Pyodermas are one of the most common conditions encountered in dermatological practice. They are purulent skin conditions caused by pyogenic bacteria and constitute a large proportion of skin diseases [1,2]. Infections of the skin and soft tissues with microorganisms that produce an inflammatory response from the infected host are known as pyodermas [3]. The group name for dermatoses which are generally purulent are known as pyodermas [4]. The majority of pyodermas are caused by Staphylococcus aureus and Streptococcus pyogenes [5]. Other organisms that may cause pyodermas are coagulase negative staphylococci, Escherichia coli, Citrobacter spp and Pseudomonas aeruginosa [6]. When pyodermas involve normal skin, it is known as primary pyoderma and when it involves infection of previously diseased skin it is known as secondary pyoderma. Primary pyoderma involves the conditions of impetigo, furunculosis, carbuncles, sycosis, follicullitis, cellulitis and ecthyma to name a few. Infectious eczematoid dermatitis, infected scabies, infected contact dermatitis, infected herpes zoster are examples of secondary pyoderma [7]. Malnutrition, overcrowding and poor hygiene lead to higher incidence of pyodermas and they are most common during summer and rainy seasons [8]. Clinical conditions causing immune-suppression like malignancy, diabetes, HIV are an additional risk factors which predispose to increased risk of pyoderma [9].
The prevalence of pyoderma in different studies varies from 1.5% to 16.2% in different regions of the world [5,10]. Occasionally, superficial pyodermas may lead to complications like glomerulonephritis [7]. To treat pyodermas early, identification of causative organisms and initiation of appropriate antimicrobial therapy is essential. These days, many cases do not respond to antibiotics that were previously very effective. The emergence of antibiotic resistance has significantly eroded the utility of established antibiotics and poses a serious threat to public health worldwide. Indiscriminate use of antibiotics, both topical and systemic has led to development of resistance among pathogens which is problematic to the physicians [11].
The present study, attempted to find the prevalence of different types of pyoderma, causative organisms, their antibiotic susceptibility pattern with special reference to Staphylococcus aureus isolates, among patients attending the outpatient and the inpatient wings of the Dermatology Department in a Tertiary Care Hospital. In this region such studies are sparse and hence this study was planned.
Materials and Methods
This hospital based prospective cross-sectional study was conducted for a period of seven months i.e., from 15th May 2019 to 15th December 2019 in a 1750 bedded Tertiary Care Hospital in Odisha, India. The study was approved by the Institutional Ethics Committee. (Letter no. Ref.No.:KIIT/KIMS/IEC/26/2019). Within a period of seven months, a total of 13,496 cases were examined in the outpatient and inpatient wings of the Dermatology Department and of them 402 cases were diagnosed to have pyoderma, which comprised the study population.
Inclusion criteria: Patients belonging to all age groups and either sex with any purulent skin condition presenting to the Dermatology Department (both outpatient and inpatient wings), and giving written informed consent were included in the study. For children less than 18-year-old, parental consent was taken.
Exclusion criteria: Non-infected insect bites and non-inflamed partly healed pyoderma lesions were excluded.
History: History of the patient with regards to mode of onset, history of contact, type, distribution and progression of lesions was taken. Socio-economic status and other relevant history of the patient with respect to associated co-morbidities, details of antibiotic consumption over the last two weeks, occupation, personal habits and hobbies were also recorded [12]. Thorough clinical examination was done to find out the distribution of lesions, the secondary changes, the co-morbidities associated, general health and personal hygiene of the patients.
Specimen collection: A sample of pus was collected on two sterile swabs after cleaning the lesions with normal saline [4]. In case of an intact pustular lesion, it was ruptured with a sterile needle and the material was collected on two sterile swabs. In case of open wounds, the debris was first removed and the lesion was rinsed thoroughly with sterile saline prior to material collection with sterile cotton swab stick. In crusted lesions, the crust was partially lifted and the specimen collected from underneath with a sterile cotton swab stick. Two swab sticks were obtained from the lesion sites [13].
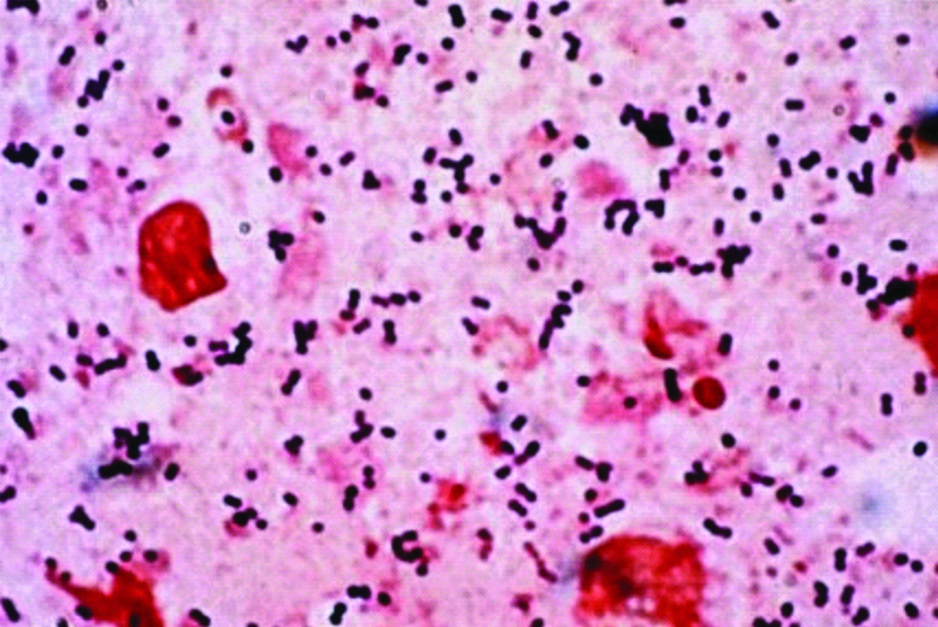
The sample was transported to the microbiology lab within 30 minutes. Gram stain was done with the first swab [Table/Fig-1]. The second swab was inoculated in blood agar and Mac Conkey agar and incubated at 37°C for 24-48 hours.
Image of gram stain of exudate from pyodermal lesion showing gram positive cocci in pairs and clusters.
After 24-48 hours, the culture plates were looked for any growth. Pure bacterial growths obtained after incubation were subjected to various biochemical tests (including gram stain, catalase, slide coagulase, tube coagulase, DNase, oxidase, bile esculin, bacitracin test, indole, methyl red, Voges-Proskauer, citrate, urease, triple sugar iron, phenylalanine deaminase and sugar fermentation) as dictated by the presumptive identifications [14]. Any growth that did not correlate with the gram stain findings was not processed further and was reported as probable contamination. Antimicrobial susceptibility testing was carried out by Kirby-Bauer disc diffusion method and interpreted as per Clinical Laboratory Standard Institute (CLSI) guidelines [15]. A cefoxitin disc was used as a surrogate marker for predicting MRSA isolates. An inhibition zone of ≤21 mm around a 30 mcg cefoxitin disc was considered as MRSA [15].
Statistical Analysis
All the data was entered in a Microsoft excel spread sheet and analysed for variables. Descriptive statistics for both clinical and bacteriological characteristics was generated. Statistical comparison of categorical variables was undertaken using Chi-square test and a p-value of <0.05 was considered statistically significant.
Results
Of the total 13,496 cases examined in the outpatient and inpatient wings of the Dermatology Department, 402 cases were diagnosed to have pyoderma, with a prevalence of 2.9%.
Out of the 402 cases, most of the pyoderma cases were observed in the 11-30 years age group (20.9% in 11-20 year age group and 20.6% in 21-30 year age group), followed by 19.9% in 0-10 years age group and least (1%) in 71-80 years age group [Table/Fig-2]. The mean age was 22±1.5 years, with range 1 year to 78 years. Males (254 cases, 63.2%) outnumbered females (148 cases, 36.8%) cases and the ratio of male to female was 1.7:1.
Age and sex distribution of pyoderma cases (n=402).
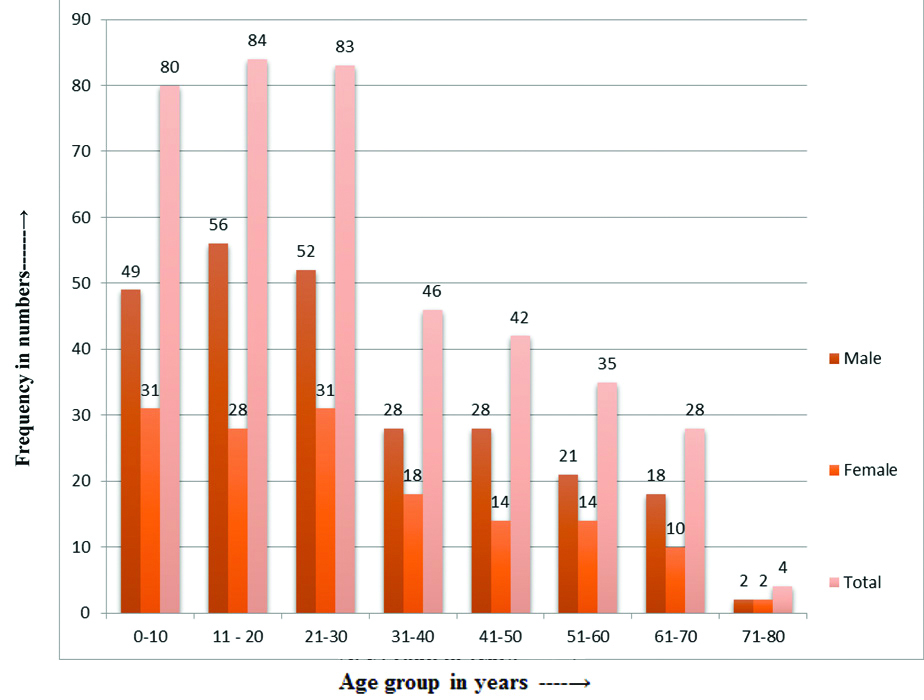
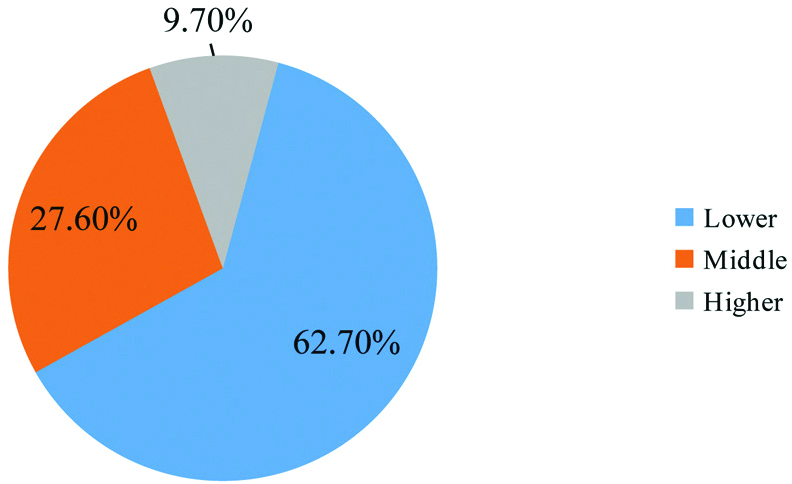
Of the total number of patients who attended the dermatology departments, pyoderma was diagnosed in 3.03% males and 2.89% females. (Among the 13,496 patients attending the dermatology department, 8383 were males and 5113 were females). Gender differences between presence of pyoderma and sex was not found to be statistically significant (p-value=0.66). The prevalence among lower socio-economic class was highest (252, 62.7%) and 111 (27.6%) were affected in middle socioeconomic class (n=402) [Table/Fig-3].
Socio-economic status of the patients (n=402).
In this study, co-morbidities were present in 269 patients [Table/Fig-4]. Gender differences were found to have a statistically significant association in those with anaemia (p<0.001) and hypothyroidism (p=0.002). Three hundred and thirty five patients (83.3%) were unaware of the source of infection, contact at school was seen in 45 patients (11.2%), contact with family members in 18 patients (4.5%) and hospital contact was seen in 4 patients (1%). The most common site of infection was the lower limb [Table/Fig-5]. On gram-staining, gram positive cocci were observed in 82.6% cases and gram negative bacilli in 13.1% cases. As there was no growth in 17 cases, hence the total number of isolates were 385 [Table/Fig-6].
Co-morbidities associated (n=402).
| Co-morbidities (n=269)* | Male (n=147) | Female (n=122) | p-value |
|---|
| Diabetes (n=35) | 25 | 10 | 0.05 |
| Anaemia (n=188) | 87 | 101 | <0.0001 |
| Hypothyroidism (n=46) | 35 | 11 | 0.002 |
*None of the patients had multiple co-morbidities
Lesions in different parts of the body (n=402)*.
| Site | Numbers | Percentage |
|---|
| Head or neck | 49 | 12.2 |
| Upper limbs | 125 | 31.1 |
| Lower limbs | 182 | 45.3 |
| Multiple | 11 | 2.7 |
| Genitalia | 4 | 1 |
| Trunk | 31 | 7.7 |
| Total | 402 | 100 |
*None of them reported multiple sites of infection
Distribution of organisms based on gram’s stain [n=402].
| Type of organism | Numbers | Percentage (%) |
|---|
| Gram positive cocci | 332 | 82.6 |
| Gram negative bacilli | 53 | 13.1 |
| No organisms | 17 | 4.3 |
| Total | 402 | 100 |
*The total number of bacterial isolates were 385
Of the total 402 cases, 317 (78.9%) had primary pyoderma and 85 (21.1%) had secondary pyoderma. Among the 317 primary pyoderma cases, furuncle was present in 143 (45.1%), folliculitis in 81 (25.5%), impetigo in 41 (12.9%), abscess in 23 (7.3%), carbuncle in 18 (5.7%), celulitis in 7 (2.2%) and ecthyma in 4 (1.3%) cases. Among the 85 secondary pyoderma cases, infected eczema was present in 37 (43.5%), infected contact dermatitis in 18 (21.1%), nonhealing ulcers in 14 (16.5%). Miscellaneous group included infected verruca and infected keloid [Table/Fig-7]. The bacteriological analysis showed that Staphylocccus aureus was the predominant organism isolated in 229 cases (59.5%, n=385), 205 being isolated from primary pyoderma cases and 24 from cases of secondary pyoderma [Table/Fig-8]. Of them, 14 strains were found to be Methicillin-Resistant Staphylococcus aureus (MRSA) and the rest were Methicillin Sensitive Staphylococcus aureus (MSSA).
| Type of pyoderma | No. of patients | Age (years) |
|---|
| 0-10 | 11-20 | 21-30 | 31-40 | 41-50 | >50 |
|---|
| Primary pyoderma |
| Impetigo | 41 | 20 | 11 | 7 | - | 3 | - |
| Folliculitis | 81 | 4 | 3 | 32 | 24 | 14 | 4 |
| Ecthyma | 4 | 0 | 0 | 0 | 0 | 4 | 0 |
| Furuncle | 143 | 10 | 28 | 45 | 14 | 21 | 25 |
| Carbuncle | 18 | - | - | 4 | 7 | 7 | 0 |
| Abscess | 23 | - | - | 3 | 3 | 11 | 6 |
| Cellulitis | 7 | - | - | - | 4 | 3 | - |
| Sub total | 317 | 34 | 42 | 91 | 52 | 63 | 35 |
| Secondary pyoderma |
| Infected eczema | 37 | 4 | 4 | 7 | 3 | 5 | 14 |
| Infected scabies | 8 | 4 | 3 | 0 | 0 | 1 | 0 |
| Infected contact dermatitis | 18 | 0 | 7 | 3 | 4 | 0 | 4 |
| Non-healing ulcers | 14 | 0 | 7 | 4 | 3 | 0 | 0 |
| Miscellaneous | 8 | 0 | 0 | 4 | 4 | 0 | 0 |
| Sub total | 85 | 8 | 21 | 18 | 14 | 6 | 18 |
| Total | 402 | 42 | 63 | 109 | 66 | 69 | 53 |
Distribution of isolates.
| Organism | Primary pyoderma N=307 | Secondary pyoderma N=78 | Total no. of isolates N=385 |
|---|
| No. | % | No. | % | No. | % |
|---|
| Staphylococcus aureus | 205 | 66.7 | 24 | 30.8 | 229 | 59.5 |
| Coagulase negative Staphylococcus | 33 | 10.7 | 15 | 19.3 | 48 | 12.5 |
| Beta haemolytic streptococci | 29 | 9.5 | 9 | 11.5 | 38 | 9.9 |
| Escherichia coli | 15 | 4.8 | 9 | 11.5 | 24 | 6.2 |
| Enterococcus | 11 | 3.6 | 6 | 7.7 | 17 | 4.4 |
| Klebsiella pneumoniae | 7 | 2.3 | 9 | 11.5 | 16 | 4.2 |
| Pseudomonas aeruginosa | 3 | 0.9 | 6 | 7.7 | 9 | 2.3 |
| Citrobacter spp | 4 | 1.3 | 0 | 0 | 4 | 1 |
| Total | 307 | 100 | 78 | 100 | 385 | 100 |
All the Staphylococcus aureus strains isolated were sensitive to vancomycin and 96.9% were sensitive to linezolid. Sensitivity to penicillin was 8.3%, to amikacin it was 75.1% and to doxycycline it was 84.3% [Table/Fig-9]. Of the other gram positive cocci isolated, CoNS was highly susceptible to linezolid, vancomycin, their susceptibility being 100%, clindamycin and amikacin, their susceptibility being 95.8% and 85.4%, respectively [Table/Fig-10]. Escherichia coli were 95.8%, 83.3% and 62.5% susceptible to piperacillin-tazobactam, amikacin and gentamicin, respectively [Table/Fig-11].
Antibiotic susceptibility pattern of Staphylococcus aureus.
| Antibiotics | No. of isolates susceptible (%) N=229 |
|---|
| Penicillin G | 19 (8.3) |
| Amikacin | 172 (75.1) |
| Gentamicin | 200 (87.3) |
| Erythromycin | 116 (50.6) |
| Doxycycline | 193 (84.3) |
| Ciprofloxacin | 114 (50.1) |
| Clindamycin | 153 (66.8) |
| Cotrimoxazole | 124 (54.1) |
| Linezolid | 222 (96.9) |
| Vancomycin | 229 (100) |
Antibiotic susceptibility pattern in other (excluding S.aureus) gram positive isolates.
| Antibiotics | CoNS (%) (n=48) | Beta-haemolytic streptococci (%) (n=38) | Enterococcus (%) (n=17) |
|---|
| Penicillin | 10 (20.8) | 15 (37.5) | 8 (47.1) |
| Amikacin | 41 (85.4) | 29 (76.3) | 11 (64.7) |
| Gentamicin | 20 (41.6) | 16 (42.1) | 10 (58.8) |
| Erythromycin | 29 (60.4) | 18 (47.4) | 13 (76.4) |
| Doxycycline | 16 (33.3) | NT | 8 (47.1) |
| Ciprofloxacin | 24 (50) | 10 (26.3) | 9 (52.9) |
| Clindamycin | 46 (95.8) | 33 (86.8) | 13 (76.5) |
| Cotrimoxazole | 34 (70.8) | 25 (65.8) | 12 (70/6) |
| Linezolid | 48 (100) | 38 (100) | 16 (94.1) |
| Vancomycin | 48 (100) | 11 (28.9) | 16 (94.1) |
NT: Not tested; CoNS: Coagulase-negative staphylococci
Antibiotic susceptibility pattern in gram negative isolates.
| Antibiotics | E.coli (%) (n=24) | Klebsiella pneumoniae (%) (n=16) | Pseudomonas aeruginosa (%) (n=9) |
|---|
| Gentamicin | 15 (62.5) | 8 (50) | 5 (55.5) |
| Amikacin | 20 (83.3) | 10 (62.5) | 5 (55.5) |
| Ciprofloxacin | 8 (33.3) | 11 (68.8) | 7 (77.7) |
| Piperacillin | 13 (54.2) | 14 (87.5) | 4 (44.4) |
| Ceftazidime | 12 (50) | 8 (50) | 6 (66.6) |
| Ceftazidime+clavulanic acid | 16 (66.6) | 9 (56.2) | 6 (66.6) |
| Piperacillin+Tazobactum | 23 (95.8) | 15 (93.8) | 6 (66.6) |
| Cotrimoxazole | 2 (8.3) | 1 (6.2) | 2 (22.2) |
| Aztreonam | 3 (12.5) | 5 (31.2) | 3 (33.3) |
Discussion
This study was done over a period of seven months, in a Tertiary Care Hospital, to know the prevalence, types and bacterial aetiology of pyoderma, as well as to know the antibiogram of the organisms causing pyoderma. The prevalence of pyoderma was 2.9%. These findings are comparable to that of Singh A et al., and Ashokan C et al., where the prevalence was 2.5% and 1.55%, respectively [8,16]. Pyoderma was more in males which is also similar with the findings of Bhat YJ et al., [7]. The common age group affected was 11-30 years, which is consistent with the observations of Hulmani M et al., and Ashokan C et al., [11,16]. Higher prevalence (62.7%) was observed in the patients belonging to the lower socio-economic status, which can be compared to the findings of Hulmani M et al., and Gandhi S et al., [1,11]. In the present study, co-morbidities were found in 269 cases (66.9%) with anaemia being the most common morbidity associated. This is in contrast to a study by Singh A et al., where co-morbidities were associated in 29% cases but here too anaemia was the most common associated morbidity [8].
In the current study, most of the patients (83.3%) were unaware of the history of contact and family history of pyoderma was present in 4.5%, which can be contrasted to the study of Nagmoti MJ et al., where 21% of the persons had history of family contact [17]. Majority of the lesions were confined to lower limbs (45.3%) followed by upper limbs (31.1%) which can be compared to a study by Nandihal NW and Ravi GS where 31% of the lesions were on the lower limbs [18]. On Gram staining, 82.6% of cases showed gram-positive organisms and 7.9% showed gram negative organisms which is comparable to the findings of Ghadage DP and Salil YA, where 67% of cases showed gram positive organisms [19].
The prevalence of primary pyodermas (78.9%) was higher than that of secondary pyodermas (21.1%). This is in accordance with the study by Ashokan C et al., where the incidence of primary pyoderma was 60% [16]. Among the primary pyodermas, furuncle was the most common lesion (45%) followed by folliculitis (25.5%). This is in contrast to the study by Badabagni P et al., where the most common lesion among primary pyodermas was impetigo followed by folliculitis and furunculosis [20]. Among the secondary pyodermas, infected eczema was the most common entity (43.5%) which correlates well with the finding of Singh A et al., where the most common secondary pyoderma was infected eczema [8].
The most common organism isolated in pyoderma was Staphylococcus aureus, 229 being isolated (59.5%, n=385), followed by 48 coagulase negative staphylococci isolates. This finding was corroborated by the study by Haibati S and Deshmukh A [21]. Among the Staphylococcus aureus strains, 14 (6.1%) were MRSA strains which can be compared to the findings of Malhotra SK et al., where the incidence of MRSA among Staphylococcus aureus strains was 9.83% [9]. The other organisms isolated in this study were beta-haemolytic streptococci (38-9.9%), Escherichia coli (24-6.2%), Enterococcus (17-4.4%), Klebsiella pneumoniae (16-4.2%), Pseudomonas aeruginosa (9-2.3%) and Citrobacter spp. (4-1%) [Table/Fig-8]. This can be compared with the findings of Malhotra SK et al., where the 6.39% of cases were coagulase negative Staphylococcus, Klebsiella was reported in 4.92%, Citrobacter and Escherichia coli in 1.69% cases [9].
All the Staphylococcus aureus strains isolated were sensitive to vancomycin, 96.9% were sensitive to linezolid. Susceptibility of Staphylococcus aureus to amikacin was 75.1%, to doxycycline it was 84.3%, to co-trimoxazole it was 54.1%, to clindamycin it was 66.8% and to penicillin it was 8.3%. In a study by Singh A et al., strains of Staphylococcus aureus showed susceptibility to amikacin (75%), co-trimoxazole (72%) and clindamycin (61%) [22]. Hulmani M et al., reported the sensitivity of Staphylococcus aureus strains to vancomycin to be 88.24% and to linezolid to be 86.67% [11]. Studies by Jayaraj YM et al., and Ruturaj MK et al., reported the highest antibiotic sensitivity to linezolid (100%), vancomycin (86.32%), amikacin (85.26%), cotrimoxazole (70.53%) and clindamycin (69.47%) [23,24]. Coagulase negative Staphylococcus was most susceptible to amikacin (85.4%), clindamycin (95.8%) and linezolid (100%) and moderately sensitive to doxycycline (33.3%) and gentamicin (41.6%) which is comparable to the study by Singh A et al., [22]. Majority of the Beta-haemolytic streptococci strains in the study were susceptible to amikacin (76.3%), clindamycin (86.8%) and linezolid (100%) which is comparable to the study by Hulamni M et al., and Ruturaj MK et al., [11,24]. In this study E.coli was highly susceptuble to piperacillin and tazobactam (95.8%) and amikacin (83.3%) which can be compared to the findings of Ruturaj MK et al., where E. coli was highly susceptible (100%) to amikacin and piperacillin-tazobactam [24].
To summarise, pyodermas being an important public health problem, cause significant morbidity to patients. In this study, the prevalence of pyoderma was 2.9% with male predominance and was from lower socio-economic group. Majority of the cases belonged to the 11-30 years age group. Anaemia was the most common co-morbidity associated and the prevalence of primary pyoderma was higher than secondary. With the knowledge of the causative organisms and their antibiogram, it will become easier to treat patients empirically rather than wait for culture reports.
Limitation(s)
This study was done in a single tertiary care centre of Eastern Odisha and highlights the clinico-epidemiological features and current pattern of bacterial infections in pyodermas. A larger study involving many centres would be have more validity and scientific rigor to support the findings and bring about changes in practice.
Conclusion(s)
Pyoderma is a major cause of morbidity among patients. In recent times, emerging drug resistant strains are posing difficulties in treating pyoderma. This study will give an idea about the antibiotic sensitivity pattern of the organisms causing pyoderma in this region of the country and encourage judicious use of antibiotics.
*None of the patients had multiple co-morbidities
*None of them reported multiple sites of infection
*The total number of bacterial isolates were 385
NT: Not tested; CoNS: Coagulase-negative staphylococci