Aetiology behind unilateral proptosis can run from benign to life-threatening condition. Carotico Cavernous Sinus Fistula (CCF) is abnormal communication between Internal Carotid Artery (ICA) alone or its branches and cavernous sinus. This was a case of a 32-year-old female presented with unilateral proptosis, diminution of vision in right eye, diplopia and unilateral headache towards right side. On ocular examination, right eye had pulsating proptosis, severe chemosis, relative afferent papillary defect, restricted ocular movements in all gazes and left eye was normal. There was no history of trauma, hypertension, diabetes mellitus, cardiovascular abnormality. Common causes of unilateral proptosis are carotid cavernous sinus fistula, orbital pseudotumour, orbital cellulitis, cavernous sinus thrombosis, or intraorbital neoplasms. Radiological investigations like Computed Tomography (CT)/Magnetic Resonance Imaging (MRI) imaging and CT/MR Angiography (MRA) is necessary to rule out the cause for proptosis. Patient presented to Ophthalmology Outpatient Department (OPD) with concern of reduced vision, redness and proptosis. Hence, MRA was advised to this patient which was suggestive of right ICA- cavernous sinus fistula. Cavernous sinus fistula can be traumatic or spontaneous and delay in diagnosis may lead to poor visual outcome.
Case Report
A 32-year-old female patient presented to Ophthalmology Outpatient Department for protrusion of right eye, redness, swelling and diminution of vision along with diplopia since two months. Patient also complained of pain in right eye with restriction of movements and right sided headache since two months. Patient symptoms were insidious in onset and progressed gradually over two months. There was no history of trauma in past month, hypertension or any cardiovascular disorder.
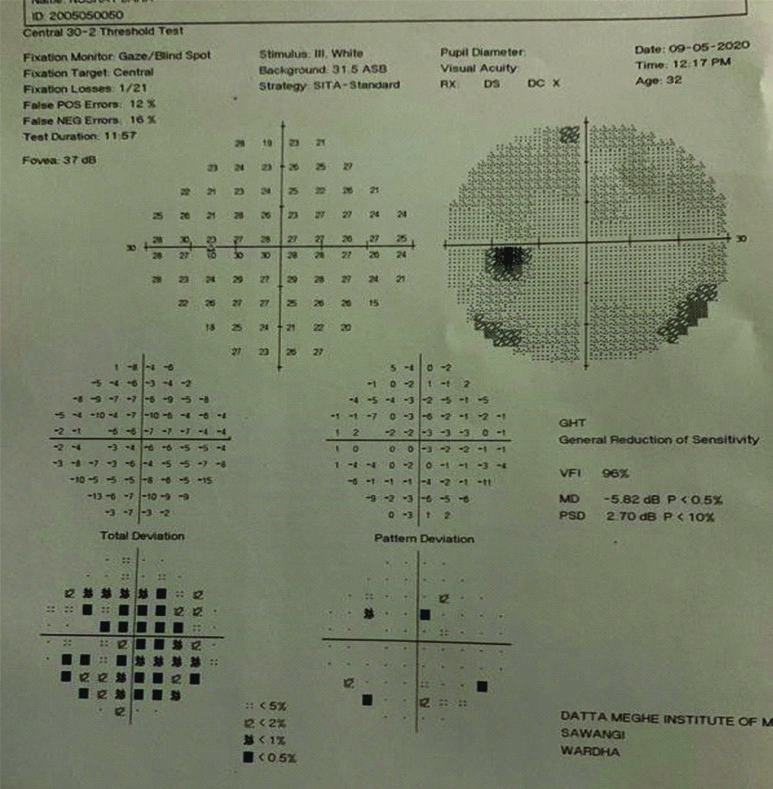
The Best Corrected Visual Acuity (BCVA), right eye was 2/60 and left eye 6/6. On slit-lamp biomicroscopic examinatison, right eye had upper lid oedema, lagophthalmos, severe haemorrhgic chemosis and conjunctival congestion with keratinisation. Cornea showed exposure keratopathy inferiorly due to lagophthalmos. Relative afferent papillary defect was present. Intraocular pressure could not be assessed on applanation but digitally felt normal. On examination of proptosis, unilateral pulsatile proptosis was seen, shape and surface was irregular, margins ill-defined, consistency was firm and bruit was present on auscultation [Table/Fig-1].
Clinical picture showing proptosis right side, with chemosis and conjunctival keratinisation with extraocular movements restricted in all gaze.

Left eye was normal, ocular movements full and free in all gazes with IOP 16 mmHg on applanation tonometry. Patient perimetry (30-2) was done in left eye which showed normal visual field [Table/Fig-2]. Right eye perimetry could not be performed due to proptosis and chemosis.
Showing left eye visual field appears normal.
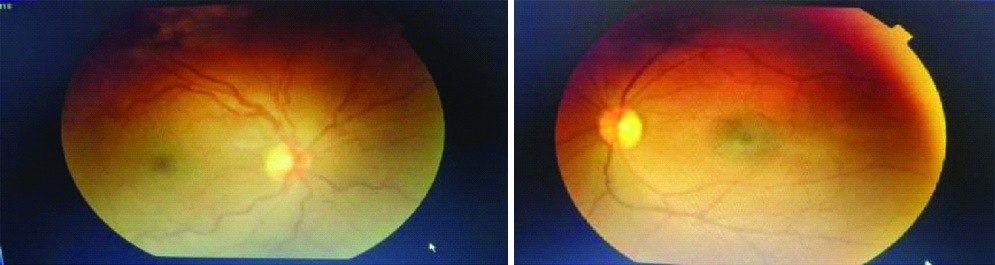
Fundus examination in right eye, disc was normal, no hyperemia or oedema, blood vessel showed tortousity, macula and periphery were normal. In left eye no abnormality was detected [Table/Fig-3].
Right eye fundus; Tortuous blood vessels. Left eye fundus; Normal.
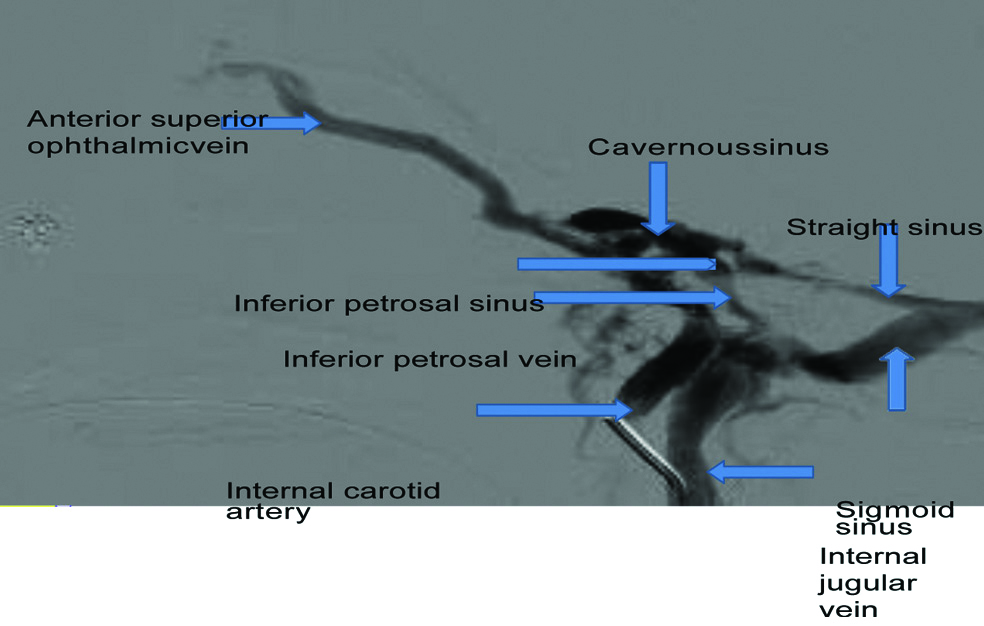
Patient was advised MRI with MRA and venography, which showed no abnormality in brain parenchyma, but MRA non-contrast showed, abnormal prominent tortuous vessels showing normal flow voids in the region of right cavernous sinus with the cavernous portion of intracranial right carotid artery not visualised separately, enlarged cavernous sinus with bulky right extraocular muscle. There was evidence of flow related signal in right cavernous sinus, right superior ophthalmic vein and adjacent right periorbital veins showing anastomosis with right superior ophthalmic vein in angiography phase. Features were suggestive of right ICA cavernous sinus fistula probably due to ruptured aneurysm. DSA through ICA injection showed [Table/Fig-4], contrast opacification, all venous communication anteriorly- anterior superior ophthalmic vein and posteriorly-inferior petrosal vein and sinus are filled when dye is injected through ICA.
Showing contrast opacification in all the venous communication.
Patient laboratory investigations were sent- complete blood count, liver function test, kidney function test, peripheral smear, coagulation profile, thyroid profile, all were within normal limit.
Patient informed consent was taken and patient was thoroughly explained regarding the procedure.
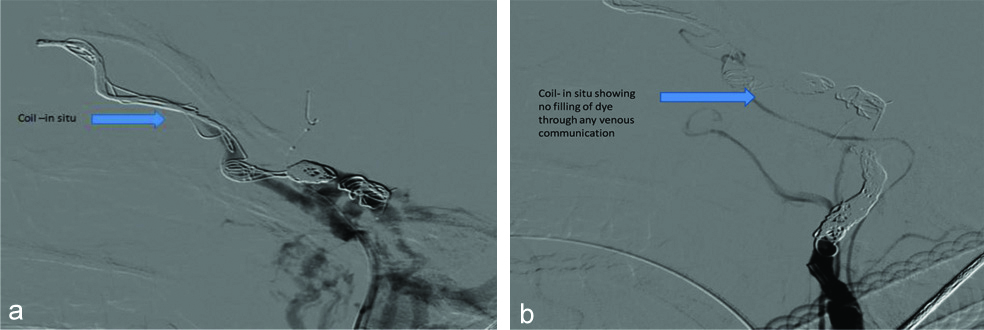
Patient underwent coiling of fistula [Table/Fig-5a] as an interventional procedure, done in our Radiology Department under all aseptic precautions. In [Table/Fig-5b] it is showing that after coiling filling is not seen in all the connections of cavernous sinus that was filling anteriorly through superior ophthalmic vein and posteriorly through inferior petrosal vein which was seen earlier.
a) Showing coil in-situ; b) Coil in-situ with no filling of vessels.
Patient had hospital stay for one week post-procedure. And during hospital stay patient was given tablet aceclofenac plus serrratiopeptidase two times a day for seven days and tablet pantoprazole once a day for seven days and topical antibiotic eyedrop moxifloxacin twice a day for 10 days. Patient was discharged on similar medications. After discharge, patient was advised regular follow-up. Post-procedure patient followed-up after one month which showed complete resolution of redness, chemosis and proptosis [Table/Fig-6]. However, restricted movements persisted. There was marginal improvement in visual acuity of 6/60.
Follow-up after one month.

Discussion
Proptosis can be due to pathology in orbit or intracranial space. It can be acute or with varying degrees of chronicity and associated with significant visual loss [1].
Aetiology behind unilateral proptosis can run from benign to life-threatening condition [1]. Congestive Cardiac Failure (CCF) is abnormal communication between ICA alone or its branches and cavernous sinus [2]. Trauma is the most common cause (70-90%) that leads to CCF from basal skull fracture [3]. Other causes include spontaneous rupture of an existing aneurysm or atherosclerotic ICA seen in postmenopausal and hypertensive females, Ehlers-Danhlos syndrome type IV, or iatrogenic causes including transarterial endovascular intervention, internal carotid endarterectomy, percutaneous treatment for trigeminal neuralgia, trans-sphenoidal resection of a pituitary tumour, and maxillofacial surgery [4].
Anatomically, they can be direct or indirect with high flow or low flow. According to Barrows classification, cavernous sinus fistula is divided into four subtypes. Type A- direct communication between ICA and cavernous sinus, Type B- communication between dural ICA branches and cavernous sinus, Type C- communication between dural external carotid artery branch and cavernous sinus, Type D- communication from dural branches of ICA and external carotid artery branches to cavernous sinus [5]. Type D-accounts for 71% of cases. CCF is common in western countries [6].
Direct fistulas are usually seen following blunt trauma or basal skull fracture (70-90%) resulting from tear in ICA within cavernous sinus.
However, in this case there was no history of direct trauma so likely, cause could be due to spontaneous rupture of aneurysm in young patient making it an unusual case [7].
Direct and indirect CCFs produce classic triad of proptosis, conjunctival chemosis and cranial bruit but can masquerade as chronic conjunctivitis. Third cranial nerve and the anterior visual pathways can be compressed by the unruptured aneurysm. Ruptured aneurysms and subarachnoid haemorrhage can result in Terson syndrome [8] and papilloedema. Arteriovenous malformations with or without haemorrhage, may compress portions of the retrochiasmal pathways causing visual field defect.
Clinical manifestation depend on whether the lesion is high or low flow which includes proptosis which can be pulsatile, chemosis due to episcleral venous congestion, striabismus due to third cranial nerve involvement, ocular bruit [2]. In present case, she had unilateral pulsatile proptosis, severe chemosis and audible bruit.
To diagnose carotid cavernous fistula, diagnostic modality requires neuroimaging such as non-invasive Computed Tomographic Angiography (CTA) or Magnetic Resonance Angiography (MRA) or Digital Substraction Angiograpy (DSA). These modalities can diagnose both direct and dural fistula which causes visual manifestations. In our patient, MRA and DSA both were performed. DSA is the gold standard for classification and diagnosis of carotid cavernous fistula. It is used for both diagnostic and therapeutic purpose [7].
Chances of spontaneous closure of dural fistula becomes a greater risk after diagnostic angiography, normally spontaneous closure of the same is highly unlikely. DSA for this patient showed, opacification of cavernous sinus and ophthalmic vein and all connection of cavernous sinus were filling anteriorly as well as posteriorly through inferior petrosal vein.
Neurosurgical intervention is often required for such cases such as ligation of external and ICA or embolisation of fistula which can be done by glues, detachable balloons or thermogenic micrcoils [3].
There were very limited options in the past for treatment which includes, ligating the cervical carotid artery proximal to the fistula and intracranial ICA distal to the fistula or occlusion of common crotid artery or ICA thus, trapping the fistula. But such interventions could lead to cerebral ischaemic event due to low induced flow or embolic event [9].
These procedures are obsolete as endovascular interventional techniques took a leap because of 90-100% cure rate and low rate of complications and also ICA can be preserved [10]. A transarterial approach via the ICA is most commonly used. Embolic material of choice that are used includes detachable balloons, coils, n-butyl cyanoacrylate (acrylic glue). Detachable balloons are most commonly used. Flow directing stent are also used, though postoperatively, antiplatelet therapy is required [11].
Our patient underwent, endovascular coiling after knowing the exact location of fistula through DSA.
Minor complications of these procedures include haematoma, facial pain, and ocular motor nerve palsies seen in 1-30% of cases [12]. In our patient, no such complications were observed.
There can be arterial and venous stasis causing decreased retinal and ocular perfusion, venous dilatation, retinal haemorrhage, central retinal vein occlusion and artery occlusion with cotton wool patches and serous retinal detachment as a sequelae [12].
Patient presented to us after two months of symptoms, so the intervention was late. Though there was anatomical restoration that is decrease proptosis and chemosis post intervention but patient persisted with ophthalmoplegia and had marginal visual improvement.
Conclusion(s)
Congestive Cardiac Failure needs early interventions because of various ocular complications like glaucoma due to raised episcleral pressure, iris neovascularisation and retinal ischemia.
[1]. Nambiar KR, Ajith PS, Arjunan A, Unilateral proptosis as the initial manifestation of malignancyJ Egypt Natl Canc Inst 2017 29(3):159-61.10.1016/j.jnci.2017.05.00428673746 [Google Scholar] [CrossRef] [PubMed]
[2]. Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT, Classification and treatment of spontaneous carotid-cavernous sinus fistulasJ Neurosurg 1985 62(2):248-56.10.3171/jns.1985.62.2.02483968564 [Google Scholar] [CrossRef] [PubMed]
[3]. Miller NR, Diagnosis and management of dural carotid-cavernous sinus fistulasNeurosurg Focus 2007 23(5):E1310.1097/ito.0b013e31815da672 [Google Scholar] [CrossRef]
[4]. Kashiwagi S, Tsuchida E, Goto K, Shiroyama Y, Yamashita T, Takahasi M, Balloon occlusion of a spontaneous carotid-cavernous fistula in Ehlers-Danlos syndrome type IVSurg Neurol 1993 39(3):187-90.10.1016/0090-3019(93)90180-9 [Google Scholar] [CrossRef]
[5]. Houser OW, Campbell JK, Campbell RJ, Sundt TM Jr, Arteriovenous malformation affecting the transverse dural venous sinus-An acquired lesionJrMayo Clin Proc 1979 54(10):651-61. [Google Scholar]
[6]. Chaudhry IA, Elkhamry SM, Al-Rashed W, Bosley TM, Carotid cavernous fistula: Ophthalmological implicationsMiddle East Afr J Ophthalmol 2009 16(2):57-63.10.4103/0974-9233.5386220142962 [Google Scholar] [CrossRef] [PubMed]
[7]. de Keizer R, Carotid-cavernous and orbital arteriovenous fistulas: Ocular features, diagnostic and hemodynamic considerations in relation to visual impairment and morbidityOrbit 2003 22(2):121-42.10.1076/orbi.22.2.121.1431512789591 [Google Scholar] [CrossRef] [PubMed]
[8]. Robert T, Sylvestre P, Blanc R, Botta D, Ciccio G, Smajda S, Thrombosis of venous outflows of the cavernous sinus: Possible aetiology of the cortical venous reflux in case of indirect carotid-cavernous fistulasActa Neurochir (Wien) 2017 159(5):835-43.10.1007/s00701-017-3079-228111701 [Google Scholar] [CrossRef] [PubMed]
[9]. Gemmete JJ, Ansari SA, Gandhi D, Endovascular treatment of carotid cavernous fistulasNeuroimaging Clin N Am 2009 19(2):241-55.Table of Contents10.1016/j.nic.2009.01.00619442908 [Google Scholar] [CrossRef] [PubMed]
[10]. Lewis AI, Tomsick TA, Tew JM, Management of 100 consecutive direct carotid-cavernous fistulas: Results of treatment with detachable balloonsJr Neurosurgery 1995 36(2):239-44.discussion 244-510.1097/00006123-199502000-00001 [Google Scholar] [CrossRef]
[11]. Debrun GM, Viñuela F, Fox AJ, Davis KR, Ahn HS, Indications for treatment and classification of 132 carotid-cavernousNeurosurgery 1988 22(2):285-89.10.1227/00006123-198802000-000013352876 [Google Scholar] [CrossRef] [PubMed]
[12]. Berk AT, Ada E, Kir E, Saatci AO, Choroidal detachment associated with direct spontaneous carotid-cavernous sinus fistulaOphthalmologica 1997 211(1):53-55.10.1159/0003108758958533 [Google Scholar] [CrossRef] [PubMed]