Absolute elimination of all organic and inorganic debris from root canal system even with accurate application of rotary, hand or hybrid instrumentation is difficult, especially from the inaccessible areas of the intricate root canal system. Thus, irrigation forms an integral part of cleaning and shaping [1,2]. Today, despite the best efforts and intentions of researchers and clinicians, it is likely that one of the most neglected procedures in cleaning the root canal is irrigation, especially of the apical third [3].
The conventional endodontic irrigation syringe is most widely used because of ease in manipulation, good control of needle depth and volume of irrigants [2]. One of the modifications from open-ended needle is closed-ended, side-vented channel which claims to reduce the chance of apical extrusion of debris [2].
In order to improve the effectiveness and safety of irrigation procedure, multiple irrigation devices are being developed [3]. Endoactivator (DENTSPLY, USA), produces strong sonically driven movement within the irrigants [4]. The activator tips oscillates and vibrates producing cavitation and acoustic streaming which enhances the disruption of smear layer and intracanal biofilm along with disinfection into various intracanal fins and anastomoses [2,3].
Even when root canal therapy is performed meticulously, there are multiple mechanical and chemical factors which can lead to an unfortunate but common sensation of postoperative pain [5].
Although, there is inconclusive evidence in literature regarding the relationship of vital or necrotic pulp status and severity of postoperative pain, there are multiple contradictory studies, [1,5-12]. One prospective study has reported 63% incidence of postoperative pain at 6 hours and 51% at 18 hours in patients with vital teeth [5]. This is because the aetiology of postoperative pain is multifactorial [7]. Debris and/or irrigants may be extruded into the periradicular tissues during root canal preparation especially during irrigation, inducing flare ups. Thus, great care should to be taken in selecting the proper delivery systems [2]. Routinely in dental practice open-ended needle is used for irrigation [3].
However, no study has been conducted which directly compares the influence of final irrigation using open and closed-ended endodontic needles and an Endoactivator (Dentsply, USA) on postoperative pain. Hence, the aim of this study was to compare postoperative pain after using open and closed-ended endodontic needles and Endoactivator during final root canal irrigation.
The null hypothesis stated that there was no difference in postoperative pain after using open and closed-ended endodontic needles and Endoactivator during final root canal irrigation.
Materials and Methods
The randomised controlled trial was approved by Institutional Review Board of Bapuji Dental College and Hospital, Davangere, Karnataka vide letter no. BDC/Exam/016/2018-19. Patients visiting the Outpatient Department of Conservative Dentistry and Endodontics in Bapuji Dental College and Hospital, Davangere, Karnataka from June 2018 to August 2018 were recruited for the study. Written informed consent from patients participating in the study was obtained. Randomisation was done by an online program (available at www.randomiser.org).
Sample size calculation:
N=2 σ2 (zα/2+zβ)2/δ2 [13]
Where, σ=standard deviation.
Zβ=standard normal variate for power. It is the Z-variate of β error=0.84 (β=0.2)
Zα/2=standard normal variate for level of significance.
α=0.05
δ was expected mean difference between mean values.
Sample size was derived to get the mean difference of percentage reduction in postoperative pain from 8 hours to 48 hours by 9.44 with Standard Deviation (SD)±12.5 at 95% Confidence Interval (CI) and 80% power. Total sample size calculated was 75.
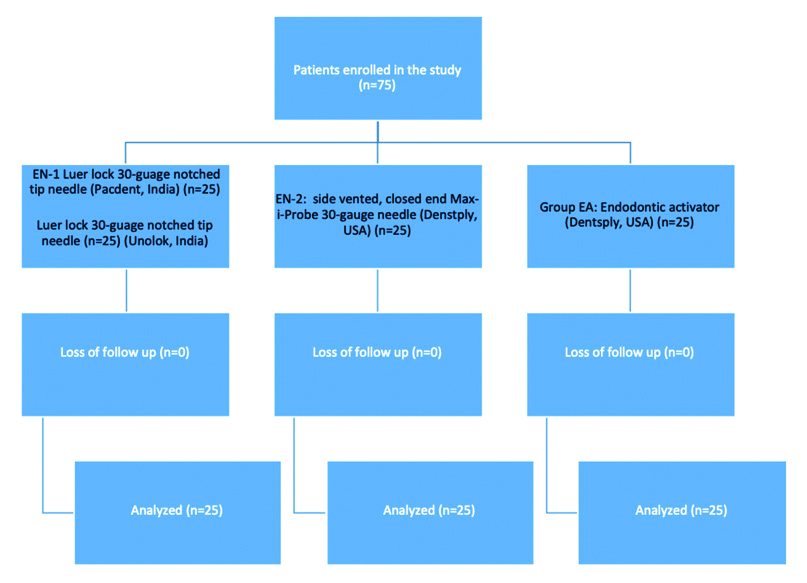
The sample size selected for each group was 25. Group EN-I: Luer lock 30-guage notched tip needle (Pac-Dent, India) Group EN-2: side-vented, closed-ended Max-i-Probe 30-gauge needle (DENTSPLY, USA). Group EA: Endoactivator (DENTSPLY, USA). Only single tooth per patient was endodontically treated during the study. Hence, 25 patients were included in a single group.
Preoperative palpation, percussion tests, pulpal sensibility test using Endo-Frost (Coltene, Switzerland), Electric Pulp Tester (Waldent, India) and radiographs were taken to establish diagnosis and also exclude patients with calcified canals or who had already undergone root canal treatment in the concerned teeth. Only patients diagnosed with symptomatic irreversible pulpitis in mature permanent upper or lower molar teeth were included. Patients included in the study belonged to the age group of 18-65 years. Patients with preoperative pain score from moderate to severe (4-10) on a VAS were included [8]. Those patients with periodontal diseases, who had consumed an analgesic or anti-inflammatory drugs within the last 12 hours, those allergic to NSAID, pregnant or lactating females and patients with any medical conditions were excluded from the study. Data were recorded in the chart which included age, sex, tooth number and intensity of pain.
All the treatments were carried out by a single operator who was a second year postgraduate student of Conservative Dentistry and Endodontics with two years of experience in Endodontics.
Teeth were anaesthetised with 2% lignocaine with 1:80,000 epinephrine (LIGNOX A 2%, India) and isolated using rubber dam. Following conventional access cavities, coronal flaring of the cervical third was performed using Protaper Universal (Dentsply, USA) rotary S1 file. Working Length (WL) was determined using electronic apex locator (Root ZX II; J Morita, Japan) along with 10 K-file (Dentsply, USA) and confirmed radiographically using 15 K-file (Dentsply, USA). The canals were prepared using ProTaper Universal instruments (Dentsply, USA) in a 16:1 controlled torque, low-speed rotary hand piece X-Smart Endo Motor (DENTSPLY, USA) at 250 rpm using the following steps: scouting the coronal two-thirds with size 10 K-file (Dentsply, USA) and shaping with ProTaper rotary files S1 and S2, scouting the apical third with K-files from size 10 to 15 K-file (Dentsply, USA) to Working Length (WL) and shaping with ProTaper rotary files S1 and S2 to WL, finishing the apical third with ProTaper rotary files F1. This was followed by apical gauging using manual hand files and finishing the apical third to the required size (F2/F3/F4/F5) and taper. A 10 k-file (Dentsply, USA) was used to recapitulate and maintain apical patency. All the files were restricted to single use only.
A different final irrigation protocol was performed for each group based on the group assigned [Table/Fig-1]-
Flow diagram for patient enrollment (CONSORT Flow chart).
For group EN-1: 4 mL of 2.5% NaOCl (Prime, India) was delivered into each canal by the Luer lock 30-gauge notched tip (Pac-Dent, India) needle 3 mm short of the WL.
For group EN-2: 4 mL of 2.5% NaOCl (Prime, India) was delivered into each canal by the side-vented, closed-ended 30-gauge Max-i-Probe (DENTSPLY, USA) 1 mm short of the WL.
For group EA: 2 mL of 2.5% NaOCl (Prime, India) was delivered into pulp chamber with Luer lock 30-gauge notched tip needle (Pac-Dent, India). Endoactivator tip (size #15/0.02) (DENTSPLY, USA) was placed loosely at 2 mm from WL and activated at 10,000 cycles/min in each canal along with 2-3 mm vertical strokes to agitate NaOCl (Prime, India) for one minute [4].
Patients were informed about the irrigation devices in general but not about the system used for the particular treatment. After the final irrigation protocol, canals were dried. Closed dressing using Cavit (3M ESPE, USA) was placed.
All participants received a sheet containing VAS after the procedure. Patients were instructed to call the investigator via telephone in case of postendodontic pain. Only then were NSAIDS prescribed to the patients. A total of 650 mg of paracetamol was prescribed as an escape medication if the pain was unbearable. The patient was asked to record the number of tablets intake required to relieve postoperative pain.
After 8, 24 and 48 hours, patients were called by telephone and asked about pain intensity both numeric and verbal (using VAS) and the number of NSAIDs taken.
Statistical Analysis
The data obtained were presented in Microsoft excel. Descriptive analysis, means and standard deviation were calculated using SPSS 20.0 for windows. Comparison between the three groups at each time interval was done using Kruskal Wallis test followed by Mann Whitney U test as post-hoc test. Change in VAS score over different time interval (8, 24 and 48 hours) in each group was compared using Kruskal Wallis test and Mann-Whitney U test. If p<0.05, then it was considered statistically significant.
Results
Mean age of the patients were 36.97±11.102, 39.19±13.975 and 40.02±10.811 years for group EN-1, EN-2 and EA, respectively. Mann-Whitney test in age distribution and Pearson’s test for gender showed no significant relationship between groups with p-value 0.499 and 0.796, respectively [Table/Fig-2].
| Variables | EN-1 | EN-2 | EA | p-value |
|---|
| Age (Mean±SD) (in years) | 36.97±11.102 | 39.19±13.975 | 40.02±10.811 | 0.499* |
| Gender | Male n (%) | 15 (60) | 13 (52%) | 11 (44%) | 0.796** |
| Female n (%) | 10 (40%) | 12 (48%) | 14 (56%) |
*Mann Whitney test; **Pearson’s Chi-square test
Pain score at baseline ranged from 4 to 10 with a mean of 6.24 in group EN-1, 6.12 in group EN-2 and 6.32 in group EA which showed no significant difference using Mann-Whitney test and Kruskal Wallis test. (p>0.05) [Table/Fig-3].
Comparison of pain intensity between the study groups at baseline and three different time intervals.
| Pain | Group | N | Mean (SD) | Range | Median (Q1-Q3) | Kruskal Wallis test | Mann-Whitney U test (p-value) |
|---|
| Chi-square value | p-value | EN-1 vs. EN-2 | EN1 vs. EA | EN-2 vs. EA |
|---|
| Preoperative | EN-1 | 25 | 6.24 (1.72) | 4-10 | 6 (5-7.5) | 0.06 | 0.97(NS) | 0.82(NS) | 1.00(NS) | 0.86 (NS) |
| EN-2 | 25 | 6.12 (1.64) | 4-10 | 6 (5- 7.5) |
| EA | 25 | 6.32 (2.08) | 4-10 | 6 (4-8) |
| 8 hours | EN-1 | 25 | 5.80 (2.75) | 0-10 | 5 (4- 8.5) | 15.17 | <0.001** | 0.002* | <0.001** | 0.54 (NS) |
| EN-2 | 25 | 3.40 (2.22) | 0-10 | 4 (2- 4) |
| EA | 25 | 3.20 (1.92) | 0-9 | 3 (2-4) |
| 24 hours | EN-1 | 25 | 3.96 (1.95) | 0-7 | 4 (3- 5) | 9.34 | 0.009* | 0.07(NS) | 0.002* | 0.42 (NS) |
| EN-2 | 25 | 2.92 (2.53) | 0-10 | 3 (0-4.5) |
| EA | 25 | 2.36 (1.32) | 0-5 | 2 (2-3) |
| 48 hours | EN-1 | 25 | 3.04 (1.62) | 0-7 | 3 (2- 4) | 11.09 | 0.004* | 0.01* | 0.002* | 0.90 (NS) |
| EN-2 | 25 | 1.68 (2.02) | 0-6 | 1 (0-3) |
| EA | 25 | 1.52 (1.45) | 0-5 | 2 (0-2.5) |
*indicates statistical significance (p<0.05)
At 8 hours, pain scores ranged from 0-10 with a mean pain score of 5.80 in group EN-1, 3.40 in group EN-2 and 3.20 for group EA. At 24 hours, pain scores ranged from 0 to 10 with mean pain score of 3.96 for group EN-1, 2.92 for group EN-2 and 2.36 for group EA.
At 48 hours, pain scores ranged from 0 to 7 with a mean pain score of 3.04 in group EN-1, 1.68 for group EN-2 and 1.52 for group EA. Kruskal Wallis test revealed significant difference in all the three time intervals between the three groups with p< 0.05 [Table/Fig-3].
Mann-Whitney U test revealed significant difference between EN-1 and EN-2 (p=0.002) and between EN-1 and EA (p-<0.001) at 8 hour time interval; between EN-1 and EA at 24 hour time interval (p=0.002) and between EN-1 and EN-2(p=0.01) as well as between EN-1 and EA (p=0.002) at 48 hour time interval which was statistically significant. There was no significant difference in postoperative pain intensity between side-vented needle or Endoactivator irrigation.
According to the data representated in [Table/Fig-4], Kruskal Wallis test showed significant difference in NSAIDS intake in all the three group at 8 hours, 8-24 hours and 24-48 hours with p<0.05. There was a significant difference in number of NSAIDS taken at 8 hour between EN-1 and EA (p=0.04) and between EN-2 and EA (p=0.01) while there was no difference between EN-1 and EN-2 (p=0.90). During 8-24 hour interval between EN-1 and EN-2 and EN-1 and EA there was a statsically highly significant difference p<0.001 while there was no difference between EA and EN-2 (p=0.74). During 24-48 hours the comparison between EN-1 and EN-2 and EN-1 and EA showed statsically highly significant differences p<0.001 while there was no difference between EA and EN-2 (p=0.23).
Comparison of number of NSAIDS between the study groups at different time intervals.
| NSAID | Group | N | Mean (SD) | Range | Median (Q1-Q3) | Kruskal Wallis test | Mann-Whitney U test (p-value) |
|---|
| Chi-square value | p-value | EN-1 vs. EN-2 | EN-1 vs. EA | EN-2 vs. EA |
|---|
| 8 hours | EN-1 | 25 | 1.12 (0.78) | 0-2 | 1 (0.5- 2) | 7.05 | 0.03** | 0.90(NS) | 0.04** | 0.01** |
| EN-2 | 25 | 1.12 (0.53) | 0-2 | 1 (1-1) |
| EA | 25 | 0.68 (0.63) | 0-2 | 1 (0-1) |
| 8-24 hours | EN-1 | 25 | 0.84 (0.47) | 0-2 | 1 (1- 1) | 23.38 | <0.001** | <0.001** | <0.001** | 0.74(NS) |
| EN-2 | 25 | 0.20 (0.41) | 0-1 | 0 (0-0) |
| EA | 25 | 0.24 (0.44) | 0-1 | 0 (0-0.5) |
| 24-48 hours | EN-1 | 25 | 0.72 (0.54) | 0-2 | 1 (0- 1) | 23.15 | <0.001** | <0.001** | <0.001** | 0.23(NS) |
| EN-2 | 25 | 0.08 (0.28) | 0-1 | 0 (0-0) |
| EA | 25 | 0.20 (0.41) | 0-1 | 0 (0-0) |
*indicates statistical significance (p<0.05)
Discussion
In clinical investigations, it can be difficult to determine the outcome in relation to pain due to multiple factors affecting the results and subjective perception of pain [7,8].
In the present study, there was no significant difference in the three study groups (p>0.05) in terms of age, gender and preoperative pain. Owing to the simplicity and easy adaptability, VAS is frequently used for pain assessment [5-9,11,14]. Previous studies have shown that incidence of postoperative pain was found to be more in molars that were compared treated to other teeth [1,8-10,13]. Most of the studies which evaluate postoperative pain include maxillary incisors owing to the presence of a single root and root canal. But, as maximum number of endodontic treatments are performed in molars [6,8,14], this study has incorporated both upper and lower molars. In this present study, when using activation of irrigant using syringes, the irrigant had to be placed in the apical third of the canal and hence 4 mL of irrigant was used. But for Endoactivator, the irrigant was to be delivered using 30 gauge notched tip endodontic needle, in the pulp chamber and hence 2 mL of irrigant was used [4].
In this study, irrigation with open-ended needle showed highest postoperative pain intensity at all three intervals (p<0.05) compared to side-vented needle or Endoactivator. The efficiency of needle irrigation depends upon its design as it affects the pattern, velocity and apical wall pressure exerted by the irrigant [3,12,15-18]. Notched needles generate higher apical pressure; can get wedged in the canal, blocking the back flow. Thus, the irrigant does not have any escape route [19-21]. Side-vented needles allow some of the pressure to be vented laterally, allows the escape of irrigants coronally thus, they can be placed closer in the apical third [20,21]. This can be the reason for high postoperative pain at all three different durations, in open-ended needle compared to closed-ended needle group.
Endoactivator generates bubbles which expand and collapse producing miniature shockwaves, reducing the stagnation plane which can breakup bacterial biofilms [4,22-24]. Improved efficiency could explain the less postoperative pain at all time intervals in Endoactivator group compared to group with open-ended needle. Although no significant difference in postoperative pain was observed at different time intervals between Endoactivator and side-vented needle.
In a similar study, the authors observed more postoperative pain and analgesic intake in open-ended syringe irrigation group compared to Endoactivator [9]. In another study, the authors compared postoperative pain in four groups with different irrigating devices and solutions. These groups were 2.5% NaOCl with conventional syringe; 2.5% NaOCl with Endoactivator; NaOCl and QMix with conventional syringe and 2.5% NaOCl, QMix and Endoactivator. The least postoperative pain was noted when both the irrigating solutions were used and activated using Endoactivator [25]. A systematic review evaluated six devices Endovac, Endoactivator, Ultrasonic, manual dynamic agitation, Continuous Ultrasonic Irrigation and Passive Ultrasonic Irrigation, with passive needle irrigation on postoperative pain. It concluded that activating irrigants mechanically is beneficial in reducing postoperative pain [26].
Number of NSAIDS taken by patients was significantly higher in open-ended needle irrigation group compared to side-vented needle and Endoactivator groups at all the three time intervals. There was no significant difference in number of NSAIDS taken in side-vented needle irrigation and Endoactivator group at different time intervals except at 8 hours in which number of NSAID taken was more in side-vented needle group. This is in accordance to a previous study, in which Endoactivator group irrigation activation resulted in significantly less postoperative pain at 8 hours, 24 hours and 48 hours (p=<0.001, <0.001 and 0.006, respectively) and analgesics intake for 0-8 hours and 8-24 hours (p=0.001) than group in which open-ended needle was used [8]. This may be due to the fact that although large amount of irrigant is delivered in the chamber, only few millilitres of irrigant is present inside the canal during agitation [27]. In another study, four activation methods were used. Group 1: Passive side-vented needle, Group 2: Sonic agitation using Eddy, Group 3: Endoactivator and Group 4: Passive ultrasonic agitation. With regards to NSAIDs intake, no statistically significant results were obtained. The authors have concluded that irrigants activation did not make any difference in postoperative pain after 24 hours [28]. This is in contrast to present study.
Currently, there is limited research to recommend a particular irrigation flow rate, specific agitation regimen, volume of irrigant required and ranges of apical pressures within the root canal system [3,16,29,30].
Limitation(s)
There were several limitations in this study. Measuring pain as a variable is difficult because it is difficult to identify the specific cause of pain. There were multiple variables which might have affected the postoperative pain in the study which were difficult to control by the operator including trauma due to rubber dam isolation or to soft tissue caused by anaesthetic injection. Although instrumentation was performed meticulously there are always chances of apical extrusion of debris which will be impossible to detect in an invivo study model. NSAIDs could have been a confounding factor by giving false positive reading for pain reduction. Thus, the VAS score results may not be true representation of pain control as effect of analgesics was not excluded.
Conclusion(s)
It in can be concluded that irrigation activation with open-ended needle showed higher incidence of postoperative pain compared with closed-ended needle and Endoactivator. More randomised controlled trials which can provide us with high level of evidence are required.
*Mann Whitney test; **Pearson’s Chi-square test
*indicates statistical significance (p<0.05)
*indicates statistical significance (p<0.05)