Vitiligo is an acquired disorder of pigmentation characterised by depigmented macules on any part of the skin and mucosa. It affects approximately 1% of the population worldwide [1]. Vitiligo has significant psychosocial impact on patients’ quality of life, especially in those with skin of colour [2]. Phototherapy is considered a first line treatment in the management of vitiligo [3,4]. Phototherapy modalities currently preferred for the treatment of vitiligo include NBUVB light and the 308 nm monochromatic xenon chloride excimer laser.
Both modalities are relatively new. NBUVB was first used in 1997 by Westerhof W and Nieuweboer-Krobotova L, and is now the most-commonly used phototherapy modality for vitiligo [5]. It is administered via fluorescent tubes emitting light with a wavelength of 311-312 nm which lies in the NBUVB spectrum. The treatment is available in full body chambers, as hand and foot units as well as hand-held units for home-based treatments [6]. Excimer laser was first reported for vitiligo treatment in 2002 [7]. The laser’s wavelength of 308 nm lies in the UVB spectrum of light and thus has almost similar effects on repigmentation as NBUVB [8]. It offers some advantages over NBUVB. Nonlesional skin is not treated, hence tanning of surrounding normal skin is avoided, difficult to reach sites can be targeted and the overall cumulative UVB dose is lower compared to NBUVB. However, it is time consuming and labor intensive, and does not address disease stabilisation, since clinically unaffected skin is not treated [9].
NBUVB and excimer laser are currently Food and Drug Administration (FDA) approved treatments of vitiligo. Both are administered 2-3 times a week on nonconsecutive days. In general, NBUVB is used in patients with vitiligo affecting more than 10% of Body Surface Area (BSA) and excimer laser in those with less than 10% BSA [6,9].
There are only a handful of studies comparing NBUVB and excimer laser in patients with vitiligo [10-14]. These studies were conducted with small patient numbers, hence the significance of conclusions inferred cannot be extrapolated to the general population. Larger comparative studies are required in vitiligo to assess the effectiveness of treatments. The aim of present study was to compare the efficacy and safety of NBUVB versus excimer laser in 146 patients with vitiligo attending the phototherapy unit of a tertiary care dermatology center in Dubai.
Materials and Methods
This clinical audit was a retrospective chart review. The audit was approved by the Clinical Governance Office of the Health Regulation Department of Dubai Health Authority (dated: 30 May, 2018).
Inclusion criteria: Patients aged 4-70 years with established vitiligo undergoing NBUVB and excimer laser therapy from January 2016 to August 2018 at the phototherapy unit of the Department of Dermatology, Rashid Hospital, Dubai Health Authority.
Exclusion criteria: Patients aged less than 4 years and more than 70 years.
The PHAROS EX 308 protocol was followed in the hospital for administering excimer laser [7] [Table/Fig-1a,b]. The laser was administered via a fibre optic cable directly to the vitiligo lesions by a trained nurse. Starting doses varied for different parts of the body and 10-20% increments in doses were made on subsequent visits depending on response to earlier doses.
PHAROS EX-308 protocol for excimer laser.
| (a) Vitiligo protocol: First treatment dose |
|---|
| Site | Complete depigmentation | Partial pigmentation |
|---|
| Face, neck, trunk | 100 mJ/cm2 | 150 mj/cm2 |
| Arms, legs, elbows, knees | 150 mJ/cm2 | 200 mj/cm2 |
| Hands and feet | 200 mJ/cm2 | 250 mj/cm2 |
| (b) Vitiligo protocol: Continuing treatment doses |
|---|
| Patient response to previous dose | None or minimal reaction-Slight erythema, warmth or sensitivity | Moderate reaction-Bright red erythema, some warmth or sensitivity for short time | Good reaction-Bright red erythema, the skin is very warm and sensitive | Severe reaction-Severe erythema, pain and/or blisters |
| Suggested change | Increase dose by 20% | Increase dose by 10% | Continue increasing by 10% unless patient is uncomfortable. Then maintain the dose | Reduce dose by 20% |
The NBUVB phototherapy chamber used to administer full body NBUVB (Waldmann Co., Villingen-Schwenningen, Germany) had 48 fluorescent tubes (TL-100W/01, Phillips, Eindhoven, The Netherlands) lined in its wall with peak emission at 311 to 312 nm. All patients were initiated with 70% of the standard Minimal Erythema Dose (MED) of the patient’s Fitzpatrick’s skin type [15] and 10% subsequent dose increments were made. The Vitiligo Working Group guidelines were the protocol used for NBUVB treatment in the hospital [Table/Fig-2] [4]. All patients wore safety glasses during treatment sessions and patients on NBUVB wore their underwear in the NBUVB chamber to protect the genitalia during treatment. Both treatment modalities were administered 2-3 times a week on nonconsecutive days.
NBUVB phototherapy protocol.
| Skin type | Initial dose (J/cm2) | Increase (%) | Maximum dose (J/cm2) |
|---|
| I | 0.03 | 10 | 2.00 |
| II | 0.06 | 10 | 2.00 |
| III | 0.10 | 10 | 2.50 |
| IV | 0.20 | 10 | 2.50 |
| V | 0.20 | 10 | 3.00 |
| VI | 0.20 | 10 | 3.00 |
At every visit, repigmentation details and side effects were noted in the patient’s electronic medical record by the trained nurse administering phototherapy. The treating physician reviewed the patient every 3 months and documentation including lesional photographs was entered in the patients’ electronic medical records. These data were used in this retrospective analysis.
The primary efficacy parameter was the number of sessions required for initial repigmentation after treatment commencement. The secondary efficacy parameter was side effects of treatment.
Statistical Analysis
Data are summarised using descriptive statistics in the form of frequencies and percentages for qualitative variables and mean and Standard Deviation (SD) for quantitative variables. Chi-square tests were used for analysing qualitative variables. A p-value of less than 0.05 was considered significant.
Results
One hundred and forty-six patient records were reviewed in this audit. Patient demographic data are presented in [Table/Fig-3].
Patient demographic data.
| Demographic data | NBUVB (50) | Excimer laser (96) |
|---|
| Gender |
| Male | 32 | 42 |
| Female | 18 | 54 |
| Type of vitiligo |
| Vitiligo vulgaris | 50 | 38 |
| Focal vitiligo | - | 52 |
| Acral vitiligo | - | 6 |
| Fitzpatrick’s skin types |
| Skin type III | 2 | 17 |
| Skin type IV | 47 | 79 |
| Skin type V | 1 | 0 |
The number of sessions required to achieve initial repigmentation was the primary efficacy parameter of the study. In the NBUVB group, a mean of 28.91±16.61 sessions were required before initial repigmentation occurred, whereas in the excimer laser group, a mean of 24.26±17.57 sessions were required [Table/Fig-4]. The difference between the two means calculated using the Chi-square test was not statistically significant (p>0.05).
Number of sessions required for onset of repigmentation.
This was represented as descriptive statistics in the form of mean and Standard Deviation (SD) for this quantitative variable
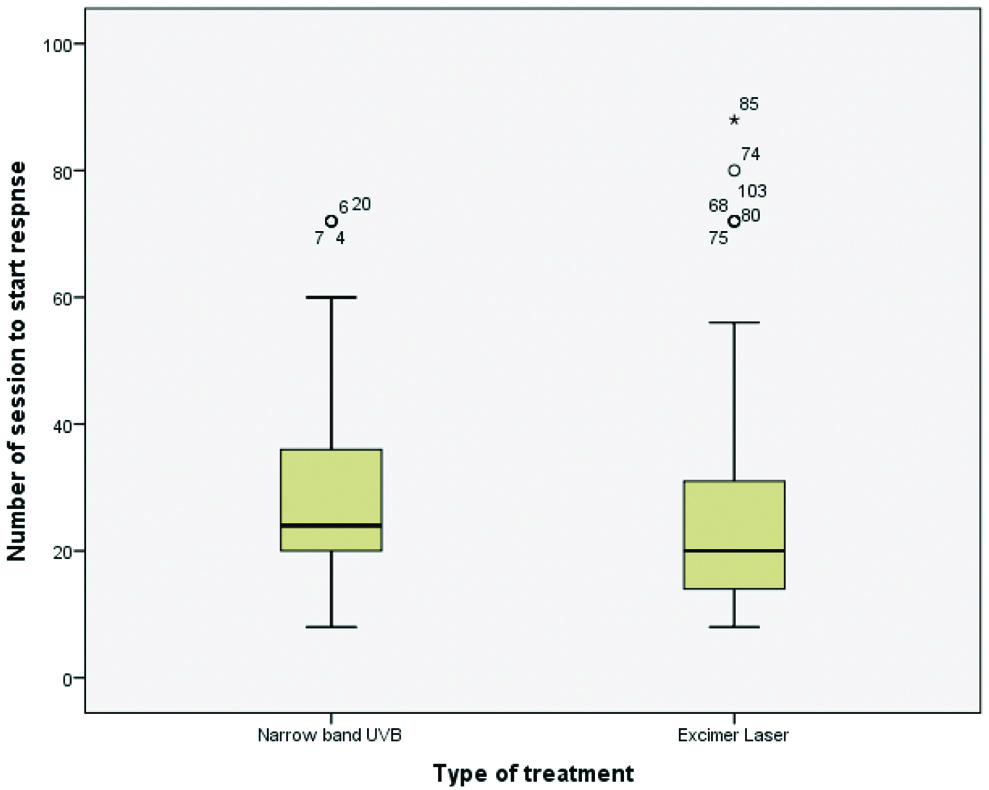
All patients in the excimer laser group (n=96) received treatment twice a week. In the NBUVB group (n=50), 98% of patients received treatment thrice a week and one patient received treatment twice a week. Onset of re-pigmentation was earlier in the excimer laser group compared to the NBUVB group.
Locations that showed faster initial re-pigmentation included the face followed by the trunk in both groups [Table/Fig-5]. More number of patients with facial vitiligo showed re-pigmentation with excimer laser (69.8%, n=67/96) than with NBUVB (64%, n=32/50). However, the difference was not statistically significant (p>0.05).
Location of lesions to respond initially to NBUVB and Excimer laser.
| Groups | Face | Neck | Hand | Arm | Trunk | Leg |
|---|
| NBUVB (n=50) | 32 (64%) | 4 (8%) | 2 (4%) | 3 (6%) | 4 (8%) | 5 (10%) |
| Excimer laser (n=96) | 67 (69.8%) | 5 (5.2%) | 6 (6.2%) | 5 (5.2%) | 9 (9.4%) | 4 (4.2%) |
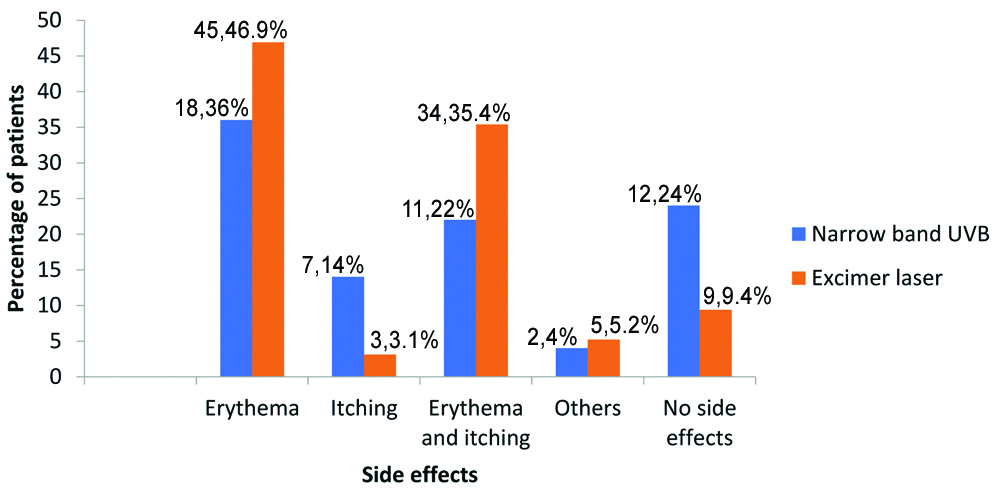
Side effects in both treatment groups were mild and did not necessitate discontinuation of therapy. All patient-reported side effects were considered for inclusion in the analysis and are compared in [Table/Fig-6]. In the excimer laser group, 90.6% (n=87/96) of patients experienced side effects compared to 76% (n=38/50) of patients in the NBUVB group. The difference was statistically significant (p<0.05). Erythema followed by erythema and itching was the most common side effects in both groups. Other side effects included hyperpigmentation, dryness, erythema along with itching and burning. All the side effects were managed by dose reduction and gradual escalation as per protocol. No patient underwent temporary discontinuation of phototherapy.
Side effects in the patients of both the groups.
Other side effects refer to: hyperpigmentation, dryness, erythema along with itching and burning
Discussion
Phototherapy based treatment of vitiligo has evolved from the traditional Psoralen and UVA (PUVA) and broadband UVB based treatments to NBUVB and excimer laser in the last 2 decades [16]. This is attributed to the safety profile and ease of administration of the latter two. This retrospective chart review of 146 vitiligo patients probably represents the largest comparison of patients undergoing NBUVB versus excimer laser in terms of number of sessions required for repigmentation onset and patient-reported side effects. Present study findings demonstrate that onset of repigmentation is marginally earlier with excimer laser compared to NBUVB although, the difference was not statistically significant. Side effects, albeit mild, were significantly higher in patients on excimer laser compared to NBUVB.
A recent study compared histopathological effects on vitiligo skin after treatment with NBUVB and excimer laser twice a week on symmetrical lesions in 30 patients [17]. The authors performed skin biopsies at baseline and after 6 weeks and prepared them for light microscopy and immunohistochemistry with HMB-45 stain for melanin. At 6 weeks, lesions treated with excimer laser showed a statistically significant increase in basal melanocytes, basement membrane thickness and decrease in vacuolated keratinocytes compared to those treated with NBUVB. However, the short duration of 6 weeks was a major limitation of this study as 12 sessions of phototherapy is too early for repigmentation changes to occur in majority of cases. Only a handful of previous studies have compared NBUVB and excimer laser for the number of sessions required for initial repigmentation, type of repigmentation and side effect profile.
Casacci M et al., conducted a randomised investigator-blinded half side comparison multicenter study comparing excimer laser and NBUVB in 21 vitiligo patients [10]. Excimer laser and NBUVB were used to treat symmetric vitiligo patches in nonacral extrafacial areas twice weekly for 6 months. Efficacy of treatment was assessed by number of treatments required for initial repigmentation of at least 25%, number of treatments required for follicular pigmentation and overall repigmetation score at the end of the study. Sixteen patients completed the study. On the excimer laser treated side, a mean of 21.6±8.08 treatments were required for a minimum of 25% repigmentation whereas in the NBUVB treatment side, 27.6±10.29 treatments were required. The difference was statistically significant (p=0.004). The authors noticed faster follicular pigmentation with both excimer laser and NBUVB: 13.06±7.47 versus 15.4±8.53 treatment sessions respectively, although this was not statistically significant (p=0.08). The authors concluded that repigmentation caused by excimer laser occurred earlier and was more prominent than that caused by NBUVB. The major limitation of this study was the small number of patients (n=16).
In another small study by Hong SB et al., 23 symmetrically patterned vitiligo patches in eight patients were treated using excimer on one half of the body and NBUVB on the other half [11]. Only patients with vitiligo vulgaris and acrofacial vitiligo were included [13]. Treatment was carried out twice a week for a maximum of 20 sessions. At the end of 10 sessions, 13/23 (57%) of patches showed ≤25% repigmentation and 3/23 (13%) of patches showed 25-50% repigmentation in the excimer laser group. In the NBUVB group, 5/23 (22%) of patches showed ≤25% repigmentation, and none showed more pigmentation. In conclusion, the authors commented that although improvement was seen in both groups, the degree of repigmentation was considerably greater (p<0.05) in the excimer laser group starting after the tenth treatment session. Comparable to present study findings repigmentation was more obvious and prominent on the face, followed by trunk.
Yang YS et al., compared the repigmentation patterns in 51 patients undergoing NBUVB and 52 patients undergoing excimer laser treatments for vitiligo in a randomised comparative clinical trial [12]. The authors reported that perifollicular repigmentation was the commonest in both groups (42.2% in NBUVB group vs 51.3% in excimer laser group). The authors also observed that the patterns of repigmentation differed in the early responders versus late responders. Marginal repigmentation occurred first in the early responders (>75% repigmentation at 12 weeks) whereas perifollicular repigmentation occurred first in the late responders (<75% repigmentation at 12 weeks). The side effect profile was not recorded in this study. The major drawback of the study was the short duration of 12 weeks. A randomised placebo-controlled trial, an intrapatient comparison of 308 excimer light versus localised NBUVB, evaluated three lesions each in 11 vitiligo patients after 24 treatment sessions. The investigators observed that repigmentation scores of >50% were achieved with NBUVB in 20% of lesions whereas none of the excimer light treated lesions achieved repigmentation >50% at 24 sessions [13]. The authors concluded that localised 311-nm NB-UVB was superior to 308-nm excimer light and should be considered for localised vitiligo as it is easily accessible.
Linthorst Homan MW et al., conducted a randomised comparison of excimer laser versus NBUVB phototherapy after punch grafting surgery in stable vitiligo patients [14]. Fourteen patients underwent punch grafting technique on two symmetrical vitiligo patches. The punch grafted patches were subsequently treated with excimer laser on one side and NBUVB on the other side, twice a week for 3 months and percentage of repigmentation measured by a digital image analysis system. In this study patients’ preference for treatment and satisfaction were also assessed. At the end of 3 months, no statistically significant difference in grade of repigmentation was observed. Patient satisfaction was greater with NB-UVB and preferred it over excimer laser. Inspite of having a small sample size, this study used a digital tool to assess repigmentation and addressed patient preference of treatment albeit postpunch grafting.
Limitation(s)
The major limitation of the study was the need for comparison of the grade and pattern of repigmentation between NBUVB phototherapy and excimer laser, thus providing a quantitative assessment.
Conclusion(s)
Excimer laser and NBUVB phototherapy are both comparable in their onset of repigmentation in vitiligo. The time taken for the onset of repigmentation was similar across both groups. Lesions on the face and trunk repigmented faster with excimer laser compared to NBUVB. Side effects were significantly higher in the excimer laser group. However, they were mild, did not require treatment disruption and were managed by dose reduction according to protocol. Finally, based on this audit, patients can be counselled appropriately regarding repigmentation goals, thereby motivating them to adhere to treatment.