Acute IWMI with RVMI has difficult management issues. In MI of LV myocardium, additional RV involvement becomes an independent risk factor for increased mortality [1,2].
Right Ventricular Myocardial Infarction is present in approximately 50% cases of acute IWMI [3]. Complications of an RVMI include low cardiac output state with hypotension, decreased heart rate and right heart failure. ST segment elevation in lead III more than lead II, in standard 12-lead Electrocardiogram (ECG), is characteristic for an RVMI [4]. ST-elevation in lead V4R more than 1.0 mm is a reliable marker of an RV infarction, with 100% sensitivity and 87% specificity [5]. Hence, involvement of RV in all acute IWMI should be carefully looked at in 12-lead standard ECG along with additional right-sided leads. Signs of significant haemodynamic effects of RV ischaemia include a tricuspid regurgitation murmur; pulsus paradoxus and Kussmaul’s sign [6].
Ventricular myocardium produces BNP in response to wall stress due to volume or pressure overload. BNP decreases right atrial pressure, systemic vascular resistance, aldosterone secretion and decreases sympathetic stimulation and cell hypertrophy, while increasing sodium excretion [7]. Raised BNP level was a poor prognostic factor in patients with first episode of AMI who underwent angioplasty and in patients presenting with heart failure [8]. Trop I levels and CK-MB levels are independent markers of extent of myocardial damage or necrosis [9,10].
This study aimed to evaluate the relationship of RV involvement with the help of routine echocardiography and Doppler techniques with the commercially available cardiac triage markers (Trop I, BNP, CK-MB) in acute IWMI, with or without associated RVMI, and their consequences in the outcomes (in hospital) in these patients.
Materials and Methods
This was a cross-sectional study in compliance with the ethical principles in accordance of the Declaration of Helsinki and informed consent was taken from all the study participants. The study was undertaken at ABVIMS (F.No. 18/2018/IEC/ABVIMS/RMLH 1886) and Dr. Ram Manohar hospital, Cardiology Department, New Delhi. Patients were enrolled from September, 2018 to August, 2019. Sample size using Cochran’s formula was 285, with a 95% confidence interval.
A total of 735 acute ST elevation MI patients presented to the institute, which is a tertiary care centre in Northern India having round the clock primary angioplasty facility, out of which 314 had an acute IWMI, with or without RV involvement, with or without a normal sinus rhythm and a heart rate ranging from 30 to 140 minutes.
Patients having prior MI, prior re-vascularisation, valvular heart disease, pulmonary hypertension, pericardial disease and chronic kidney disease were excluded from the study. Twenty patients were excluded because of prior MI, on the basis of presence of pathological Q-waves in anterior leads, not explained by the acute IWMI with or without RVMI and valvular heart disease (mitral regurgitation).
A total of 294 patients were divided into two study groups, on the basis of presence or absence of RV involvement in the form of RVMI, as determined by ECG and/or echo (echocardiogram) findings [Table/Fig-1].
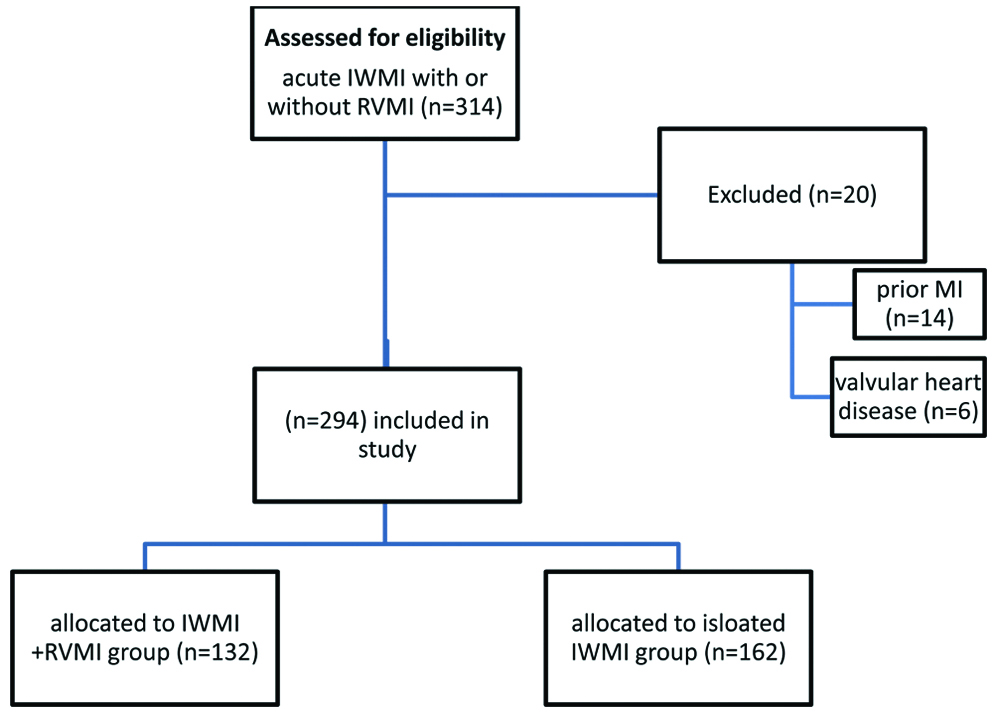
Thus, there were 162 patients with isolated acute IWMI (120 males and 62 females), and 132 patients with RV involvement (98 males and 34 females). All patients were pre-medicated with standard loading doses of dual antiplatelet therapy and a statin and were transferred to catheterisation laboratory for primary angioplasty.
The diagnostic criteria for MI used was: acute onset ischaemic chest pain with the standard electrocardiogram diagnostic criteria for IWMI. ST elevation of 1 mm in at least two of the three inferior leads (II, III, and aVF); in lead V4R, an ST-segment elevation of more than 1 mm was used as criteria for diagnosing RVMI, in those patients that satisfied the criteria for an IWMI [9]. Right-sided chest leads were taken in all patients for detecting RV involvement. In doubtful cases, additional help in the form of change in troponin levels above the 99 percentile with ischaemic symptoms, echocardiogram for regional wall motion abnormality or angiography for detection of intracoronary thrombus were used [10]. Blood sampling was done immediately after presentation to the emergency. Serum BNP levels, Trop I, and CK-MB levels were detected by an immunoassay panel using Cardiac Markers Triage Meter Pro (Alere Medical, USA). BNP value of >100 pg/mL was the cut-off. The normal values were 0.00-0.02 ng/mL for Trop I and 0.0-4.3 ng/mL for CK-MB [11].
The patients were evaluated by 2D Echocardiography (Echo) within first 12 hours after admission. ECG-gated Echo evaluation was performed from parasternal long axis, parasternal short axis, apical four chambers, and subcostal views using Philips HD11XE machine (Philips Corp. USA). All patients underwent M-mode, pulse-wave, continuous-wave, colour Doppler, and tissue Doppler assessment and the average of three consecutive measurements were taken.
Teicholz method/formula was used to assess Left Ventricular Ejection Fraction (LVEF) and parasternal short axis was used to evaluate wall motion abnormalities. Modified Simpson’s method was used to assess biplane ejection fraction in apical four and two chamber views [12]. Diastolic function was assessed by pulse wave and tissue Doppler. Systolic function of right ventricle was assessed by TAPSE, Right Ventricle Fractional Area Change (RVFAC), and RV systolic wave (RSm) and global function was assessed by Right Ventricle Myocardial Performance Index (RVMPI). Comparison was done first between patients with and without RV involvement during their hospital stay, followed by comparison among groups for quantitative parameters, especially biomarkers, for finding correlation between biomarker levels and echocardiographic parameters (both RV and LV functions).
Statistical Analysis
Statistical analysis was performed using SPSS statistical package, version 25.0 (SPSS, Chicago, IL, USA). Independent groups t-test was used for intergroup comparisons with a normal distribution, and Mann-Whitney U test in those without. To analyse the relationship between variables, Pearson’s correlations were used. For qualitative data, comparison of proportion test was used to calculate p-values. Descriptive statistics were shown as arithmetic mean±standard deviation. A p-value <0.05 was taken statistically significant for all statistical analysis.
Results
During the 12 months study period, 294 patients of acute IWMI were included for analysis. Of these, 132 (44.9%) had acute inferior MI with RV involvement (mean age, 59.48±11.46 years) and 162 (55.1%) did not have involvement of RV (mean age, 61.06±11.83 years). Two hundred and eighteen (74.2%) were males, and 76 (25.8%) were females. The mean stay of patients (in hospital) in the isolated IWMI group was 3.2±0.56 days as compared to 4.3±0.88 days in the group with RV involvement. Significant difference was found only in the window period from time of onset of pain to primary angioplasty [Table/Fig-2].
Baseline characteristics.
| Parameter | IWMI+RVMI (n=132) | Isolated IWMI (n=162) | p-value |
|---|
| Age | 62.32±10.31 | 61.11±11.1 | 0.3380@ |
| Sex F/M | 34/98 | 62/120 | 0.751/0.973# |
| Smoking, n (%) | 68 (51.5) | 81 (50.0) | 0.798# |
| H/o HTN, n (%) | 53 (40.1) | 68 (41.9) | 0.755# |
| DM, n (%) | 21 (15.9) | 16 (9.9) | 0.123# |
| Family history, n (%) | 46 (34.8) | 65 (40.1) | 0.351# |
| SBP, mm Hg | 118.08±34.25 | 120.42±20.12 | 0.4666@ |
| DBP, mm Hg | 76.50±20.22 | 80.46±15.56 | 0.058@ |
| HR/min | 65.32±15.65 | 71.56±12.43 | 0.203@ |
| Window period in hours | 9.32±2.43 | 6.57±3.41 | 0.0365@* |
Data are shown as mean±standard deviation or number (%). HTN: Hypertension; DM: Diabetes mellitus; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; HR: Heart rate; RVMI: Right ventricular myocardial infarction; IWMI: Inferior wall myocardial infarction. @independent t-test, #Comparison of proportion test *Significant at p<0.05
BNP and Troponin I levels were significantly higher in patients with IWMI with involvement of RV as shown in [Table/Fig-2]. In Echocardiographic variables, there was significant difference in E/E’ ratio, which is a marker of diastolic dysfunction; TAPSE and RVFAC were significantly lower in IWMI +RVMI patients. Details are described in [Table/Fig-3,4,5].
| Parameter | IWMI+RVMI (n=132) | Isolated IWMI (n=162) | p-value |
|---|
| BNP pg/mL | 390.48±300.53 | 368.32±290.54 | 0.0432@* |
| Trop I ng/mL | 8.24±5.13 | 6.21±3.40 | 0.0378@* |
| CK-MB ng/mL | 10.56±3.21 | 9.11±2.86 | 0.1452@ |
Data are shown as median±standard deviation. BNP: Brain natriuretic peptide; RVMI: Right ventricular myocardial infarction; Trop I: Troponin I; CK-MB: Creatine kinase muscle brain; RVMI: Right ventricular myocardial infarction; IWMI: Inferior myocardial infarction. @independent t test, #Comparison of proportion test *Significant at p<0.05
Left Ventricular (LV) echocardiographic parameters.
| Parameter | IWMI+RVMI (n=132) | Isolated IWMI (n=162) | p-value |
|---|
| LVEDD mm | 45.64±4.53 | 44.87±4.44 | 0.1438@ |
| LVESD mm | 32.43±4.50 | 32.57±3.82 | 0.1675@ |
| LA mm | 36.54±4.12 | 35.79±4.25 | 0.1281@ |
| LVEF% | 45.06±5.05 | 44.12±6.42 | 0.2650@ |
| E/A ratio | 1.20±0.54 | 0.98±0.34 | 0.1982@ |
| E/E’ ratio | 13.45±6.2 | 11.51±4.50 | 0.0154@* |
Data are shown as mean±standard deviation, LVEDD: Left ventricular end-diastolic diameter; LVESD: Left ventricular end-systolic diameter; LA: Left atrium; LVEF: Left ventricular ejection fraction; E/A ratio: Ratio of early to late diastolic filling; E/E’: Ratio of early filling velocity to tissue Doppler early filling velocity; RVMI: Right ventricular myocardial infarction; IWMI: Inferior myocardial infarction. @independent t-test *Significant at p<0.05
Right Ventricular (RV) echocardiographic parameters.
| Parameter | IWMI+RVMI (n=132) | Isolated IWMI (n=162) | p-value |
|---|
| TAPSE | 18.32±1.32 | 20.31±2.23 | 0.0305@* |
| RSm | 10.83±1.21 | 11.42±1.86 | 0.1697@ |
| RVFAC% | 45.37±8.88 | 49.52±6.62 | 0.0261@* |
| RVMPI | 0.56±0.15 | 0.59±0.12 | 0.2872@ |
Data are shown as mean±standard deviation, TAPSE: Tricuspid annular plane systolic excursion; RSm: Right ventricular systolic wave; RVFAC: Right ventricle fractional area change; RVMI: Right ventricular myocardial infarction; RVMPI: Right ventricular myocardial performance index; RVMI: Right ventricular myocardial infarction; IWMI: Inferior myocardial infarction. @independent t-test, *Significant at p<0.05
Significant positive correlation was found between BNP levels of more than 400 pg/mL, Troponin I, CK-MB and E/E’ ratio. Significant negative correlation was found between BNP levels more than 400 pg/mL and LVEF, TAPSE and RSm and between Trop I and TAPSE. Details are shown in [Table/Fig-6].
Correlation between BNP, Trop I, CK-MB and echocardiographic parameters.
| Biomarkers | Echo parameter | Correlation level | p-value |
|---|
| BNP ≤400 | LVEF | -0.323 | 0.032 |
| E/E’ ratio | +0.333 | 0.020 |
| RVFAC % | -0.421 | 0.080 |
| TAPSE | -0.387 | 0.040 |
| RSm | -0.321 | 0.033 |
| LA mm | +0.322 | 0.401 |
| Trop I | LVEF | -0.521 | 0.423 |
| E/E’ ratio | +0.342 | 0.036 |
| TAPSE | -0.466 | 0.028 |
| CK-MB | E/E’ ratio | +0.432 | 0.044 |
| TAPSE | -0.311 | 0.089 |
Correlation level using Pearson’s correlation analysis. Significant at p<0.05
Complications were higher in the patients with IWMI, with RVMI than with isolated IWMI with death occurring in 6 (4.5%) cases in IWMI+RVMI group and 3 (1.86%) in isolated IWMI group. Arrhythmia in the form of high degree AV block, ventricular fibrillation and ventricular tachycardia was more in the IWMI+RVMI group, as well as higher incidence of acute kidney injury as shown in [Table/Fig-7].
| Parameter | | IWMI+RVMI (n=132) | Isolated IWMI (n=162) | p-value |
|---|
| Death (in-hospital mortality) | Cardiogenic | 3 | 1 | 0.048# |
| Non cardiogenic | 3 | 2 | 0.836# |
| Arrhythmias | 32 | 22 | 0.019# |
| Acute kidney injury | 34 | 12 | 0.024# |
| Bleeding | 14 | 12 | 0.337# |
RVMI: Right ventricular myocardial infarction; IWMI: Inferior myocardial infarction. #Comparison of proportion test. Significant at p<0.05
Discussion
This study demonstrated that patients of IWMI with RVMI had lower TAPSE and RVFAC. The incidence of acute IWMI with RVMI was found to be 10% to 50% in previous studies [13,14]. In this study, 45% patients had IWMI with RVMI and 55% had isolated IWMI, but it excluded prior MI and late presentations. A previous study had found 32% cases with IWMI and RVMI vs 68% with isolated IWMI [15]. The present study study found more hypotension in patients with RVMI than isolated IWMI, but it was not statistically significant, may be due to early initiation of fluids in the RVMI group unlike a previous study [15]. Patients presenting with RVMI had statistically significant longer window period for primary angioplasty, which may be accounted by the same reason of starting intravenous fluids in such patients prior to shifting to cathlab.
Ventricles secrete BNP in situations of increase volume and pressure load, it rises in two to four hours and stabilises in 24 hours after onset of ischaemic symptoms [7]. BNP levels were higher in patients presenting with IWMI with RVMI than in patients with isolated IWMI, similar to a finding demonstrated previously [16].
There was no statistical difference between LV echocardiographic parameters between the two groups except for E/E’ ratio, which is a marker of diastolic dysfunction and which was higher in the RVMI group. This can be explained by the reverse Bernheim’s effect, as such patients were given liberal intravenous fluids during their management.
Trop I and BNP levels were significantly higher in patients with RV dysfunction compared to IWMI alone, CK-MB levels were also raised, but did not reach statistical significance. Similar prognostic value of Trop I and BNP have been demonstrated in MI and unstable angina pectoris in previous studies [17-19]. There was a negative correlation with LVEF <45% and BNP levels in a study [20] while another showed higher BNP levels in RVEF <40% compared to RVEF >40% [21]. This study found a similar correlation between LVEF and BNP levels, in addition it founded lower TAPSE and RVFAC%, but RSM values did not reach statistical significance between the two groups. This study found positive correlations between BNP, Trop I, and CK-MB levels with E/E’ ratio. Another study showed a positive correlation between mitral inflow (E and A waves) and BNP levels [22]. Similar correlation between diastolic dysfunction with N-terminal pro-BNP (NT-proBNP) were shown previously [23].
No significant difference between RVMPI was found between the two groups in this study unlike the study by Nagaya N and colleagues [24], which found a relationship between BNP levels and RV functions, which may be attributed to pulmonary hypertension which was present in that study unlike the present study.
There was a negative correlation between BNP levels, LVEF and TAPSE, with BNP >400 pg/mL in this study, similar to a study done in 2014 [25].
There was a higher incidence of death, arrythmias and acute kidney injury, even after primary angioplasty in the RVMI group confirming the higher complication rate and mortality in previous studies [2,3].
Although the in-hospital mortality in patients with RVMI in this study was significantly lower than a previous study [26] (31% versus 6%), it was still significantly higher (4.5% vs. 1.8%) even after primary angioplasty.
Limitation(s)
Being a cross-sectional observational study in a tertiary care centre, patients presenting within the first 12 hours of window period eligible for primary angioplasty were taken, which may indicate a selection bias and exclusion of patients with late presentations. Also, RV function was only assessed by Echocardiography, excluding magnetic resonance and nuclear imaging modalities, which are known to be better for assessing RV function.
Early recognition of RV involvement in IWMI with the help of ECG and higher cardiac biomarker levels will help in better management and avoidance of shock in this subset of patients with acute ST elevation MI. Further studies focussing on different management strategies like early use of mechanical support devices in such cases might help in preventing the higher morbidity and mortality in these patients.
Conclusion(s)
This study showed a significant correlation between cardiac marker levels and ventricular dysfunction. It was found that BNP levels >400 pg/mL and higher Trop I levels within first 12 hours in patients presenting with acute IWMI might indicate associated RVMI, implying significant myocardium at risk, resulting in RV dysfunction (higher TAPSE) associated with significant diastolic dysfunction of left ventricle (higher E/E’ ratio). This may play a major role in morbidity and mortality even after successful primary angioplasty.
Data are shown as mean±standard deviation or number (%). HTN: Hypertension; DM: Diabetes mellitus; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; HR: Heart rate; RVMI: Right ventricular myocardial infarction; IWMI: Inferior wall myocardial infarction. @independent t-test, #Comparison of proportion test *Significant at p<0.05
Data are shown as median±standard deviation. BNP: Brain natriuretic peptide; RVMI: Right ventricular myocardial infarction; Trop I: Troponin I; CK-MB: Creatine kinase muscle brain; RVMI: Right ventricular myocardial infarction; IWMI: Inferior myocardial infarction. @independent t test, #Comparison of proportion test *Significant at p<0.05
Data are shown as mean±standard deviation, LVEDD: Left ventricular end-diastolic diameter; LVESD: Left ventricular end-systolic diameter; LA: Left atrium; LVEF: Left ventricular ejection fraction; E/A ratio: Ratio of early to late diastolic filling; E/E’: Ratio of early filling velocity to tissue Doppler early filling velocity; RVMI: Right ventricular myocardial infarction; IWMI: Inferior myocardial infarction. @independent t-test *Significant at p<0.05
Data are shown as mean±standard deviation, TAPSE: Tricuspid annular plane systolic excursion; RSm: Right ventricular systolic wave; RVFAC: Right ventricle fractional area change; RVMI: Right ventricular myocardial infarction; RVMPI: Right ventricular myocardial performance index; RVMI: Right ventricular myocardial infarction; IWMI: Inferior myocardial infarction. @independent t-test, *Significant at p<0.05
Correlation level using Pearson’s correlation analysis. Significant at p<0.05
RVMI: Right ventricular myocardial infarction; IWMI: Inferior myocardial infarction. #Comparison of proportion test. Significant at p<0.05