Removable prosthodontics is defined as “the replacement of missing teeth and supporting tissues with a prosthesis designed to be removed by the wearer” [1]. Removable partial denture is one of the most accepted means of tooth replacement depending on the patient’s socioeconomic status and clinical scenarios. Many of the patients prefer RPD because of its cost-effectiveness. CAD/CAM design of RPD framework is better in all aspects to conventional RPD when patients are not affordable for implant prosthesis [2]. The indications for removable prosthesis are wide and varied because of its attendant advantages of removable prosthesis on teeth and implants. Removable partial denture can overcome financial limitations, biomechanical and pragmatic issue associated with dental implants [3].
Dental caries is one of the most significant oral health problems. Certain factors play a vital role in the prevalence of dental caries such as diet, socioeconomic status, oral hygiene factors, malnutrition and deleterious habits [4]. The mouth of healthy individuals always contains some amount of streptococcus mutans, due to alterations in the oral environment it can severely alter the homeostatic balance resulting in microbial disease [5]. The relationship between occurrence of caries in relation to wearing a removable partial denture is contradictory. Some studies [6,7], have reported that high caries frequency in individuals wearing a partial denture, but several studies [8-11] shows least caries frequency.
Diabetes is one of the systemic diseases where the individual has a compromised oral and general health. Mageshwari M et al., in the year 2015 reported that dental caries is more prevalent and severe in diabetic patients than nondiabetic. Patients with diabetes are susceptible to develop new and recurrent dental caries. It effects on the oral cavity and its structure, impairs the quality of life [12].
Diabetic patients have altered salivary flow, calcium level and changes in the pH which directly influencing on the prevalence of dental caries. Salivary pH directly influences the calcium deposition and when there is a decrease in pH it results in increased solubility of hydroxyapatite. Changes in salivary composition alter the severity and symptoms in diabetic patients [13].
Apart from that, poor metabolic control, decreased salivary flow and poor oral hygiene also favours the progression of caries. Patients with restrictions of cariogenic food had least caries in diabetes when compare to nondiabetics. Wostmann B et al., reported that diabetes resulting in dry mouth may restrict RPD treatment because of its inability of the mucosa to withstand mechanical trauma [14]. In addition to this, insertion of RPD into the oral cavity may restrict self-cleaning mechanism resulting in accumulation of plaque leading to poor oral hygiene [15].
These factors favour the growth of caries and other infections in diabetic patients when compare to nondiabetic. Therefore, the purpose of the review was: a) To assess the influence of RPD in prevalence of dental caries in partially edentulous patients. b) To evaluate the impact of diabetic condition in prevalence of dental caries compared to nondiabetic patients, so that preventive care can be taken for diabetic and RPD patients in prevention of initiation and progression of caries.
Materials and Methods
This study was carried out in JSS Dental College and Hospital (JSSDCH), JSS Academy of Higher Education and Research (JSSAHER), Mysuru, Karnataka in the year July 2017 and it is not registered in any of the database. The duration of conducting literature search was from July 2017 to Dec 2019. Individuals participating in the study should be partially edentulous and aged between 18 to 64 years either diabetic or nondiabetic. The review was done based on the articles included in Pubmed, Cochrane, Scopus, Google Scholar and Web of Science. The review articles were also collected manually from the journals and online basis from the period July 2017 to December 2019 using the keywords such as diabetes, where diabetes mellitus condition in patients favour an environment for initiation and progression of caries, removable partial denture, which may act as tool for plaque accumulation and which has been used for replacement of natural dentition enhancing prevalence and progression of caries, (Removable partial denture and Diabetes or Oral hygiene), (Removable partial denture and Caries), (Diabetes and Caries). The data required for this literature review was extracted from the results and conclusion from the articles included in the study favouring the hypothesis of this study such that removable acrylic partial denture had a significant effect on prevalence of dental caries in partially edentulous patients and diabetic condition favouring the prevalence of dental caries. [Table/Fig-1] shows flow diagram of the study selection process.
The flow diagram of the study selection process. (N indicates number of articles).
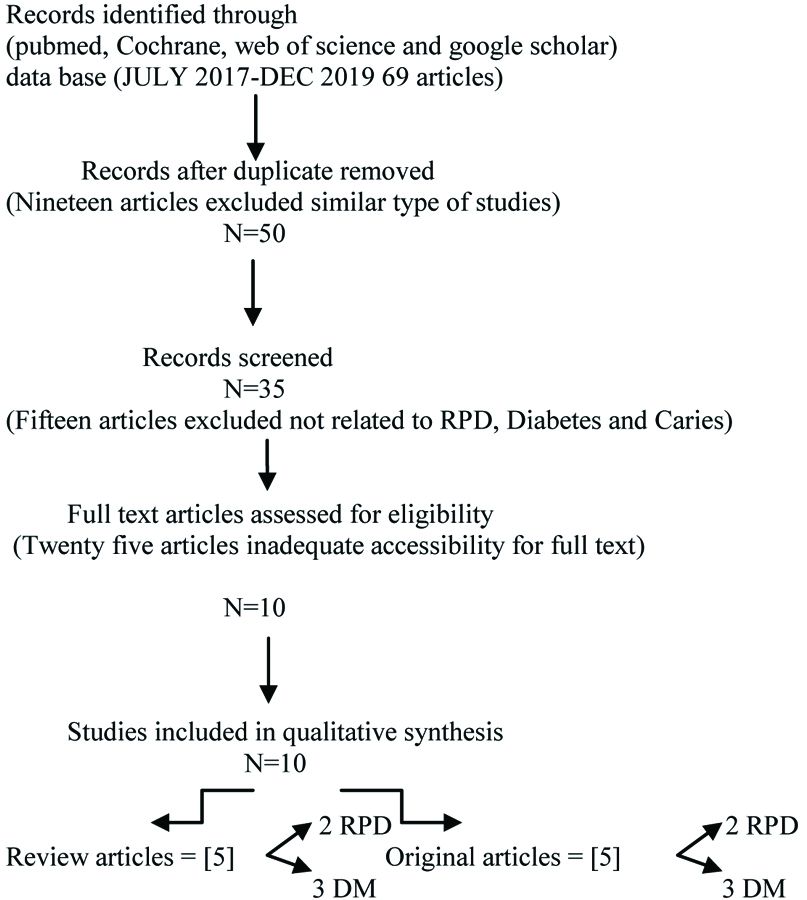
Totally sixty nine articles were collected, after screening ten articles were selected for the review process among which five are review articles and five are original research articles.
Records identified through (Pubmed, Cochrane, Web of Science and Google Scholar) data base (JULY 2017-DEC 2019 69 articles).
Selection Criteria
Types of Study
The review included any type of study (example original research, review articles) as well as systemic reviews. Case series and reports were excluded.
Types of Participants
Inclusion criteria for potentially eligible studies were partially edentulous patients and removable partial denture wearers who over the age of 18 years and classified as either diabetic/non-diabetic based on medical history and random blood sugar level.
Types of Intervention
1) Oral hygiene motivation prior to and during treatment with RPD.
2) Replacement of ill-fitting dentures.
3) Report to follow-up period that is minimum of six months after the insertion of RPD.
4) DMFT index applied before the insertion of the RPD.
5) Existing carious lesions were treated before insertion of prosthesis.
6) The oral hygiene status should be 0.1-1.2 (Greene and Vermillion oral hygiene index).
7) Partially edentulous diabetic patients with random blood sugar level more than 160 mg/dL.
Excluded Studies
Nineteen articles excluded at the initial screening stage with 50 articles considered as relevant for further processing. The reason for exclusion was there resemblance with similar type of studies. Fifteen articles again excluded which were not related to either RPD, diabetes or caries. Due to inadequate accessibility for full text twenty five articles were again excluded. There was no restriction in the language of studies.
Results
The literature review of this study in which 10 articles were selected for the review analysis, in which five original articles and five review articles strongly support the hypothesis of the study. Among them, two articles from original research and review are related to RPD, three articles from original research and review are related to diabetes, influencing on prevalence of caries. [Table/Fig-2] indicates the original research articles included in this literature review.
Indicates the original research articles included in this literature review in which article ref no [8,16] shows RPD and caries prevalence, ref no [13,17,18] shows diabetic condition and caries prevalence.
| Ref No., Author, Place | Clinical finding | Study population | Year | Conclusion |
|---|
| [8] Tuominen R et al., Finland | Caries prevalence61.4% (n=4144) without RPD60.5% (n=774) Single RPD User 62.7% (n=110) RPD in both the jaws | Nondiabetic | 1988 | RPD in both jaws shown slight increased risk of having carious teeth.RPD is considered as a device accumulating plaque on tooth surface |
| [13] Singh A et al., Rajasthan | Caries prevalence (DMFT Index Mean and SD)12.6±0.48 - Diabetic patients2.67±0.14 - Nondiabetic patients | Diabetic and Nondiabetic population | 2014 | Salivary calcium, flow rate, and pH are in direct relation with dental caries. In diabetic condition salivary components deteriorates creating a favourable environment for the progression for caries |
| [16] Rodan R et al., Jordan | Caries Index Rate-RPD WearerCoronal caries- 0.023Root caries- 0.025NonRPD wearerCoronal caries- 0.0078Root caries- 0.0072 | Nondiabetic population | 2012 | Wearing of RPDs increased coronal and root surface caries |
| [17] Goyal D et al., Haryana | Caries prevalence (DMFT Index Mean and SD)6.26±3.72 Nondiabetic4.52±1.560 Controlled Diabetic patients8.6±4.01- uncontrolled diabetic patients | Diabetic and Nondiabetic population | 2012 | Diabetes mellitus have a direct effect on salivary PH reducing it from normal levels.Lower incidence of caries in controlled diabetics suggest that diet plays an important role |
| [18] Machado D et al., Portugal | | Nondiabetic | Type 1 Diabetic | Diabetic and Nondiabetic population | 2017 | No higher prevalence of tooth decay lesions in patients with type I diabetes mellitus compared to nondiabetic patients |
| Decayed | 4.13 | 3.83 |
| Missing | 1.57 | 1.43 |
| Filled | 2.07 | 2.73 |
Indicates review articles included in this literature review in which article ref no [14,15] shows RPD and caries prevalence, ref no [12,19,20] shows diabetic condition and caries prevalence.
| Ref No., Author, Place of study, Population | Year and Type of article | Objectives of the study | Number of articles reviewed by the author | Conclusion |
|---|
| [12] Mageshwari M et al., Chennai, Diabetes | 2018A Review Article | To assess the diabetic condition status favouring an environment for the prevalence of dental caries | 60 | A complex relationship between the type II diabetes mellitus and dental caries even though very well controlled diabetic patients tends to show a lower dental caries index when compared to nondiabetic controls. |
| [14] Wostmann B et al., Germany, Non Diabetes | 2005A literature Review | To evaluate indications for the use of removable partial dentures | 85 | There is strong evidence of an association between the use of RPD’s and root surface caries in elderly nondiabetic persons. |
| [15] Ezawi AAE et al., London, Non Diabetes | 2017A Systematic Review | RPD insertion has a deterioration effect on the oral health status | 43 | RPD promote accumulation of the plaque in the absence of good oral hygiene which may in turn lead to higher risk of dental caries |
| [19] Gowdar IM and Almuhaiz M, Saudi Arabia, Diabetes | 2016A Review | Diabetic condition has impact on oral health | 58 | Dental caries in diabetes is related to poor metabolic control, salivary gland hypofunction and high salivary glucose concentrations which promotes growth of Streptococcus mutans and lactobacillus |
| [20] Ship JA, New York, Diabetes, USA | 2003An overview | Summarise the diabetic condition status of the oral health and dental treatment considerations | 54 | Patients with diabetes are susceptible to oral sensory, periodontal and salivary disorders which could increase their risk of developing new and recurrent dental caries. |
In relation to RPD and partially edentulous patients, reference number [8] in [Table/Fig-2] states that patients wearing RPD in both the jaws had shown high caries prevalence, but it is not statistically significant when compared to patients without RPD and with single RPD among nondiabetic patients. Reference number [16] shows high caries prevalence which is statistically significant in RPD wearers among nondiabetic patients. In relation to diabetic and nondiabetic patients, [Table/Fig-2] shows high caries prevalence in diabetic condition which is statistically significant compare to nondiabetic patients without RPD [13]. In [17], controlled diabetic patient’s shows statistically significant low caries prevalence when compare to nondiabetic and uncontrolled diabetic patients without RPD. In [18] indicates no statistical significance between decayed, missing, filled teeth among type I diabetic and nondiabetic patients.
[Table/Fig-3] Indicates review articles included in this literature review. [Table/Fig-3] [14,15] review articles support high prevalence of caries in RPD wearing non diabetic patients compare to nonwearers. [Table/Fig-3] conclusion favours the result that good metabolic control and maintaining good oral hygiene in diabetic patients contributes to low caries prevalence and prevention of dental caries [12,19,20].
Discussion
Role of RPD in Dental Caries Prevalence
A RPD while restoring the functions can damage surrounding hard and soft tissues resulting in gingival inflammation, periodontitis, tooth mobility and dental caries. It can also influence the quality and quantity of plaque resulting in gingival inflammation or caries status as observed on the supporting teeth [15]. It was noticed that Staphylococcus was found in abundance in the plaque of diabetic patients wearing RPD compare to nondiabetic patients [21].
High caries index rate was noticed in RPD wearers when compare to nonwearers. Rodan R et al., revealed that teeth next to edentulous area have similar caries rate to that of abutment teeth in denture wearers. Apart from that Authors also mentioned that irrespective of patients having satisfactory or unsatisfactory removable partial dentures there was no influence on caries prevalence [16].
Further in some reports, it was mentioned that increase in Streptococcus mutans quantity in saliva is directly proportional to insertion of removable partial dentures. This shows that patients wearing RPD are at higher risk for caries when compare to nonwearers [22].
Poorly designed RPD and poor oral hygiene results in plaque accumulation which enhances risk for caries [15]. Apart from this proximal areas of abutment teeth supporting prosthesis is difficult to clean resulting in progression of caries [23]. It is also mentioned that RPD with fairly large plate and hook-shaped drawn steel clasp to ensure retention results in plaque accumulation ending with progression of caries [24].
Individuals with greater number of remaining natural teeth have more surface area and are at risks for caries and the proportion of filled teeth can be expected to represent cumulative caries treatment. RPDs decrease the probability or the amount of caries would be biased because of the confounding effect of oral health habit and oral status difference. Subjects who are wearing two RPDs have an average more teeth in contact with denture than those wearing single RPD, which may explain the almost significant increase in the probability of caries among those wearing two RPD [8].
Partial acrylic dentures in contact with large surface area of all remaining teeth results in high plaque index of all teeth. It is also stated that after six months of wearing acrylic removable partial denture it results in increase in plaque index which is favouring environment for progression of caries [25]. Clasp, rests and denture bases interfere with oral hygiene and acts as an area for bacterial attachment. It results in increased proportion of Streptococcus mutans resulting in demineralisation. Therefore, all precautions to be taken in reducing Streptococcus mutans in these patients during the initial therapy phase before placement of RPD [26].
Tanaka J and Tanaka M also reported an increase in the LB counts in presence of dentures. The bacterial attaches to the rough surface of the dentures or the inner surface of the acrylic dentures in which residual foods easily enters where the self-cleansing would be difficult [27].
Role of Diabetes in Caries Prevalence
Diabetes is considered as a risk factor for oral diseases especially for dental caries. Apart from that, it results in periodontal diseases and tooth mobility. It can influence the quality and quantity of saliva. The buffering capacity of saliva has a protective effect by neutralising pH in oral cavity after sugar intake thereby influencing the prevalence of caries [28]. It has a major influence on caries initiation by means of plaque formation rather than by direct contact on tooth surface [29].
Risk for dental caries in diabetic patients is three-fold that of nondiabetic patients. The reason behind this was alteration in the composition of saliva which resists the process of remineralisation [13]. Individuals with controlled diabetics had lower incidence of caries when compare to uncontrolled diabetic patients suggesting that diet plays an important role in caries prevalence [17]. It is reported that high salivary glucose concentration correlates with high blood glucose concentration resulting in increase in the number of lactobacilli and yeast in saliva. Salivary gland hypofunctions also contributes to the growth of Streptococcus mutans [19].
Increase concentration of salivary glucose in the oral environment promotes bacterial growth and proliferation, increase in lactic acid products and decrease in pH [18]. This is because of increased glucose level which alters the plaque microflora. This results in increase in colony-forming units of Streptococcus mutans in saliva of patients with carious teeth and in gingival crevicular fluid.
Canepari, 1919 reported that early gingivitis an ecological niche may create an environment for the growth of Streptococcus mutans along with the other species [30]. Miralles L et al., had stated that due to gingival recession and aging factors in diabetic patients, caries initiates in root or at below CEJ where saliva is also a contributing factor [31].
The cariogenic effect of refined carbohydrates and a significant higher glucose content in the saliva and gingival fluid of diabetes has made us to pay special attention to the cervical areas because of higher possibilities of caries appearance there [32]. Patients with diabetes are subjected to new or recurrent caries in type I diabetes due to chronic immunosuppression and acute hyperglycemia, whereas in type II diabetes [20]. It interferes with the dental pulp healing inhibition of dentinal bridge and increase in pulpal inflammation after pulp capping procedures [33]. Studies had revealed that dental caries increased with age as well as increased with blood glucose level [34].
Limitation(s)
This review gives limited data for further data synthesis and gives a major impact on the quality of life of RPD wearers and requires further investigation in future reviews on the impact of RPDs in the oral cavity and diabetic condition favouring the prevalence and progression of caries.
Conclusion(s)
Patients wearing an acrylic removable partial denture have been noted for increased risk of having carious teeth. Dentures that are initially compatible, over the period of time, affect the oral condition of the individuals directly or indirectly, if not monitored properly and the oral hygiene not maintained. Diabetic factors also contribute to increased risk of caries due to poor metabolic control, salivary gland hypofunction.