A Case of Pseudoepitheliomatous Keratotic and Micaceous Balanitis with Verrucous Carcinoma
Yu-Hua Yang1, Ren-He Chen2, Ru-Zhi Zhang3
1 Department of Dermatology, The Third Affiliated Hospital of Soochow University, Changzhou, Jiangsu, China.
2 Department of Dermatology, ZhenJiang First People’s Hospital, Changzhou, Jiangsu, China.
3 Department of Dermatology, The Third Affiliated Hospital of Soochow University, Changzhou, Jiangsu, China.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Ru-zhi Zhang, Department of Dermatology, The Third Affiliated Hospital of Soochow University, 185 Juqian Road, Changzhou-213003, Jiangsu, China.
E-mail: zhangruzhi628@163.com
Pseudoepitheliomatous Keratotic and Micaceous Balanitis (PKMB) is a rare chronic inflammatory disease characterised by hardened, hyperkeratotic plaques on the glans of the penis of older men. Although PKMB is described as benign, there is growing evidence that it has the potential to become cancerous. authors hereby report a case of 55 year old male who was initially characterised by white sclerosis and atrophy at the glans. Without treatment, verrucous keratinising organisms appeared after two years and were misdiagnosed as viral warts. The patient received four cryotherapy treatment with liquid nitrogen, which completely removed the warts, but the rash recurred about two months after cryotherapy. The patient received histopathological examinations which showed obvious hyperkeratosis with incomplete keratosis in the epidermis, papilloma-like and pseudoepithelioma-like hyperplasia appeared in the spinous layer, flattening of rete ridges, squeezing growth into the dermis, disordered arrangement of basal cells and frequent mitoses. A few squamous masses were seen in the dermis and the formation of squamous fossa could be seen. There were more lymphocyte infiltrations in the superficial layer of the dermis and around blood vessels. After being diagnosed with PKMB with verrucous carcinoma, the patient finally chose to undergo surgery in the Urology Department of another hospital. Unfortunately, we lost the follow-up. Our case supports the view that PKMB can develop into a malignant disease, which suggests that early detection, treatment and follow-up of the disease are essential.
Glans penis, Hyperkeratotic, White sclerosis
Case Report
A 55-year-old male patient presented with a complaint of white sclerosis of the glans and coronal sulcus of his penis. It started as white hardening and atrophy of glans penis three years ago, which was painless, and he did not receive any treatment at that time. Subsequently, the rash gradually increased to 1×1.5 cm and spread to the coronary sulcus, and two years ago, verrucous keratinising organisms began to appear on the glans. The patient was diagnosed with “viral warts” in many medical institutions and received four cryotherapy with liquid nitrogen which completely removed the warts. However, the rash recurred about two months after cryotherapy. The patient underwent a circumcision four years ago and denied a history of travel or that anyone in his family had a similar condition.
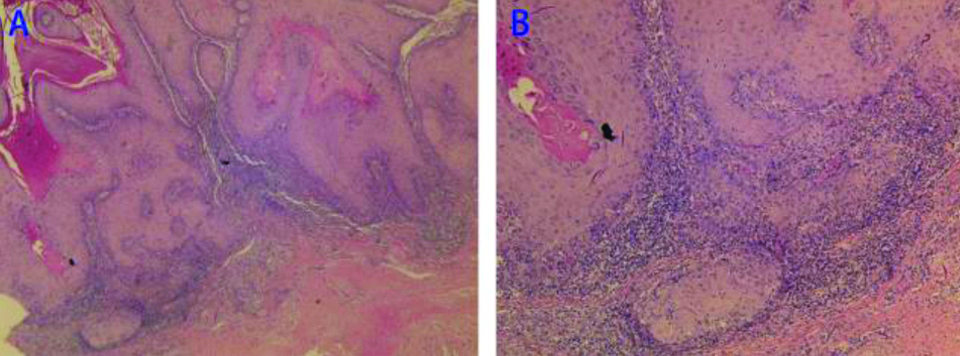
The general condition upon physical examination of the patient was good, and there was no special abnormality noted. The skin condition of his glans and coronal groove surface skin was 1×1.5 cm white with sclerosing atrophy, hard texture and no tenderness. Verrucous growth of the nail cover can be seen at the glans [Table/Fig-1]. No abnormality was found in routine blood analysis, liver function, biochemistry, blood coagulation function, Anti-Human Immunodeficiency Virus (HIV) antibody, Treponemal Pallidum Particle Agglutination (TPPA) and Rapid Plasma Reagin test (RPR). In view of the repeated skin lesions, a skin biopsy of the lesion was taken. Histopathological examination showed that there was obvious hyperkeratosis with incomplete keratosis in the epidermis, papilloma-like and pseudoepithelioma-like hyperplasia appeared in the spinous layer, flattening of rete ridges, squeezing growth into the dermis, disordered arrangement of basal cells and frequent mitoses. A few squamous masses were seen in the dermis and the formation of squamous fossa could be seen. There were more lymphocyte infiltrations in the superficial layer of the dermis and around blood vessels. These findings were consistent with verrucous carcinoma [Table/Fig-2]. The patient was eventually diagnosed with PKMB with verrucous carcinoma. The patient requested to continue treatment in the Urology Department of another hospital, so we lost the follow-up. The presentation of the case was approved by the patient.
The glans and coronal groove surface skin was white with sclerosing atrophy, hard texture and no tenderness. Verrucous growth of the nail cover can be seen at the glans.

A) Histopathology of the lesional biopsy. Obvious hyperkeratosis with incomplete keratosis is visible in the epidermis, papilloma-like and pseudoepithelioma-like hyperplasia appeared in the spinous layer, flattening of rete ridges, squeezing growth into the dermis, disordered arrangement of basal cells and frequent mitoses. B) A few squamous masses can be seen in the dermis and the formation of squamous fossa can be seen. There are more lymphocyte infiltrations in the superficial layer of the dermis and around blood vessels. These characteristics are consistent with verrucous carcinoma. (A,×40. B,×100. H&E stain).
Discussion
Pseudoepitheliomatous Keratotic and Micaceous Balanitis (PKMB) is a very rare chronic inflammatory disease that mainly occurs in the prepuce glans of middle-aged and elderly men [1]. The disease was first described in 1961 and was named according to its clinical and histological features [2]. The exact pathogenesis of PKMB is still unknown. Phimosis and Human Papilloma Virus (HPV) infections are the most frequently reported and possibly related factors, but the exact aetiology and susceptibility factors are still uncertain [3]. An obvious related factor in this patient was a circumcision. According to current reports, patients with PKMB are usually over 50-year-old with a history of circumcision, and the reason for that operation was usually acquired phimosis. In the reported cases, the causes of phimosis were also different. Another frequently reported possible cause is a HPV infection, but as in this case, most cases are not examined for HPV genomes, so there is a lack of sufficient data. Kang BS et al., used broad spectrum Polymerase Chain Reaction (PCR) technology and restriction fragment mass polymorphisms to identify HPV in skin lesions of a patient with PKMB, and HPV81 was detected [4]. However, in a different case of verrucous carcinoma caused by PKMB, HPV in-situ hybridisation and PCR analysis were negative in the tumour and PKMB lesions [5]. Therefore, the role of HPV in the pathogenesis of PKMB needs to be further studied.
The main clinical manifestation of PKMB is sclerosing keratotic plaques in the glans, giving rise to the name “mica”, which indicates that the plaques are covered with white scales. The disease usually progresses slowly and has no obvious other symptoms. There may be pain when the skin lesions are chapped or impregnated. It very rarely affects the urethra, which can lead to urinary tract obstruction and bifurcation. Pathologically, PKMB shows significant hyperkeratosis with incomplete keratosis, pseudoepithelioma-like hyperplasia, spinous layer hypertrophy and so on. The disease can be diagnosed according to its typical clinical symptoms and pathological features [6]. Clinically, it is necessary to distinguish PKMB from other diseases such as lichen sclerosus et atrophicus and erythroplasia of queyrat that can occur in the glans of the prepuce. Lichen sclerosus et atrophicus [7] is usually characterised by clear white patches, surrounded by edematous erythema, and hard and shiny skin, usually with symptoms such as itching, burning pain or dysuria. Erythroplasia of queyrat [8] is usually seen as a single bright red or bright erythema with a glossy surface, and histopathology shows obvious hyperplasia and hypertrophy of the mucosal epithelium. At sites of hyperplasia, the structure of normal epithelial mucosa disappears and is replaced by hyperplastic atypical epithelial cells.
The most prominent feature of this patient is that a verrucous carcinoma appeared. In this case, white sclerosis and atrophy appeared in the glans three years ago, and verrucous proliferative changes appeared one year later. PKMB was previously thought to be a benign disease, but there is an increasing number of reports of secondary verrucous or squamous cell carcinoma [9,10]. A few cases have reported fibrosarcoma of the penis and cutaneous horn secondary to PKMB [11,12]. Therefore, some scholars have suggested that the disease should be renamed mica verrucous malignant balanitis. Krunic AL et al., divided the clinical development of PKMB into four stages: plaque stage, tumour stage, verrucous carcinoma stage and squamous cell carcinoma stage [13]. At present, there is increasing evidence that PKMB is likely to be a precancerous state or a locally invasive low-grade malignant tumour. In this case, the patient eventually developed verrucous carcinoma. This indicates that PKMB may be a precancerous state of verrucous carcinoma.
At present, it is advocated that different treatment measures should be taken according to the different clinical stages. The plaque stage is mainly treated with topical drugs, such as retinoic acid cream, glucocorticoid, and by subcutaneous injection of Interferon-α (IFN-α), cryosurgery and electrocoagulation, but the efficacy of those treatments is not satisfactory [14]. Recently, it was reported that photodynamic therapy or 5-fluorouracil can achieve better results [15,16]. Local resection is often used in the tumour stage. Partial penis resection or even a radical operation is often used in the verrucous carcinoma stage and squamous cell carcinoma stage. When the effects of topical drug treatments are not good, it should be suspected that the skin lesion has progressed to the tumour stage. Our patient was confirmed to have advanced to the verrucous carcinoma stage, so he was transferred to the Urology Department for surgery.
In this case, the patient initially showed white sclerosis and atrophy of the glans and was diagnosed with “viral warts” after the appearance of verrucous hyperplasia. The condition still recurred after cryotherapy. Finally, a pathological biopsy confirmed PKMB, but the long period of misdiagnosis led to the development of the disease to the stage of verrucous carcinoma. Our report shows once again that PKMB is not a benign disease and may develop into a malignant disease if not treated properly. Therefore, clinicians need to pay more attention to verrucous lesions of the glans and the collection of medical history and should consider PKMB when conventional treatments are ineffective. This case also indicates that cryotherapy may not be an appropriate treatment for PKMB, and whether cryotherapy is related to the occurrence of verrucous carcinoma needs further study.
Conclusion(s)
The purpose of this report is to remind clinicians of the cancerous potential of PKMB. It is recommended that all patients with PKMB be followed-up for a long time to monitor for malignant transformation. The progress of early detection of PKMB should be a significant guide for the choice of treatment and is closely related to the prognosis of patients.
Author Declaration:
Financial or Other Competing Interests: As declared above
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 07, 2020
Manual Googling: Oct 12, 2020
iThenticate Software: Nov 27, 2020 (7%)
[1]. Sardesai VR, Agarwal TD, Dalal AB, Mhatre MA, Pseudoepitheliomatous keratotic and micaceous balanitis with malignant transformationIndian J Sex Transm Dis AIDS 2013 34:38-40.10.4103/0253-7184.11287123919054 [Google Scholar] [CrossRef] [PubMed]
[2]. Lortat-Jacob E, Civatte J, Balanite pseudo-eÂpitheÂliomateuse keÂratosique et micaceÂeBull Soc Fr Dermatol Syphiligr 1961 68:164-67. [Google Scholar]
[3]. Child FJ, Kim BK, Ganesan R, Southern SA, Herrington CS, Calonje E, Verrucous carcinoma arising in pseudoepitheliomatous keratotic and micaceous balanitis, without evidence of human papillomavirusBr J Dermatol 2000 143:183-87.10.1046/j.1365-2133.2000.03613.x10886158 [Google Scholar] [CrossRef] [PubMed]
[4]. Kang BS, Lee SD, Park YM, Cho SY, Kang H, Is recurrent pseudoepitheliomatous keratotic balanitis related to human papillomavirus infection?Acta Derm Venereol 2010 90:208-09.10.2340/00015555-080820169317 [Google Scholar] [CrossRef] [PubMed]
[5]. Bashir SJ, Grant JW, Burrows NP, Pseudoepitheliomatous, keratotic and micaceous balanitis after penile squamous cell carcinomaClin Exp Dermatol 2010 35:749-51.10.1111/j.1365-2230.2010.03815.x20456408 [Google Scholar] [CrossRef] [PubMed]
[6]. Choo KJL, Ng SK, Sim CS, Cheng SWN, Pseudoepitheliomatous keratotic and micaceous balanitis treated with topical 5-fluorouracil and liquid nitrogenClin Exp Dermatol 2017 42:424-26.10.1111/ced.1307228406530 [Google Scholar] [CrossRef] [PubMed]
[7]. Conforti C, Toffoli L, Giuffrida R, Retrosi C, Vezzoni R, Di Meo N, An unusual presentation of genital herpes in a patient affected by lichen sclerosus et atrophicus: A case report and a combined treatment proposalDermatol Ther 2020 33:e1323910.1111/dth.13239 [Google Scholar] [CrossRef]
[8]. Proietti I, Michelini S, Skroza N, Bernardini N, Tolino E, Anzalone A, Ingenol mebutate therapy in erythroplasia of Queyrat: A new approachG Ital Dermatol Venereol 2019 10:23736 [Google Scholar]
[9]. Malkud S, Dyavannanavar V, Pseudoepitheliomatous, Keratotic and Micaceous Balanitis: A Case ReportJ Clin Diagn Res 2015 9:WD01-02.10.7860/JCDR/2015/15663.660126557598 [Google Scholar] [CrossRef] [PubMed]
[10]. Perry D, Lynch PJ, Fazel N, Pseudoepitheliomatous, keratotic, and micaceous balanitis: Case report and review of the literatureDermatol Nurs 2008 20:117-20. [Google Scholar]
[11]. Irvine C, Anderson JR, Pye RJ, Micaceous and keratotic pseudoepitheliomatous balanitis and rapidly fatal fibrosarcoma of the penis occurring in the same patientBr J Dermatol 1987 116:719-25.10.1111/j.1365-2133.1987.tb05907.x3593636 [Google Scholar] [CrossRef] [PubMed]
[12]. Pai VV, Hanumanthayya K, Naveen KN, Rao R, Dinesh U, Pseudoepitheliomatous, keratotic, and micaceous balanitis presenting as cutaneous horn in an adult maleIndian J Dermatol Venereol Leprol 2010 76:547-49.10.4103/0378-6323.6908720826996 [Google Scholar] [CrossRef] [PubMed]
[13]. Krunic AL, Djerdj K, Starcevic-Bozovic A, Kozomara MM, Martinovic NM, Vesic SA, Pseudoepitheliomatous, keratotic and micaceous balanitisCase report and review of the literatureUrol Int 1996 56:125-28.10.1159/0002828298659009 [Google Scholar] [CrossRef] [PubMed]
[14]. Murthy PS, Kanak K, Raveendra L, Reddy P, Pseudoepitheliomatous, keratotic, and micaceous balanitisIndian J Dermatol 2010 55:190-91.10.4103/0019-5154.6275320606894 [Google Scholar] [CrossRef] [PubMed]
[15]. Hanumaiah B, Mohan Lingaiah NB, Kumaraswamy SK, Vijaya B, Pseudoepitheliomatous keratotic and micaceous balanitis: A rare condition successfully treated with topical 5-FluorouracilIndian J Dermatol 2013 58(6):49210.4103/0019-5154.11997024249909 [Google Scholar] [CrossRef] [PubMed]
[16]. Zhu H, Jiang Y, Watts M, Kong F, Treatment of pseudoepitheliomatous, keratotic, and micaceous balanitis with topical photodynamic therapyInt J Dermatol 2015 54:245-47.10.1111/ijd.1250925266766 [Google Scholar] [CrossRef] [PubMed]