Transitional Cell Carcinoma in Pelvis of a Double Moiety Kidney- A Rare Presentation
Debansu Sarkar1, Bikram Haldar2, Dilip Kumar Pal3
1 Professor, Department of Urology, IPGME&R, Kolkata, West Bengal, India.
2 PDT MCH, Department of Urology, IPGME&R, Kolkata, West Bengal, India.
3 Professor, Department of Urology, IPGME&R, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dilip Kumar Pal, 244, AJC Bose Road, Kolkata-700020, West Bengal, India.
E-mail: urologyipgmer@gmail.com
Neoplasia of the renal pelvis in duplex kidneys is extremely rare, especially in complete renal ureteral duplex cases. A 46-year-old aged male patient had presented with intermittent haematuria for the last seven months. A mildly enhancing well-defined, lobulated mass arising from the pelvis of lower moiety of right kidney was found on evaluation. Confirmatory findings of a renal pelvic malignancy couldn’t be obtained. Infective condition like pyelonephritis couldn’t be excluded. To clear the diagnostic dilemma, flexible ureteroscopy was done which revealed the renal pelvic malignancy. Right lap assisted radical nephroureterectomy was done. Histopathology was suggestive of transitional cell carcinoma. The increased incidence of chronic infection, obstruction and stone formation may be instrumental in producing a higher incidence of renal pelvic tumours in patients with anomalous kidney. Diagnosing a neoplasia originating from a duplex kidney is difficult and often a multiple battery of investigations like intravenous pyelogram, ultrasonography and rigid ureteroscopy may not be useful. Considering the fact that tumour recurrence is high in the ureteric stump after local resection, a total nephroureterectomy seems to be a better treatment choice. Flexible ureteroscope might be the saviour in such doubtful clinical situations to confirm our diagnosis beyond doubt. Partial nephrectomy cannot be recommended unless long-term follow-up reports of such cases are available.
Duplex kidney, Nephroureterectomy, Renal pelvic malignancy
Case Report
A 46-year-old aged male patient presented to our Urology Department with the chief complaint of ongoing intermittent haematuria with passage of clots for the last seven months. No history of any flank pain, fever, other urinary complaints or any systemic complaints. No history of any significant weight loss. No history of any addictions. He was being managed conservatively before this visit. There was no history of relevant illness including malignancy among his family members.
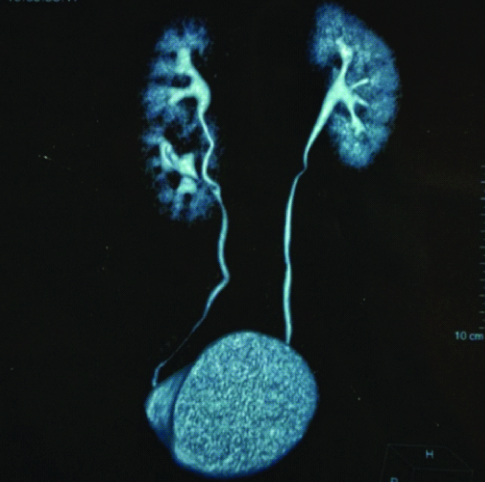
General survey was unremarkable. There were no palpable abdominal lumps. A Contrast Enhanced Computed Tomography (CECT) abdominal scan of the patient showed a malrotated enlarged right kidney with duplex moiety and partial duplication of the right ureter, joining at the level of L2 vertebrae [Table/Fig-1].
Contrast Enhanced Computed Tomography (CECT) abdominal scan of the patient showing a malrotated enlarged right kidney with duplex moiety and partial duplication of the right ureter.
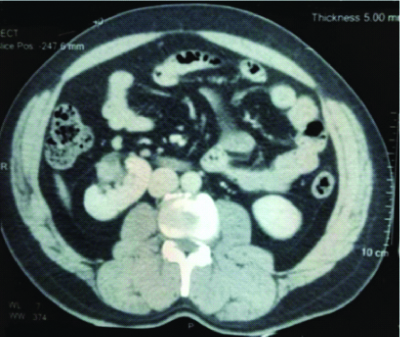
An exophytic, well-defined, lobulated Space Occupying Lesion (SOL) (2.2×1.7×2.6 cm) arising from pelvis of lower moiety of right kidney was noted [Table/Fig-2]. It was hypo-enhancing (precontrast 31HU to postcontrast 39HU) without any upstream obstruction. No malignant cells were noted in the urine cytology and cystoscopy was also unremarkable.
Contrast Enhanced Computed Tomography (CECT) abdominal scan of the patient showing an exophytic, lobulated Space Occupying Lesion (SOL) arising from pelvis of lower moiety of right kidney (L2).
The differential diagnosis on the basis of these investigations were renal pelvic malignancy or infective causes like pyelonephritis and renal abscess. Flexible ureteroscopy was done under anaesthesia which revealed two ureteric openings at the level of L2 vertebrae. Retrograde pyelogram showed the similar findings.
A solid sessile SOL was seen at the pelvis of the lower moiety without any calcification. Perilesional fluid cytology was positive for malignant cells.
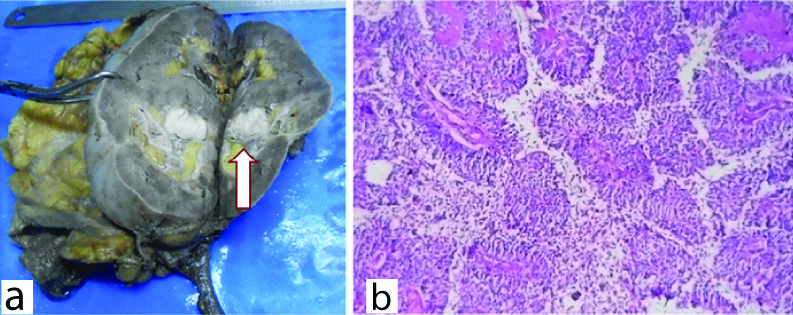
The patient was treated by laparoscopic assisted right radical nephroureterectomy with the intraoperative finding of two lower polar and three hilar renal arteries. Two renal veins were also encountered. The patient had an uneventful post-operative recovery. The histopathological features were suggestive of infiltrating transitional cell carcinoma without any surrounding tissue infiltration or lymphadenopathy [Table/Fig-3].
a) Lesion, as seen during pathological grossing of the specimen; b) Histopathological features were suggestive of infiltrating transitional cell carcinoma (H&E stain, X100).
As the tumour was localised in nature so, adjuvant therapy was not needed for this case. No significant issues were noted during follow-up at three months, six months and at the end of one year.
Discussion
Primary tumours of the renal pelvis and collecting system are not seen frequently when compared to tumours of the renal parenchyma. Duplication of the renal pelvis and ureter although a common anomaly of the renal collecting system yet they are seen in about one in 150 autopsies [1,2].
Mostly patients with congenital malformations remain asymptomatic. Few among them often presents with complications due to prolonged urinary stasis and obstructive uropathy. This can lead to infections, calculi formation and even malignancy [3,4].
Various reports have suggested that due to such chronic stasis of urine there is an increased incidence of renal pelvic malignancy among the patients with horseshoe kidneys [5,6].
Presently, the aetiology for the development of renal pelvic neoplasm is not defined and prolonged stasis and smoking might be instrumental for the same [6-8].
Duplication is associated with various anatomical variations and therefore, confirming the diagnosis of a tumour in a duplex system is quite difficult. First line investigations like Ultrasonography and CECT scans may not be able to confirm the diagnosis of a renal pelvic malignancy in duplex systems as the other differential diagnosis of such cases might present with a similar picture [7,9]. The differential diagnosis includes renal parenchymal malignancies, complex cystic diseases of kidney, infective conditions of kidney like pyelonephritis and renal abscess [6,7]. As per the recommendations of European Association of Urology (EAU) guidelines flexible ureteroscopy helps to visualise the SOL and confirm the diagnosis before proceeding with radical surgery in these cases. Biopsy of the tumour tissue or fluid cytology aids in the diagnosis [8,10].
Multiple artery and veins might be encountered while operating on a patient with duplex kidney, so a pre-operative CT Angiogram would provide an additional boost to plan surgery in such cases [11].
Malignancy in renal pelvis should ideally be treated by radical nephroureterectomy with excision of the bladder cuff. Hemi-nephrectomy has often been advocated by some [5,7,12].
But a long-term follow-up study of such cases is not available. Ideally, the whole renaduplex units and bladder cuff or ectopic orifice should be excised radically, because the upper and lower moiety of duplex renal systems has common vessel traffic branches and the two ureters have the same origin. Cases of recurrence in the retained ureteric stump have also been reported [7,9].
A hemi-nephroureterectomy may be considered only in cases of complete duplication or when the opposite side kidney is non-functioning [11]. Hemi-nephrectomy may also damage the integrity of the collecting system and can lead to cancer cell implantation [7].
For localised Upper Tract Urothelial Carcinoma (UTUC) Radical Nephroureterectomy is the definite treatment and adjuvant therapy is not required. The follow-up is done as per the EAU guidelines for UTUC [13].
Conclusion(s)
For the patients who have a renal duplex system a regular follow-up is often necessary especially when there is evidence of stasis or any complications. Diagnosis of a malignancy in patients with duplex system is difficult and often the first line imaging methods may fail to provide a confirmation of the same. Planning a management in such cases are individualised and a radical nephroureterectomy is the best treatment based on the current literature. Long-term follow-up reports of such cases are necessary to develop any new recommendations in management of such patients.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 27, 2020
Manual Googling: Oct 13, 2020
iThenticate Software: Nov 27, 2020 (18%)
[1]. Ho DS, Jerkins GR, Williams M, Noe HN, Ureteropelvic junction obstruction in upper and lower moiety of duplex renal systemsUrology 1995 45:503-06.10.1016/S0090-4295(99)80023-5 [Google Scholar] [CrossRef]
[2]. Chen GM, Chen SW, Xia D, Li J, Yan S, Jin BY, Sarcomatoid carcinoma of the renal pelvis in duplex kidneyChin Med J (Engl) 2011 124:2074-76. [Google Scholar]
[3]. Wah TM, Weston MJ, Irving HC, Lower moiety pelvic-ureteric junction obstruction (PUJO) of the duplex kidney presenting with pyonephrosis in adultsBr J Radiol 2003 76:909-12.10.1259/bjr/5614878314711780 [Google Scholar] [CrossRef] [PubMed]
[4]. Natarajan G, Jeyachandran D, Subramaniyan B, Thanigachalam D, Rajagopalan A, Congenital anomalies of kidney and hand: A reviewClin Kidney J 2013 6:144-49.10.1093/ckj/sfs18626019842 [Google Scholar] [CrossRef] [PubMed]
[5]. Ujike T, Noda Y, Oka D, Takada S, Fujimoto N, Koide T, Squamous cell carcinoma of the renal pelvis with giant hydronephrosisHinyokika Kiyo 2003 49:757-59. [Google Scholar]
[6]. Mizusawa H, Komiyama I, Ueno Y, Maejima T, Kato H, Squamous cell carcinoma in the renal pelvis of a horseshoe kidneyInt J Urol 2004 11:782-84.10.1111/j.1442-2042.2004.00873.x15379945 [Google Scholar] [CrossRef] [PubMed]
[7]. Zhang Y, Yu Q, Zhang Z, Liu R, Xu Y, Renal pelvis urothelial carcinoma of the upper moiety in complete right renal duplex: A case reportInt J Clin Exp Pathol 2015 8:15422-25. [Google Scholar]
[8]. Rao DS, Krigman HR, Walther PJ, Enteric type adenocarcinoma of the upper tract urothelium associated with ectopic ureter and renal dysplasia: An oncological rationale for complete extirpation of this aberrant developmental anomalyJ Urol 1996 156:1272-74.10.1016/S0022-5347(01)65567-8 [Google Scholar] [CrossRef]
[9]. Karray O, Khouni H, Charfi M, Boulma R, Ureteral tumor in an ectopic duplex system: A case reportJ Med Case Rep 2019 13:7010.1186/s13256-019-1974-230845986 [Google Scholar] [CrossRef] [PubMed]
[10]. Crouzet S, Berger A, Monga M, Desai M, Ureteroscopic management of upper tract transitional cell carcinoma and ureteropelvic obstructionIndian J Urol 2008 24:526-31.10.4103/0970-1591.4426219468512 [Google Scholar] [CrossRef] [PubMed]
[11]. Khan A, Myatt A, Palit V, Biyani CS, Laparoscopic heminephrectomy of a horseshoe kidneyUrol D JSLS 2011 15:415-20.10.4293/108680811X1312573335651221985738 [Google Scholar] [CrossRef] [PubMed]
[12]. Liu GM, Ma HS, Li YM, Multilocular cystic renal cell carcinoma in lower pole moiety of a duplex kidneyInt J Surg Pathol 2012 20:613-17.10.1177/106689691243809822456872 [Google Scholar] [CrossRef] [PubMed]
[13]. Kim HS, Lee JS, Jeong CW, Kwak C, Kim HH, Adjuvant chemotherapy for locally advanced upper tract urothelial carcinoma: Updated results of the Seoul National university hospital experienceInt Braz J Urol 2015 41:1067-79.10.1590/S1677-5538.IBJU.2015.000926742963 [Google Scholar] [CrossRef] [PubMed]