised lung fields. b) Chest X-Ray Antero Posterior (CXR AP) view taken 2nd postoperative day showing bilateral peripheral multifocal consolidations consistent with typical COVID pattern.
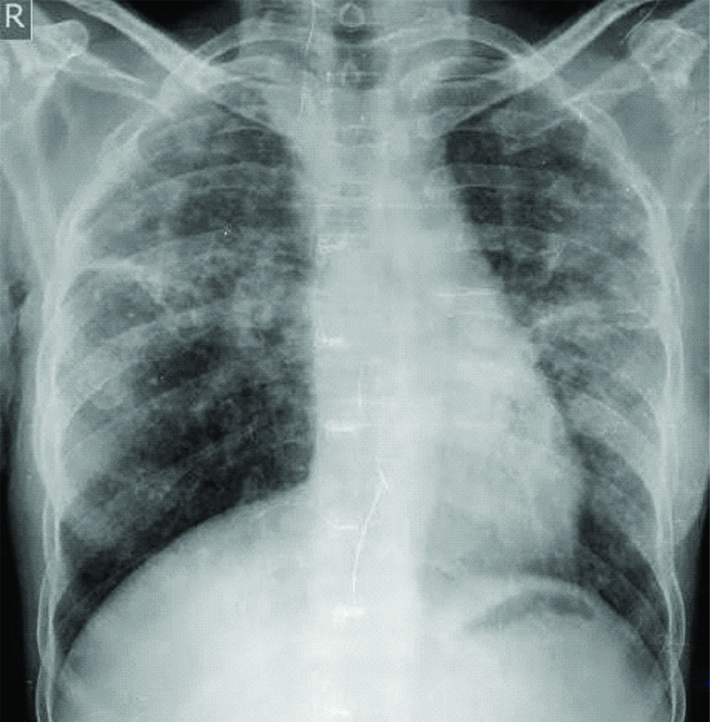
Chest X-Ray Antero Posterior (CXR AP) view showing predominantly peripheral multifocal consolidations consistent with typical COVID pattern.

Unfortunately, two of the surgery consultants along with one resident involved in this case tested positive, four days post-surgery. They were hospitalised till they tested negative twice and were discharged with instructions of self-isolation for another 14 days. All three of them remained asymptomatic throughout their illness.
Case 2
A 42-year-old man presented with a Fournier’s Gangrene since four days. Considering the septic condition, patient was subjected to immediate extensive debridement using all precautionary measures. Postoperatively, patient was discovered as being COVID-19 positive. He was shifted to isolation ward and antibiotics were continued and patient responded fairly well to treatment. He was discharged after 16 days on testing twice negative for COVID RT-PCR. The healthcare team involved though tested twice negative, was quarantined for 14 days.
Case 3
A 60-year-old man presented with abdominal distension and constipation since three days. On examination, patient shows the sign of jaundice, dehydrated having laboured breathing. Abdomen was distended, with positive shifting dullness and faecoliths on per rectal examination. He had a Contrast Enhanced Computed Tomography (CECT) abdomen report with him showing an 8×7 cm size Hepatocellular carcinoma in right lobe of liver along with ascites. Other investigations included chest radiograph showing bilateral, multifocal, peripheral air space opacities [Table/Fig-2] and deranged blood investigations and a positive COVID-19 test. He was taken to COVID Intensive Care Unit (ICU) where he died within 24 hours of admission. Healthcare team involved in Emergency Management was quarantined although none of them tested positive.
Contrast-Enhanced Computed Tomography (CECT) axial images showing dilated, inflamed appendix (solid white arrow in 3a) with periappendiceal fat stranding and appendicular abscess formation (white arrows in 3b).
Case 4
A 36-year-old lady presented to COVID-19 Outpatient Department (OPD) with pain in Right Iliac Fossa (RIF), and fever since 12 days. She was referred from a private hospital with a positive COVID-19 test. Her seven-day-old blood reports and 10-day-old CECT abdomen suggested acute appendicitis [Table/Fig-3a,b]. On call surgery consultant found tenderness (no rebound) in RIF, a 1×2 cm lump in RIF and rest of the abdomen nontender and nondistended with improved blood reports on day of admission with a raised Lactate Dehydrogenase (LDH) (1027 U/L). Diagnosis of resolving appendicitis with a small appendicular lump was made and patient was put on conservative management. She responded well, became afebrile and regained appetite. Patient was started on clear liquids and was discharged after 14 days on semisolid diet after double negative COVID-19 test.
Case 5
A 75-year-old man presented to COVID-19 Outpatient Department with complains of continuous fever and mild dyspnoea since 2 days. He had a COVID-19 positive report from a private hospital, so he was admitted in COVID-19 ward. His blood reports showed deranged C-Reactive Protein (CRP), Ferritin, Total Leucocyte Count (TLC), Fibrin Degradation Products (FDP), Activated Partial Thromboplastin Time (APTT), International Normalised Ratio (INR), Prothrombin Time (PT) and LDH. CT thorax showed no significant chest finding but left pyelonephritis with renal abscess was seen [Table/Fig-4]. Higher antibiotics with ultrasound guided aspiration were advised by surgeon. Patient showed marked improvement and became afebrile within four days. He remained admitted for nine days in isolation due to his COVID positive outside report although he never tested positive at study institute.
Axial Non-Contrast Computerised Tomography (NCCT) images showing enlarged left kidney with perinephric fat stranding and rounded low attenuation area in lateral interpolar cortex measuring 3.5×3.5 cm suggestive of changes of pyelonephritis with renal abscess (white thick arrow).
Case 6
A 42-year-old man presented with progressive cough with expectoration, dyspnoea, right sided chest and upper abdominal pain and fever since 2 days. Patient was suspected as having COVID-19 infection and was admitted in isolation ward. His blood investigations showing deranged APTT, PT, INR, TLC, FDP, D-dimer and LDH, further raised the suspicion of COVID. However, loculated right pleural effusion in chest X-ray and a negative COVID RT-PCR pointed against it. Patient was subjected to CT thorax which revealed segment seven liver abscess rupturing into right pleural space causing empyema [Table/Fig-5a,b]. On surgical consultation, an intercostal chest drain and ultrasound guided pigtail in the abscess cavity was advised and placed with antibiotic coverage. Repeat COVID-19 test was also negative. Patient recovered and was discharged after 12 days.
Axial and Coronal Contrast-Enhanced Computed Tomography (CECT) scan showing peripherally enhancing multiloculated low attenuating lesion with shaggy walls and perilesional low attenuation in segment 7 of liver (blue star) extending in perihepatic space (a) as well as right pleural space (white arrow in b) suggestive of ruptured liver abscess with right sided empyema.
Case 7
A 23-year-old man presented with severe pain in RIF, vomiting and constipation since one day. He showed rebound tenderness and guarding in RIF along with mild distension and tenderness all over the abdomen. Ultrasonography reported acute appendicitis with periappendiceal and pelvic abscess. Blood reports showed raised TLC, Blood Urea (BU) and Serum Creatinine (SCr) while chest radiograph had mild pneumonitis changes [Table/Fig-6]. Due to his grave clinical condition and a clear diagnosis on sonography in consensus with clinical findings, he was immediately explored. A completely gangrenous appendix and caecum with pregangrenous changes and gangrenous patches extending from 10 cm of distal ileum till half of the ascending colon were found. The pathological part was resected. Patient underwent COVID-19 RT-PCR postoperatively and it came out positive. Patient was shifted to COVID-19 ward where he showed progressive deterioration clinically, in laboratory parameters and in chest radiograph (bilateral white out lungs). He died of his illness on fourth postoperative day in ICU.
Chest X-Ray Posteroanterior (CXR PA) view showing mild bilateral peripheral air space opacities raising suspicion of early COVID pneumonia changes.
Case 8
A 75-year-old male presented with features of acute intestinal obstruction. CECT abdomen showed ileal stricture with proximal dilated edematous bowel. Patient tested COVID negative. On exploration, there was approximately 15 cm long perforated gangrenous segment about 20 cm proximal to ileocaecal junction with pregangrenous changes in rest of ileum. The gangrenous segment was resected and double barrel stoma taken out. Postoperatively, patient showed darkening of stoma colour. On third postoperative day, chest radiograph showed bilateral florid pneumonitis [Table/Fig-7]. COVID-19 test was repeated which came positive. Patient was immediately shifted to COVID-19 ICU. Due to rapid clinical deterioration, he could not survive. Whole of the treating team had to be quarantined although nobody tested positive.
Chest X-Ray Posteroanterior (CXR PA) view showing bilateral peripheral diffuse air space opacities consistent with COVID pneumonia typical pattern- Acute respiratory distress syndrome (ARDS).
Case 9, 10 and 11
Case 9 was a nondiabetic 38-year-old female, presented with acute pain abdomen with raised TLC and positive COVID-19 test. She was shifted to COVID ward and later diagnosed as having acute calculous cholecystitis on sonography. She settled on antibiotics and analgesics within 48 hours and was discharged after eight days after a negative COVID-19 report.
Case 10 was a 19-year-old boy who presented with acute right inguinal pain and swelling post-trauma one day back. He tested positive for COVID-19. Sonography of right inguinal region showed a hypervascular undescended testis showing features of orchitis along with inguinal hernia. He was also managed with analgesics and antibiotics and was discharged with instructions of surgery at a later date.
Case 11 was a 45-year-old man who presented with an irreducible right inguinal hernia and positive COVID report. In isolation ward, after giving analgesics and foot end elevation of bed, reduction of hernia was attempted and easily achieved. Patient was advised scrotal support along with treatment for his ongoing constipation and a hernioplasty at a later date post-lockdown.
Discussion
Abnormalities in chest imaging have been reported up to 54% of completely asymptomatic, COVID-19 test positive patients [2]. Such atypical patients can be easily missed in screening measures and hence, would not get timely isolation leading to unexpected spread of COVID-19 infection [5].
The eleven cases shared, demonstrate seven unique scenarios in which a surgeon may encounter a COVID-19 patient in field. Due to the absence of specific treatment or vaccine, it is arduous to ‘flatten the curve’ of this pandemic if timely recognition and isolation of positive patients is not done [3].
In first scenario, COVID-19 patient presents with a concurrent surgical pathology [6].
This was seen in case 1, 2 and 4. Case 4 was an already diagnosed case and cases 1 and 2 were diagnosed during the course of their treatment. Case 1 was young man with an established abdominal pathology and clear lung fields in preoperative period whose disease process flared up rapidly in postoperative period with appearance of peripheral basal opacities in chest radiograph [Table/Fig-1b], causing progressive respiratory distress and death. On the other hand, case 4, (acute appendicitis) who was managed conservatively had a favourable course and settled predictably on antibiotics. Literature has reports wherein, appendicitis patient, even without a lump formation have been successfully managed on antibiotics with vigilant monitoring during this pandemic [7,8]. Cases 2, 5 and 6 who were subjected to less invasive interventions also had a favourable outcome.
Case 1 wherein three of our doctors got infected with COVID-19 further highlights the importance of an institutional protocol for all surgical patients during this pandemic to prevent its transmission [9]. This being the first case of COVID-19 in our department, Authors were unarmed in terms of such a protocol, though the treating doctors were equipped with highest level of Personal Protection Equipment (PPE) (Level A) during surgery and were fully aware of Donning and Doffing methods.
In the second scenario, a COVID-19 positive patient may incidentally be diagnosed with an additional surgical pathology [6].
This was seen in case 5 where a COVID-19 positive patient being treated for fever and chest complaints were incidentally diagnosed with renal abscess. On aspirating the abscess and giving specific antibiotics, patient recovered very well. Thus, the bias in our mind due to positive COVID-19 test should not prevent us from diagnosing an additional surgical pathology and should not deprive our patient of the required treatment.
Third scenario is when a purely surgical patient has symptomatology closely mimicking that of a COVID-19 patient.
This was seen in case 6, with patient having chest complaints due to ruptured liver abscess in the chest and not due to COVID-19. Thus, we should not miss a true surgical pathology in patients mimicking COVID-19 clinically and not actually COVID positive.
Fourth scenario can be when a patient contracts COVID after hospitalisation indicating a possible nosocomial infection [6].
Case 8 typically exemplifies this scenario. Patient tested negative on the day of admission but postoperatively after five days of hospital stay he became symptomatic for COVID-19 and also tested positive for it. Case 3 having HCC, though may have been COVID-19 positive at time of admission, is being discussed under this scenario to highlight a specifically immunocompromised cohort susceptible to such nosocomial infections. Patients with a past history of cancer or recent chemotherapy have been reported to contract COVID-19 and develop severer forms of the disease [10] so extra caution and precaution is needed while dealing with them.
Fifth scenario is a false negative COVID RT-PCR.
First negative COVID-19 test on day of admission in case 8 may have been actually false negative which is a common possibility as already mentioned in literature [11]. This further adds to the importance of a standardised protocol for all patients (COVID-19 and non COVID-19) for everyone’s safety [9].
In Sixth scenario, COVID-19 may be suspected by intraoperative unusual intestinal findings.
This was seen in case 7. Intestinal findings in the form of gangrenous patches, yellowish discoloration, infarction (dead bowel) probably due thrombi in mesenteric vessels in COVID-19 patients have been reported in literature [12]. Similar findings were noted in case 7. Point to note here is that due to the strict adherence to Institutional Preventive Protocol [11] by the whole team of doctors and staff in all cases (COVID-19 and non COVID-19), none of our heathcare workers tested positive for COVID-19 except in case 1. Thus, all patients must be treated as positive until proven otherwise to safeguard all [3].
Lastly, COVID-19 patients requiring an elective surgical procedure were also encounterd as in cases 9, 10 and 11 of the present series. Surgeries of such patients were strictly deferred during lockdown at our institute with an advice to get operated once this pandemic is over. In available literature, the most common cause of mortality in COVID-19 operated patients was Acute Respiratory Distress syndrome (ARDS) with mortality being much higher than expected even for elective surgery [13,14]. Operation theatres carry the highest risk of transmission through respiratory as well as gastrointestinal secretions in which corona virus remains viable for a longer time [15,16]. So, theatres do need a separate protocol.
Designated COVID-19 Operating Areas (COA) should be allocated closest to the entrance of the theatre block with no movement of persons, equipments, in and out of COA after taking the patient in. Level A type of PPE donned properly by whole team of health care workers involved should also be doffed appropriately in separate designated area. Adequate time should be allowed in between the cases depending upon the number of air exchanges/hour (ideal- ≥ 25 exchanges/h) [17]. A pre-defined shortest route should be designated for transfer of COVID-19 patients. Any unexpected contamination (vomiting or else) during transport, should immediately alert the sanitisation team [18]. Smoke evacuators should be acquired in COA to decrease aerosols [19]. All deferrable surgical procedures should be postponed and if undeferable, minimal staff should be involved. Masks should be compulsory for all. Healthcare workers should use N-95 masks. COVID RT-PCR should be done preoperatively for all surgical patients except for life-threatening surgical emergencies in which all universal precautions should be then taken.
Conclusion(s)
Surgeons need to modify their surgical practice during this pandemic to safeguard themselves, their families and even their patients. Prompt recognition and isolation of positive patients along with a clear institutional protocol for surgical practice can keep our system resilient and useful for the population we serve.
[1]. Inui S, Fujikawa A, Jitsu M, Kunishima N, Watanabe S, Suzuki Y, Chest CT findings in cases from the cruise ship “diamond princess” with coronavirus disease 2019 (COVID-19)Radiol Cardiothorac Imaging 2020 2(2):e20011010.1148/ryct.202020011033778566 [Google Scholar] [CrossRef] [PubMed]
[2]. Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Correlation of Chest CT and RT-PCR testing for coronavirus disease 2019 (covid-19) in China: A report of 1014 casesRadiology 2020 296(2):E32-40.10.1148/radiol.202020064232101510 [Google Scholar] [CrossRef] [PubMed]
[3]. Gahide G, Frandon J, Vendrell JF, COVID-19 patients presenting with afebrile acute abdominal painClin Med (Lond) 2020 20(3):e04-06.10.7861/clinmed.2020-015032341078 [Google Scholar] [CrossRef] [PubMed]
[4]. Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, Digestive system is a potential route of COVID-19: An analysis of single-cell co-expression pattern of key proteins in viral entry processBMJ Pub Health Emg Coll 2020 69(6):1010-18.10.1136/gutjnl-2020-3209537211082 [Google Scholar] [CrossRef] [PubMed]
[5]. Dane B, Brusca-Augello G, Kim D, Katz DS, Unexpected Findings of Coronavirus Disease (COVID-19) at the Lung Bases on Abdominopelvic CTAJR Am J Roentgenol 2020 215(3):603-06.10.2214/AJR.20.2324032319792 [Google Scholar] [CrossRef] [PubMed]
[6]. Nepogodiev D, Global guidance for surgical care during the COVID-19 pandemicBr J Surg 2020 15:10.1002/bjs.11646 [Google Scholar]
[7]. Collard M, Lakkis Z, Loriau J, Mege D, Sabbagh C, Lefevre JH, Antibiotics alone as an alternative to appendectomy for uncomplicated acute appendicitis in adults: Changes in treatment modalities related to the COVID-19 health crisisJ Visc Surg 2020 157(3S1):S33-42.10.1016/j.jviscsurg.2020.04.01432362368 [Google Scholar] [CrossRef] [PubMed]
[8]. Suwanwongse K, Shabarek N, Successful conservative management of acute appendicitis in a Coronavirus Disease 2019 (COVID-19) PatientCureus 2020 12(4):e783410.7759/cureus.7834 [Google Scholar] [CrossRef]
[9]. Forrester JD, Nassar AK, Maggio PM, Hawn MT, Precautions for operating room team members during the COVID-19 pandemicJ Am Coll Surg 2020 230(6):1098-101.10.1016/j.jamcollsurg.2020.03.03032247836 [Google Scholar] [CrossRef] [PubMed]
[10]. Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Cancer patients in SARS-CoV-2 infection: A nationwide analysis in ChinaLancet Oncol 2020 21(3):335-37.10.1016/S1470-2045(20)30096-6 [Google Scholar] [CrossRef]
[11]. Li D, Wang D, Dong J, Wang N, Huang H, Xu H, False-negative results of real-time reverse-transcriptase polymerase chain reaction for severe acute respiratory syndrome coronavirus 2: Role of deep-learning-based ct diagnosis and insights from two casesKorean J Radiol 2020 21(4):505-08.10.3348/kjr.2020.014632174053 [Google Scholar] [CrossRef] [PubMed]
[12]. Bhayana R, Som A, Li MD, Carey DE, Anderson MA, Blake MA, Abdominal imaging findings in COVID-19: Preliminary observationsRadiol 2020 297:E207-15.10.1148/radiol.202020190832391742 [Google Scholar] [CrossRef] [PubMed]
[13]. Leia S, Jiangb F, Sua W, Chend C, Chene J, Meif W, Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infectionE Clinical Medicine 2020 21:10033110.1016/j.eclinm.2020.10033132292899 [Google Scholar] [CrossRef] [PubMed]
[14]. Aminian A, Safari S, Razeghian-Jahromi A, Ghorbani M, Delaney CP, COVID-19 outbreak and surgical practice: Unexpected fatality in perioperative periodAnn Surg 2020 272(1):e27-29.10.1097/SLA.000000000000392532221117 [Google Scholar] [CrossRef] [PubMed]
[15]. Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Washington State 2019-nCoV case investigation team. First Case of 2019 Novel Coronavirus in the United StatesN Engl J Med 2020 382(10):929-36.10.1056/NEJMoa200119132004427 [Google Scholar] [CrossRef] [PubMed]
[16]. Cha MH, Regueiro M, Sandhu DS, Gastrointestinal and hepatic manifestations of COVID-19: A comprehensive reviewWorld J Gastroenterol 2020 26(19):2323-32.10.3748/wjg.v26.i19.232332476796 [Google Scholar] [CrossRef] [PubMed]
[17]. Wong J, Goh QY, Tan Z, Lie SA, Tay YC, Ng SY, Preparing for a COVID-19 pandemic: A review of operating room outbreak response measures in a large tertiary hospital in SingaporeCan J Anaesth 2020 67(6):732-45.10.1007/s12630-020-01620-932162212 [Google Scholar] [CrossRef] [PubMed]
[18]. Coccolini F, Perrone G, Chiarugi M, Di Marzo F, Ansaloni L, Scandroglio I, Surgery in COVID-19 patients: Operational directivesWorld J Emerg Surg 2020 15(25)10.1186/s13017-020-00307-232264898 [Google Scholar] [CrossRef] [PubMed]
[19]. Mowbray NG, Ansell J, Horwood J, Cornish J, Rizkallah P, Parker A, Safe management of surgical smoke in the age of COVID-19Br J Surg 2020 107(11):1406-13.10.1002/bjs.1167932363596 [Google Scholar] [CrossRef] [PubMed]