Introduction
Night urination severely impacts the quality of life among adults. Coexisting factors such as age, obesity, diabetes, hypertension, cardiac diseases, UTI, asthma, anxiety, and depression are significantly related when voiding episodes exceed two per night. However, understanding its associated factors are essential aspects in the management of Nocturia.
Aim
The aim of the study was to determine the association of nocturia with selected demographic variables, co-morbidities, and the precipitating factors among adults with voiding episodes two or more times and adults who void only once at night.
Materials and Methods
A descriptive cross-sectional design was carried out among 420 adults of age 35-65 years with voiding over two times (Group I) and 206 adults of age 35-65 years who voided only once (Group II) a night. The data was collected from two selected hospitals of Mangalore between January 2018 and June 2019. The written permission was taken from the concerned authority, after obtaining the informed consent from the subjects. The baseline proforma was assessed by the researcher using structured interview schedule and the questionnaire on co-morbidity and precipitating factors such as regular intake of alcoholism, smoking, consumption of coffee, spicy food, anxiety, urinate before bedtime, use of diuretics, day time frequency, underwent surgeries was filled by the subjects. The data was analysed using frequency, percentage, Chi-square test, and logistic regression statistics by Statistical Package for the Social Sciences (SPSS) Version 16.
Results
The study observed that the risk of nocturia was significantly higher among Group I subjects with Urinary Tract Infection (UTI), constipation, hypertension, and on medication for various diseases compared with Group II. The precipitating factors of nocturia revealed that Group I subjects who regularly took coffee, spicy food, had anxiety, daytime frequency, and had undergone various surgeries showed significant difference associated with increased risk of nocturia compared with Group II.
Conclusion
The study findings demonstrate that nocturia is strongly associated with multiple co-morbidities and precipitating factors. These results therefore provide evidence to establish the primary and secondary preventive strategies among adults with nocturia.
Introduction
Nocturia is a very common Lower Urinary Tract Symptom (LUTS). It is defined as ‘the ailment in which a patient has to wake up at night more than once to void, with each void preceding and followed by sleep’ by the International Continence Society (ICS) [1]. It affects male and female patients of all age groups equally, and has higher incidence in the elderly [2]. Despite its prevalence, nocturia yet is a poorly reported, treated, and managed for social and medical issue [3].
The pathophysiology of nocturia is a complex one, and to date, no single direct origin has been established. Several risk factors, e.g., metabolic syndrome, aging, hypertension, congestive heart issues, Diabetes Mellitus (DM), sleep apnea, high nocturnal micturition volume, reduced bladder volume, benign prostate hypertrophy, etc., have been put forward [4,5].
Some studies have observed a significant positive correlation between nocturia and hypertension [6-8], while others have reported none at all relation between the two [9-11]. Häkkinen JT et al., observed no significant correlation between hypertension and nocturia. In their study, symptoms were evaluated twice, i.e., at baseline and five-year follow-up. So, information on the precise time of onset of symptom or deterioration was unavailable [11].
In a study by Liao CH et al., there was significant negative correlation between nocturia and the serum testosterone levels [12]. But, serum hormone levels were determined just once, and the single value is an inaccurate estimate of an individual’s general hormone status and could be affected by individual and analytic errors. Kim JW et al., observed a significant association between nocturia and low testosterone levels. However, the study was a limited, open-label, single-arm pilot research; hence both placebo and control groups were absent [13].
Rembratt A et al., observed no correlation between nocturia and ailments such as DM, angina, known and treated hypertension, or congestive heart issues [10]. However, data on the primary response variable (nightly voids per week) was missing. Furukawa S et al., observed no significant association between diabetic neuropathy/nephropathy and nocturia [14]. This is in contrast with the results of previous studies which could be because of confounding factors, e.g., gender differences, obesity, race, alcoholism, using anti-hypertensive medication, etc. Chiang GSH et al., observed a strong association between nocturia and DM. However, as a majority of the measures that gathered by self-reporting, a recall bias is suspected [15]. Moon S et al., noted that obesity was significantly associated with nocturia, and independent of gender, age, hypertension, and DM. But, though the propensity score technique was carried out for adjusting the randomization influences between control and nocturia groups, some variables were omitted [16]. In a study by Hall SA et al., the use of calcium channel blocker medication among women of age less than 55 had a significant association with nocturia. However, there is lack of data on dosage, usage duration, or even compliance [17].
Co-morbidities of nocturia comprise additional co-occurring conditions such as hypertension, DM, kidney diseases, UTI, constipation, heart diseases, etc., [18]. Multiple precipitating factors like age, BMI, alcoholism, smoking, intake of coffee, spicy food, anxiety, depression, postmenopausal status also may contribute nocturia [19,20]. However, as can be seen, there are divided opinions on their association with nocturia. Therefore, the objective of this research, conducted in South India, is to: (i) establish the association between nocturia and demographic variables such as age, gender, education, marital status, number of children, occupation, etc., (ii) establish the association between nocturia and co-morbidities such as hypertension, DM, cardiac disease, UTI, etc., and (iii) establish the association between nocturia and precipitating factors such as alcoholism, smoking, coffee intake, spicy food intake, etc.
Materials and Methods
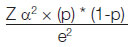
A descriptive cross-sectional design was used in this study to assess the co-morbidity (hypertension, DM, cardiac disease, UTI, Kidney disease, constipation and on medication) and precipitating factors (alcoholism, smoking, consumption of coffee, spicy food, anxiety, urinate before bedtime, use of diuretics, day time frequency, underwent surgeries) associated with nocturia among adults. Institutional Ethical Clearance and permission to conduct the study were obtained from the concerned authority (FMMCIEC/CCM./320/2018, NU/CEC/2017-2018/0170). The sample size was calculated for the group I (nocturia ≥2 voids) based on the prevalence (47%) and the attrition rate was considered as 10%. However, the prevalence 16% was considered for the group II with one episode of nocturia. The sample size estimation was done by using the formula:
The study sample size consisted of 420 adults (Group I) and 206 adults (Group II). Both groups were recruited using purposive sampling.
Inclusion criteria:
Group I:
Age: 35-65 years
Nocturia ≥2 voids
Attending the Departments of Urology and Gynaecology of two selected hospitals in Mangaluru (India)
Able to communicate in English, Kannada or Malayalam,
Selected based on the symptom not by the diagnosis.
Group II:
Age: 35-65 years
Nocturia only once at night
Recruited from the general population of the same hospitals.
Exclusion criteria:
Adults who were on urinary catheter
Pregnant women
Those who had neurogenic bladder.
After obtaining the informed consent, the data collection was done using a questionnaire which was developed by the researcher based on the review of literature and experts’ opinion. The researcher interviewed the subjects to collect the baseline proforma in terms of age, gender, education, marital status, number of children, occupation, monthly income, diet and location of the toilet. Further the self-assessment tool was filled by the subjects which has two parts: (1) Co-morbidities of subjects with nocturia such as hypertension, DM, cardiac disease, UTI, Kidney disease, constipation and on medication; (2) Precipitating factors of nocturia which includes regular intake of alcoholism, smoking, consumption of coffee, spicy food, anxiety, urinate before bedtime, use of diuretics, day time frequency, underwent surgeries.
Statistical Analysis
The data was analysed using frequency, percentage, chi-square test, and logistic regression statistics using Statistical Package for the Social Sciences (SPSS) version 16.
Results
First the association between nocturia and demographic variables were evaluated. A total of 222 (52.9%) subjects in Group I and 100 (48.5%) subjects in Group II were in the age group of 56-65 years. Group I comprised of 264 men and 156 women, and Group II of 112 men and 94 women. The results suggested that education, marital status, occupation, and monthly income were highly significant (p<0.001) and number of children were significant (p<0.045) in Group I and lesser so in Group II [Table/Fig-1].
The association between nocturia and demographic variables among Group I and Group II subjects. (Not significantNS, Significant*, highly significant**).
| Variables | Category | (Group I) n=420 | (Group II) n=206 | p-value |
|---|
| f | % | f | % |
|---|
| Age (Years) | 35-45 | 85 | 20.2 | 47 | 22.8 | 0.581NS |
| 46-55 | 113 | 26.9 | 59 | 28.6 |
| 56-65 | 222 | 52.9 | 100 | 48.5 |
| Gender | Male | 264 | 62.9 | 112 | 54.4 | 0.052NS |
| Female | 156 | 37.1 | 94 | 45.6 |
| Education | Primary | 212 | 50.5 | 61 | 29.6 | 0.001** |
| High school | 160 | 38.1 | 69 | 33.5 |
| Higher secondary | 20 | 4.8 | 19 | 9.2 |
| Graduate | 28 | 6.7 | 57 | 27.7 |
| Marital status | Single | 14 | 3.3 | 20 | 9.7 | 0.001** |
| Married | 406 | 96.7 | 186 | 90.3 |
| Number of children | Nil | 25 | 6.0 | 24 | 11.7 | 0.045* |
| 1 | 307 | 73.1 | 141 | 68.4 |
| ≥2 | 88 | 21.0 | 41 | 19.9 |
| Occupation | Unemployed | 106 | 25.2 | 57 | 27.7 | 0.001** |
| Skilled (Tailor, driver, Painter etc.) | 161 | 38.3 | 81 | 39.3 |
| Unskilled (Daily wages, sweeper, peon, farm worker etc.) | 114 | 27.1 | 25 | 12.1 |
| Professional | 39 | 9.3 | 43 | 20.9 |
| Monthly income (Rs.) | ≤5000 | 18 | 4.3 | 7 | 3.4 | 0.001** |
| 5001-10000 | 260 | 61.9 | 75 | 36.4 |
| 1001-15000 | 77 | 18.3 | 38 | 18.4 |
| >15000 | 65 | 15.5 | 86 | 41.7 |
| Diet | Vegetarian | 43 | 10.2 | 13 | 6.3 | 0.106NS |
| Mixed | 377 | 89.8 | 193 | 93.7 |
| Location of the toilet | Attached to bed room | 155 | 36.9 | 74 | 35.9 | 0.567NS |
| Within the house | 157 | 37.4 | 71 | 34.5 |
| Outside the house | 108 | 25.7 | 61 | 29.6 |
(N=626), <0.05 significant, 0.001** highly significant
Next the association between nocturia and co-morbidities was assessed. Among co-morbid diseases, UTI and constipation were highly significant (p<0.001) and Group I with UTI had 7.98 times {OR 7.98 (CI 5.08-12.58)} and with constipation had 4.01 times {OR 4.01 (CI 2.73-5.89)} the risk for nocturia than Group II. However, Group I subjects with hypertension (p<0.025) {OR 1.50 (CI 1.05-2.15)} and on medication for various diseases (p<0.031) [OR 1.45 (CI 1.03-2.03)] showed significant difference compared with Group II subjects [Table/Fig-2].
Association between nocturia and co-morbidities among Group I and Group II subjects (Not significantNS, Significant*, Highly significant**).
| Variables | Category | (Group I) n=420 | (Group II) n=206 | Chi-square value | p-value | Odds ratio |
|---|
| f | % | f | % |
|---|
| Hypertension | No | 255 | 60.7 | 144 | 69.9 | 5.020 | 0.025* | 1.50 (1.05-2.15) |
| Yes | 165 | 39.3 | 62 | 30.1 |
| Diabetes mellitus | No | 272 | 64.8 | 146 | 70.9 | 2.320 | 0.127NS | 1.32 (0.92-1.90) |
| Yes | 148 | 35.2 | 60 | 29.1 |
| Cardiac disease | No | 378 | 90.0 | 188 | 91.3 | 0.254 | 0.614NS | 1.16 (0.65-2.07) |
| Yes | 42 | 10.0 | 18 | 8.7 |
| Urinary tract infection | No | 195 | 46.4 | 180 | 87.4 | 80.574 | <0.001** | 7.98 (5.08-12.58) |
| Yes | 225 | 53.6 | 26 | 12.6 |
| Kidney diseases | No | 390 | 92.9 | 191 | 92.7 | 0.004 | 0.950NS | 0.98 (0.52-1.86) |
| Yes | 30 | 7.1 | 15 | 7.3 |
| Constipation | No | 201 | 47.9 | 162 | 78.6 | 50.201 | <0.001** | 4.01 (2.73-5.89) |
| Yes | 219 | 52.1 | 44 | 21.4 |
| On medication | No | 202 | 48.1 | 118 | 57.3 | 4.650 | 0.031* | 1.45 (1.03-2.03) |
| Yes | 218 | 51.9 | 88 | 42.7 |
(N=626), <0.05 significant, 0.001** highly significant
Subsequently, the association between nocturia and precipitating factors was evaluated. Analysis of precipitating factors of nocturia reveals that the Group I subjects who consumed coffee and spicy food regularly, had anxiety, daytime frequency, and underwent various surgeries showed significant difference (p<0.001) associated with higher of nocturia {OR 2.39 (CI 1.66-3.43)}, {OR 4.97 (CI 3.47-7.12)}, {OR 3.60 (CI 2.50-5.18)}, {OR 12.19 (CI 8.02-18.52)}, {OR 3.22 (CI 2.16-4.81)}, respectively, compared with Group II subjects [Table/Fig-3].
Association between nocturia and Precipitating factors between Group I and Group II subjects. (Not significantNS, Significant*, Highly significant**).
| Variables | Category | (Group I) n=420 | (Group II) n=206 | Chi-square value | p-value | Odds ratio |
|---|
| f | % | f | % |
|---|
| Alcoholism | No | 296 | 70.5 | 157 | 76.2 | 2.267 | 0.131NS | 1.34 (0.92-1.97) |
| Yes | 124 | 29.5 | 49 | 23.8 |
| Smoking | No | 305 | 72.6 | 160 | 77.7 | 1.840 | 0.174NS | 1.31 (0.89-1.94) |
| Yes | 115 | 27.4 | 46 | 22.3 |
| Coffee | No | 222 | 52.9 | 150 | 72.8 | 22.255 | <0.001** | 2.39 (1.66-3.43) |
| Yes | 198 | 47.1 | 56 | 27.2 |
| Spicy food | No | 95 | 22.6 | 122 | 59.2 | 76.253 | <0.001** | 4.97 (3.47-7.12) |
| Yes | 325 | 77.4 | 84 | 40.8 |
| Anxiety | No | 82 | 19.5 | 96 | 46.6 | 47.283 | <0.001** | 3.60 (2.50-5.18) |
| Yes | 338 | 80.5 | 110 | 53.4 |
| Urinate before bedtime | No | 76 | 18.1 | 44 | 21.4 | 0.948 | 0.330NS | 1.23 (0.81-1.86) |
| Yes | 344 | 81.9 | 162 | 78.6 |
| Use of diuretics | No | 390 | 92.9 | 197 | 95.6 | 1.549 | 0.209NS | 1.63 (0.76-3.51) |
| Yes | 30 | 7.1 | 9 | 4.4 |
| Day time frequency | No | 117 | 27.9 | 170 | 82.5 | 137.366 | <0.001** | 12.19 (8.02-18.52) |
| Yes | 303 | 72.1 | 36 | 17.5 |
| Underwent surgeries | No | 243 | 57.9 | 168 | 81.6 | 32.537 | <0.001** | 3.22 (2.16-4.81) |
| Yes | 177 | 42.1 | 38 | 18.4 |
(N=626)
Discussion
The study showed statistically high significant association of nocturia with baseline characteristics such as education, marital status, occupation, monthly income and significant association with gender and number of children. This result is consistent with a study by Coyne KS et al., on prevalence of nocturia and its effect on health-related quality of life and sleep in a community sample in the USA in which a significant relationship was found between nocturia and marital status and education [21]. van Dijk L et al., observed in their study that the prevalence rate of nocturia in women was 7% higher than in men. This difference of nocturia onset between genders reduces with age [22]. They also noted that women appear to develop nocturia in a more gradual manner than do men over their lives. Another study by Coyne KS et al., on the impact of Overactive Bladder (OAB), incontinence and other LUTS on quality of life showed that OAB has significant association with marital status and education [23].
The study observed that marital status significantly associates with nocturia. In this connection, Shiri R et al., observed that widowers, divorcees, or single people are at more risk for nocturia compared to those living with their partners [24]. Johnson TM et al., concluded that married people are less likely to indulge in negative health traits, e.g., heavy smoking, drinking, physical inactivity etc., than those who are single [25]. Tudiver F et al., noted that in widowers or divorcees, disturbed sleep and psychological/psychosocial issues were more prevalent than in married males [26].
The risk of nocturia was significantly more among Group I subjects with UTI, constipation, hypertension, and those on medication for various diseases compared to Group II subjects. The finding of present study is consistent with the results of Coyne et al which identified that OAB has a high significance with high blood pressure [23].
It is seen that the hypertension is a significant co-morbidity for risk of nocturia. Hypertension and nocturia could be associated because of their influences on tubular transportation and glomerular filtration. The kidney’s role in the hypertension pathogenesis has been supported by experiments indicating a positive association between blood pressure levels and renal sodium excretion [27]. Further, a few studies have noted that some younger to middle aged patients who were in the first stage of essential hypertension had issues of glomerular hyper filtration [28,29]. Hypertension might also be present along with peripheral oedema, the nocturnal re-absorption of which causes higher urine volume. Yet another association between nocturia and hypertension is obstructive sleep apnea that is linked with blood pressure elevation and obesity [30]. Those on medication, according to the results, were at significant risk for nocturia. In this regard, Asplund R observed that the use of diuretics caused a big increase in nocturia in patients of both sexes [4]. According to the study, this high prevalence may be a result of taking the medication in the mornings. In such cases, the diuretics dosage requires adjustment in accordance with its pharmacokinetics. Reynard JM et al., noted that taking diuretic medication six hours prior to bedtime substantially reduced nocturia [31]. Beta-blockers reduce the capacity of bladders and could cause nocturia when ingested just prior to bedtime [32]. Thus, inappropriate timing of medications may lead to nocturia or aggravate it.
The results on the precipitating factors of nocturia reveal that the Group I subjects who took coffee and spicy food regularly, had anxiety and daytime frequency, and had undergone various surgeries showed significant difference associated with increased risk of nocturia compared with Group II subjects. These findings are supported by a study conducted in US among men and women which observed that caffeine intake was significantly associated with urinary incontinence [33]. Another study by Gleason JL et al., assessed the relationship between the intake of caffeine and urinary incontinence among women in the US and concluded that the association was significant [34]. Contrastingly, in other studies, coffee consumption was not associated with nocturia in both male and female subjects, as observed in cohort studies [24,35]. However, a large cross-sectional research in Sweden observed that women having nocturia were less inclined to drink coffee in the evenings, which may not be the case in South India [36].
The study findings point to anxiety being a precipitating factor for nocturia. Even though the precise mechanism which explains an association between anxiety, depression, and nocturia is not known, a few shared patho-physiological pathways might considered. Depressed individuals have more of antidiuretic hormones compared to healthy people [37]. But, these patients lack a normal increase in the level of the hormones. As a result, the loss of cycle of circulating hormones could cause nocturia [36]. This abnormality is a typical mechanism of night-time polyuria in older people, too [38].
It is, therefore, seen that nocturia is not a stand-alone symptom, but is generally combined with co-morbidities and medication use, implying that patients presenting with nocturia will perhaps be ones who are familiar to their doctor owing to their previous complaints. This is significant, since nocturia affects sleep, resulting in poorer quality of life [21]. Hence, doctors need to routinely examine patients presenting with sleep disorders for nocturia.
Limitation(s)
The study focused only on the presence or absence of the co-morbidities and precipitating factors of subjects with nocturia. It was self-reported and conducted by the hospital based survey. Community based study can be replicated. Another limitation was, the cross-sectional nature of the study limited to only two selected hospitals.
Conclusion(s)
The results suggested that education, marital status, occupation, and monthly income were highly significant and number of children were significantly associated with nocturia. The association of nocturia and co-morbidities UTI and constipation were highly significant, while hypertension and taking medications were observed to be significant. The association between nocturia and precipitating factors ‘regular coffee and spicy food intake’, ‘anxiety’, ‘daytime frequency’, and ‘various surgeries’ was seen to be significant. Thus, the study observes a significant association between nocturia and many coexisting factors suggesting that multiple approaches are necessary in the management of adults with nocturia. The underlying causes of nocturia need to be addressed appropriately while deciding the treatment modalities. The awareness of these factors can help the healthcare professionals to attend to the primary prevention of nocturia.
(N=626), <0.05 significant, 0.001** highly significant
(N=626), <0.05 significant, 0.001** highly significant
(N=626)
[1]. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, The standardisation of terminology of lower urinary tract function: Report from the Standardisation Sub-committee of the International Continence SocietyNeurourol Urodyn 2002 21(2):167-78.10.1002/nau.1005211857671 [Google Scholar] [CrossRef] [PubMed]
[2]. Schatzl G, Temml C, Schmidbauer J, Dolezal B, Haidinger G, Madersbacher S, Cross-sectional study of nocturia in both sexes: Analysis of a voluntary health screening projectUrology 2000 56(1):71-75.10.1016/S0090-4295(00)00603-8 [Google Scholar] [CrossRef]
[3]. Oelke M, Anderson P, Wood R, Holm-Larsen T, Nocturia is often inadequately assessed, diagnosed and treated by physicians: Results of an observational, real-life practice database containing 8659 European and US-American patientsInt J Clin Pract 2016 70(11):940-49.10.1111/ijcp.1288227753248 [Google Scholar] [CrossRef] [PubMed]
[4]. Asplund R, Nocturia in relation to sleep, somatic diseases and medical treatment in the elderlyBJU Int 2002 90(6):533-36.10.1046/j.1464-410X.2002.02975.x12230611 [Google Scholar] [CrossRef] [PubMed]
[5]. Yoshimura K, Terada N, Matsui Y, Terai A, Kinukawa N, Arai Y, Prevalence of and risk factors for nocturia: Analysis of a health screening programInt J Urol 2004 11(5):282-87.10.1111/j.1442-2042.2004.00791.x15147543 [Google Scholar] [CrossRef] [PubMed]
[6]. Gourova LW, van de Beek C, Spigt MG, Nieman FH, van Kerrebroeck PE, Predictive factors for nocturia in elderly men: A cross-sectional study in 21 general practicesBJU Int 2006 97(3):528-32.10.1111/j.1464-410X.2006.06029.x16469020 [Google Scholar] [CrossRef] [PubMed]
[7]. Kupelian V, Rosen RC, Link CL, McVary KT, Aiyer LP, Mollon P, Association of urological symptoms and chronic illness in men and women: Contributions of symptom severity and duration-results from the BACH SurveyJ Urol 2009 181(2):694-700.10.1016/j.juro.2008.10.03919091335 [Google Scholar] [CrossRef] [PubMed]
[8]. Markland AD, Vaughan CP, Johnson TM 2nd, Goode PS, Redden DT, Burgio KL, Prevalence of nocturia in United States men: Results from the National Health and Nutrition Examination SurveyJ Urol 2011 185(3):998-1002.10.1016/j.juro.2010.10.08321251675 [Google Scholar] [CrossRef] [PubMed]
[9]. Koskimäki J, Hakama M, Huhtala H, Tammela TL, Association of non-urological diseases with lower urinary tract symptomsScandinavian Journal of Urology and Nephrology 2001 35(5):377-81.10.1080/00365590175322443111771864 [Google Scholar] [CrossRef] [PubMed]
[10]. Rembratt A, Norgaard J, Andersson KE, Nocturia and associated morbidity in a community-dwelling elderly populationBJU International 2003 92:726-30.10.1046/j.1464-410X.2003.04467.x14616455 [Google Scholar] [CrossRef] [PubMed]
[11]. Häkkinen JT, Shiri R, Koskimäki J, Tammela TLJ, Auvinen A, Hakama M, Depressive symptoms increase the incidence of nocturia: Tampere Aging Male Urologic Study (TAMUS)J Urol 2008 179(5):1897-901.10.1016/j.juro.2008.01.03718353384 [Google Scholar] [CrossRef] [PubMed]
[12]. Liao CH, Chiang HS, Yu HJ, Serum testosterone levels significantly correlate with nocturia in men aged 40-79 yearsUrology 2011 78(3):631-35.10.1016/j.urology.2011.05.03321782223 [Google Scholar] [CrossRef] [PubMed]
[13]. Kim JW, Chae JY, Kim JW, Yoon CY, Oh MM, Park HS, Can treatment of nocturia increase testosterone level in men with late onset hypogonadism?Urology 2014 83(4):837-42.10.1016/j.urology.2013.12.06024680454 [Google Scholar] [CrossRef] [PubMed]
[14]. Furukawa S, Sakai T, Niiya T, Miyaoka H, Miyake T, Yamamoto S, Microvascular complications and prevalence of nocturia in Japanese patients with type 2 diabetes mellitus: The Dogo StudyUrology 2016 93:147-51.10.1016/j.urology.2016.03.01726995392 [Google Scholar] [CrossRef] [PubMed]
[15]. Chiang GSH, Sim BLH, Lee JJM, Quah JHM, Determinants of poor sleep quality in elderly patients with diabetes mellitus, hyperlipidemia and hypertension in SingaporePrim Health Care Res Dev 2018 19(6):610-15.10.1017/S146342361800018X29580302 [Google Scholar] [CrossRef] [PubMed]
[16]. Moon S, Chung HS, Yu JM, Ko KJ, Choi DK, Kwon O, The association between obesity and the nocturia in the US populationInt Neurourol J 2019 23(2):169-76.10.5213/inj.1938062.03131260617 [Google Scholar] [CrossRef] [PubMed]
[17]. Hall SA, Chiu GR, Kaufman DW, Wittert GA, Link CL, McKinlay JB, Commonly used antihypertensives and lower urinary tract symptoms: Results from the Boston Area Community Health (BACH) SurveyBJU Int 2012 109(11):1676-84.10.1111/j.1464-410X.2011.10593.x21951754 [Google Scholar] [CrossRef] [PubMed]
[18]. Madhu C, Coyne K, Hashim H, Chapple C, Milsom I, Kopp Z, Nocturia: Risk factors and associated comorbidities; findings from the EpiLUTS studyInt J Clin Pract 2015 69(12):1508-16.10.1111/ijcp.1272726351086 [Google Scholar] [CrossRef] [PubMed]
[19]. de Boer TA, Slieker-ten Hove MC, Burger CW, Vierhout ME, The prevalence and risk factors of overactive bladder symptoms and its relation to pelvic organ prolapse symptoms in a general female populationInt Urogynecol J 2011 22(5):569-75.10.1007/s00192-010-1323-x21104400 [Google Scholar] [CrossRef] [PubMed]
[20]. Oelke M, De Wachter S, Drake MJ, Giannantoni A, Kirby M, Orme S, A practical approach to the management of nocturiaInt J Clin Pract 2017 71(11):e1302710.1111/ijcp.1302728984060 [Google Scholar] [CrossRef] [PubMed]
[21]. Coyne KS, Zhou Z, Bhattacharyya SK, Thompson CL, Dhawan R, Versi E, The prevalence of nocturia and its effect on health-related quality of life and sleep in a community sample in the USABJU Int 2003 92(9):948-54.10.1111/j.1464-410X.2003.04527.x14632853 [Google Scholar] [CrossRef] [PubMed]
[22]. van Dijk L, Kooij DG, Schellevis FG, Nocturia in the Dutch adult populationBJU International 2002 90(7):644-48.10.1046/j.1464-410X.2002.03011.x12410740 [Google Scholar] [CrossRef] [PubMed]
[23]. Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I, The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: Results from the EPIC studyBJU Int 2008 101(11):1388-95.10.1111/j.1464-410X.2008.07601.x18454794 [Google Scholar] [CrossRef] [PubMed]
[24]. Shiri R, Hakama M, Häkkinen J, Auvinen A, Huhtala H, Tammela TL, The effects of lifestyle factors on the incidence of nocturiaJ Urol 2008 180(5):2059-62.10.1016/j.juro.2008.07.04218804241 [Google Scholar] [CrossRef] [PubMed]
[25]. Johnson TM, Sattin RW, Parmelee P, Fultz NH, Ouslander JG, Evaluating potentially modifiable risk factors for prevalent and incident nocturia in older adultsJ Am Geriatr Soc 2005 53(6):1011-16.10.1111/j.1532-5415.2005.53321.x15935026 [Google Scholar] [CrossRef] [PubMed]
[26]. Tudiver F, Hilditch J, Permaul JA, A comparison of psychosocial characteristics of new widowers and married menFamily Medicine 1991 23(7):501-05. [Google Scholar]
[27]. Selkurt EE, Effect of pulse pressure and mean arterial pressure modification on renal hemodynamics and electrolyte and water excretionCirculation 1951 4(4):541-51.10.1161/01.CIR.4.4.54114870266 [Google Scholar] [CrossRef] [PubMed]
[28]. Schmieder RE, Veelken R, Gatzka CD, Rüddel H, Schächinger H, Predictors for hypertensive nephropathy: Results of a 6-year follow-up study in essential hypertensionJ. Hypertens 1995 13(3):357-65.10.1097/00004872-199503000-00012 [Google Scholar] [CrossRef]
[29]. Palatini P, Dorigatti F, Saladini F, Benetti E, Mos L, Mazzer A, Factors associated with glomerular hyperfiltration in the early stage of hypertensionAmerican Journal of Hypertension 2012 25(9):1011-16.10.1038/ajh.2012.7322673015 [Google Scholar] [CrossRef] [PubMed]
[30]. Narkiewicz K, Somers VK, The sympathetic nervous system and obstructive sleep apnea: Implications for hypertensionJ Hypertens 1997 15(12 II):1613-19.10.1097/00004872-199715120-000629488212 [Google Scholar] [CrossRef] [PubMed]
[31]. Reynard JM, Cannon A, Yang Q, Abrams P, A novel therapy for nocturnal polyuria: A double-blind randomized trial of frusemide against placeboBritish Journal of Urology 1998 81(2):215-18.10.1046/j.1464-410X.1998.00511.x9488061 [Google Scholar] [CrossRef] [PubMed]
[32]. Weiss JP, Blaivas JG, Van Kerrebroeck PE, Wein AJ, Nocturia: Causes, consequences and clinical approachesSpringer Science & Business Media 2011 10.1007/978-1-4614-1156-7_1 [Google Scholar] [CrossRef]
[33]. Davis NJ, Vaughan CP, Johnson TM, Goode PS, Burgio KL, Reddend DT, Caffeine intake and its association with urinary incontinence in United States men: Results from National Health and Nutrition Examination Surveys 2005-2006 and 2007-2008J Urol 2013 189:2170-74.10.1016/j.juro.2012.12.06123276513 [Google Scholar] [CrossRef] [PubMed]
[34]. Gleason JL, Richter HE, Redden DT, Goode PS, Burgio KL, Markland AD, Caffeine and urinary incontinence in US womenInt Urogynecol J 2013 24(2):295-302.10.1007/s00192-012-1829-522699886 [Google Scholar] [CrossRef] [PubMed]
[35]. Tettamanti G, Nyman-Iliadou A, Pedersen NL, Bellocco R, Milsom I, Altman D, Influence of smoking, coffee, and tea consumption on bladder pain syndrome in female twinsUrology 2011 77(6):1313-17.10.1016/j.urology.2010.12.07221439616 [Google Scholar] [CrossRef] [PubMed]
[36]. Asplund R, Åberg HE, Nocturia in relation to body mass index, smoking and some other life-style factors in womenClimacteric 2004 7(3):267-73.10.1080/1369713040000139815669551 [Google Scholar] [CrossRef] [PubMed]
[37]. van Londen L, Goekoop JG, van Kempen GM, Frankhuijzen-Sierevogel AC, Wiegant VM, van der Velde EA, Plasma levels of arginine vasopressin elevated in patients with major depressionNeuropsychopharmacology 1997 17(4):284-92.10.1016/S0893-133X(97)00054-7 [Google Scholar] [CrossRef]
[38]. Goessaert AS, Krott L, Hoebeke P, Walle JV, Everaert K, Diagnosing the pathophysiologic mechanisms of nocturnal polyuriaEuropean Urology 2015 67(2):283-88.10.1016/j.eururo.2014.09.00325240972 [Google Scholar] [CrossRef] [PubMed]