Introduction
Recurring mastalgia, non-cyclical mastalgia and non-specific extra-mammary pain are usually categorised as breast pain.
Aim
To determine the most usual aetiology of mastalgia and its response to management modalities like topical Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), bromocriptine and danazol.
Materials and Methods
This cohort study was conducted amongst 130 reproductive women within 21 years to 50 years of age group, with breast pain as a chief complaint, in the General Surgery Department from June 2004 to December 2005. General and local clinical assessment was performed as per the proforma. Patients’ past records associated with breast pain were noted in the Out Patient Department (OPD). Patients underwent a comprehensive quantifiable assessment. Patients with flagrant lumps in the breast and lumps discovered with ultrasound or mammography, underwent Fine Needle Aspiration Cytology (FNAC).
Results
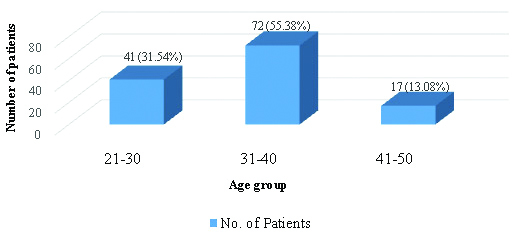
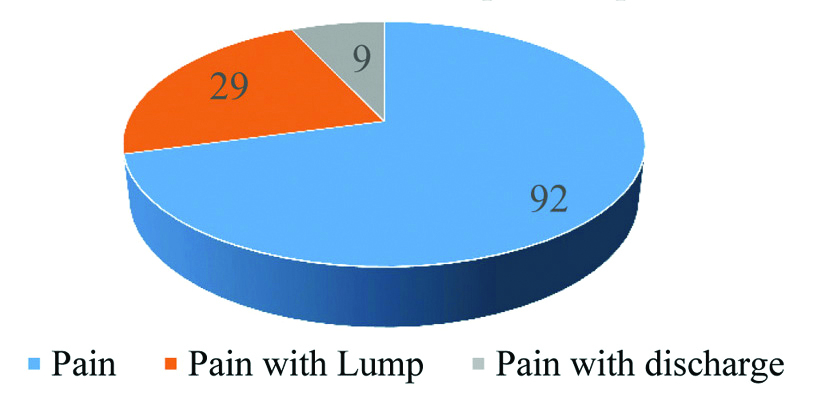
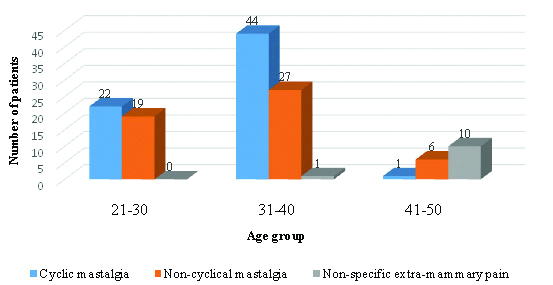
Amongst the total 130 patients, 41 (31.54%) were in age group of 21-30 years, 72 (55.38%) were in 31-40 years of age group and 17 (13.08%) were in 41-50 years of age group. The most frequent complaint was pain in the breast region which was seen in 92 patients comprising 70.77%, followed by pain with lump in 29 cases comprising 22.31 percent and pain with discharge in 9 patients comprising approximately 6.92%. Cyclic mastalgia was recorded in 22, 44 and 1 patients, non-cyclical mastalgia in 19, 27 and 6 patients and non-specific extra mammary pain in 0, 1 and 10 patients; in the age group of 21-30, 31-40 and 41-50 years respectively.
Conclusion
From the present study it is concluded that danazol, followed by bromocriptine and topical NSAIDs were effective in management of mastalgia. Their advantages in relieving symptoms must be balanced against their potential for unfavourable consequences.
Introduction
The term mastalgia first appeared in medical terminology in the year 1829 [1,2]. Mastalgia is an ordinary grievance in priliminary care and may influence up to 70% of women in their lifespan and in 10 to 20% of cases, it is severe [3-6]. The elevated height of community responsiveness concerning the breast cancer and the apprehension that mastalgia may point out sickness contribute to this drift [7]. Many patients with mastalgia can be treated with reassurance and routine prescription. Mastalgia is repeatedly associated with breast nodularity which may be soft or it may occur without a distinct lump. A quantity of breast nodularity and mastalgia have been established in normal population [6,8]. It is usual for ladies to experience mild breast pain for two or three days during pre-menstrual phase. However, 8 to 30% of cases account for moderate to severe breast pain with duration of five or more days each month [5].
Cyclical breast pain occurs one to two weeks prior to menses. The throbbing is normally experienced diffusely and bilaterally, with some radiation to the upper arm and axilla. It can be very severe in one breast than the other and it is relieved by the onset of menstrual flow. These patients are mostly seen between the age group of 30 to 40 years. The ailment may start abruptly in 22% of patients and sometimes may last in 65% of cases even after therapy [8]. Nevertheless, it can resolve with a hormonal event such as pregnancy or menopause, and due to this reason, it is assumed that cyclical mastalgia is due to hormonal stimulation of breast parenchyma, chiefly at the end of the luteal stage of the menstrual cycle [9]. For most of them, it may be about tolerating the pain until it decreases at menopause, if left untreated [8]. Non-cyclical mastalgia accounts for one-third of mastalgia. This type of mastalgia is widespread in grown-ups and post-menopausal cases. It frequently brings forth the non-radiating, jagged, smouldering or limited ache in one quadrant of the breast [9]. It is imperative to recall that non-cyclical mastalgia may be caused by benign breast pathology like big cysts in fibrocystic disease, periductal mastitis, engorgement during lactation or a breast abscess. Breast cancer may likely present as restricted softness. Frequently there is no explicit reason for the pain [10]. Non-specific extra-mammary aches may arise from the chest wall or other structures and may masquerade as a breast symptomatology [11].
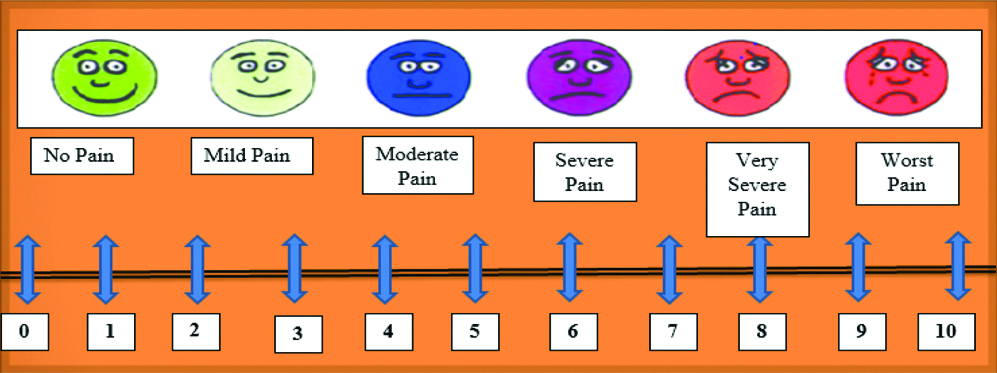
Excessive oestrogen and prolactin, less progesterone levels, or alterations in the oestrogen/progesterone ratio are theories concerning to the pathophysiology of mastalgia [12]. Menstrual irregularity, oral contraceptives, hormone treatment, psychotropic prescriptions, some cardiovascular agents, psychosocial factors, and physical trauma are associated with breast pain [7,13]. Pain may originate from ligaments in large, pendulous breasts [14]. Caffeine and nicotine consumption are also known to be associated with mastalgia [5]. Visual Analogue Scale (VAS) is used for evaluation of pain. VAS is defined as an instrument of pain measurement that tries to measure the intensity of pain. It is commonly used in epidemiological and clinical research [15]. This study was carried out to determine the most common aetiology of mastalgia and its response to management modalities like topical NSAIDs, bromocriptine, and danazol.
Materials and Methods
This cohort study was executed amongst 130 reproductive women in the age agroup of 21-50 years with breast pain as the chief complaint in the General Surgery department of Jubilee Mission Medical College and Research Institute, Thrissur, Kerala, India from June 2004 to December 2005. Written informed consent was obtained from the patients and study approval was taken from Institutional Ethics Committee (Ethical clearance no- EC/JMMCRI/612/2003/GS). Sample size was calculated by the formula of single proportions where n={Z2×P (1-P)}/E2. Local clinical examination and systemic examination were done as per the proforma. Patients’ past records related to breast pain were noted in the OPD. During detailed clinical examination, if any lumps were observed suspicious of carcinoma then these patients were advised radiographic investigations like ultrasonography, if aged <40 years and mammography, if aged >40 years. FNAC was done in those patients having palpable breast lumps, lumps found in ultrasonography and mammography. This study included those patients whose FNAC reports revealed benign lesions. Patients were categorised into six groups as displayed in [Table/Fig-1]. In the first three groups, assessment of pain was done using VAS displayed in [Table/Fig-2], at the start of the treatment and post-treatment, each week for the first month and thereafter monthly for the next six months. Last three groups were evaluated by using Cardiff Breast pain score as shown in [Table/Fig-3], at the interval after two, four and six months. Drugs were either continued/changed/surgery done as recommended by the treating clinician.
Study groups and respective medical management.
| Group | Treatment | No. of patients (130) |
|---|
| Group A | Danazol 200 mg BD for six months | 25 |
| Group B | Bromocriptine 2.5 mg BD for six months | 20 |
| Group C | Topical NSAIDs 2% TDS for six months | 20 |
| Group D | Evening primrose oil (EPO) for two months | 45 |
| Group E | Vitamin E (VIT E) for two months | 11 |
| Group F | Patients who did not receive any drugs. | 9 |
Visual Analogue Scale (VAS).
Cardiff Breast Pain Score (CBS).
| Cardiff breast pain score | Description |
|---|
| CBS 1 | An excellent response with no residual pain |
| CBS 2 | A substantial response but with some residual pain, considered by the patient to be bearable |
| CBS 3 | A poor response with substantial residual pain |
| CBS 4 | No beneficial response at all. |
Inclusion criteria: Patients in the age group of 21 to 50 years and all patients suspected or identified to have breast pathology with mastalgia were included.
Exclusion criteria: All established cases of malignancies, immune compromised patients, those with history of surgical removal of breast lump and pregnant females were excluded.
Statistical Analysis
The data was computed in Excel. Frequencies/descriptive, contingency coefficient and t-test were employed. All the data were analysed by Statistical Package for the Social Sciences (SPSS) version 20.0. The p-value <0.05 was considered significant.
Results
A total of 130 mastalgia patients were evaluated in this study. The most common age group was 31-40 years followed by age groups 21-30 years and 41-50 years as shown in [Table/Fig-4].
Age distribution of patients with mastalgia.
The most widespread or frequent indication was pain in the breast region in patients counting to 70.77% pursued by pain with lump in 22.31% and pain with discharge in 6.92% [Table/Fig-5].
Distribution of patients according to chief complaints.
Cyclic mastalgia was more common as compared to non-cyclic mastalgia in age groups of 21-30 years and 31-40 years, where as non-cyclic mastalgia was more common in age group 41-50 years compared to cyclic mastalgia. Non-specific extra-mammary pain was observed in one patient in the age group of 31-40 years and in 10 patients in the age group of 41-50 years [Table/Fig-6].
Age distribution of patients with different types of mastalgia.
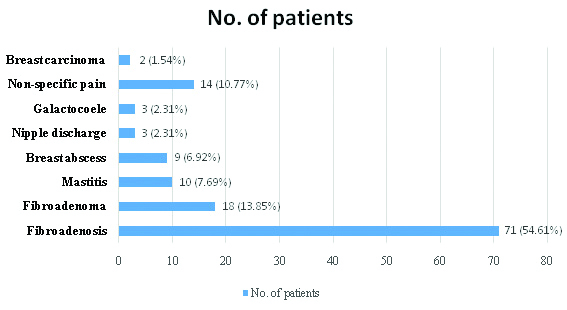
In this study, many causes for mastalgia were distinguished. The most frequent cause was fibroadenosis in 71 (54.61%) cases, followed by fibroadenoma in 18 patients (13.85%), non-specific mastalgia in 14 patients (10.77%), whereas other causes are shown in [Table/Fig-7].
Distribution of patients according to diagnosis.
Among 65 patients of group D,E and F, 45 (69.23%), 11 (16.92%) and 9 (13.85%) patients were started with evening primrose, Vitamin E and managed by reassurance without pharmacotherapy, respectively, which is shown in [Table/Fig-8].
Response distribution of patients receiving EPO, VIT E and No Drugs.
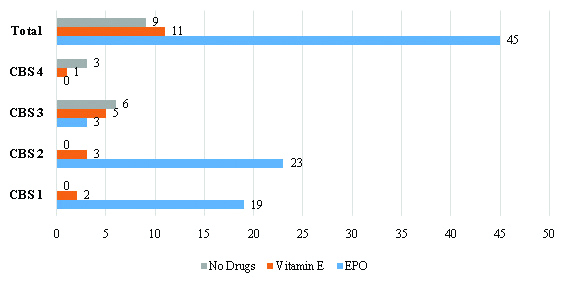
Review at four months and six months showed substantial response of patients to EPO with most of the patients having either CBS 1 or CBS 2 response; three of the patients having CBS 3 response. The mean VAS scores of patients treated with different medications are shown in [Table/Fig-9].
Comparison of mean VAS scores of patients treated with different medications.
| VAS score | Danazol | Bromocriptine | Diclofenac gel | p-value* |
|---|
| Mean | SD | Mean | SD | Mean | SD |
|---|
| At 1 weeks | 6.19 | 0.935 | 6.87 | 0.634 | 6.91 | 0.654 | 0.005 |
| At 2 weeks | 5.53 | 0.895 | 6.18 | 0.821 | 6.01 | 0.597 | 0.07 |
| At 3 weeks | 5.16 | 0.841 | 5.53 | 0.764 | 5.83 | 0.632 | 0.32 |
| At 2 months | 4.87 | 0.749 | 4.86 | 0.631 | 5.03 | 0.697 | 0.05 |
| At 3 months | 4.35 | 0.915 | 4.13 | 0.596 | 4.56 | 0.874 | 0.04 |
| At 4 months | 3.69 | 1.117 | 3.56 | 0.473 | 3.79 | 0.905 | 0.92 |
| At 5 months | 2.74 | 1.341 | 3.21 | 1.262 | 2.48 | 1.256 | 0.02 |
| At 6 months | 2.18 | 1.676 | 2.59 | 1.679 | 1.64 | 1.035 | 0.02 |
t-test done * p<0.05 significant
Discussion
Amongst the total 130 patients, 41 (31.54%), 72 (55.38%) and 17 (13.08%) patients were in the age groups of 21-30, 31-40 and 41-50 years, respectively. In a research work on 375 cases carried out by Geschickter CF, he reported a mean age of 35 years with a mean pain duration of 21.5 months [16]. According to the Cardiff breast clinic report previously published, mastalgia was observed among 212 women between ages of 12-51 years with median age of 36 years [17]. For both the cyclical and non-cyclical mastalgia, the utmost frequency was in the 3rd decade in present study. Cyclical mastalgia is normally seen in 3rd decade of life [18].
Rungruang B and Kelley JL observed that breast lump was not commonly associated with breast pain among 350 patients studied and most of the lumps were found to be non-carcinomatous [18]. In this study, the most common chief complaint was breast pain in 92 (70.77%) cases, followed by ache with lump in 29 (22.31) cases and ache with discharge in 9 (6.92%) cases. Comparable findings were found by Guerriero S et al., in which breast pain was recorded in 48% of the cases [19]. In another study, it was found that when the onset of mastalgia was in pre-menarche, the severity tends to be more and less amicable to treatment [17,20].
Many causes of mastalgia were noted in this study. Fibroadenosis was considered to be the most common reason in 71 (54.61%) cases, followed by fibroadenoma, non-specific mastalgia, mastitis, breast abscess, galactocoele, nipple discharge and breast carcinoma respectively. Similar findings were recorded by Chowdhury RA et al., where he found 51 cases (48.1%) diagnosed as fibroadenosis, 16 (15.1%) as non-specific mastalgia, 15 (14.2%) as breast abscess, 10 (9.4%) as diseases of nipple, 2 (1.9%) as carcinoma of breast and 1 (0.94%) as galactocele [21]. In other research performed by Khanna AK et al., they found three (3.75%) cases of nipple discharge [22]. Rosolowich V et al., observed that mastalgia tends to be the presenting complaint in 10-15% of carcinomatous lesions of breast [23]. Hormonal and nutritional basis have also been hypothesised in causation of mastalgia for a long time [24]. Danazol alleviates breast pain and softness in clinical trials [25-29]. On the whole, 59% to 92% of women reported relief from pain after danazol treatment [25-29]. Typically, the early dosage is 200 mg/d with eventual tapering to lower-dose, 177 alternate-day, or luteal phase administration [30-33]. However, initial dosages of 50 to 400 mg/d have been described in other studies [25,31]. Interestingly, danazol was associated with declined mammographic breast volume and density in 25 cases with breast pain, 23 of whom experienced complete resolution of symptoms [34]. Bromocriptine reduces serum prolactin. Three randomised controlled trials and one cohort work on bromocriptine reported the resolution of mastalgia in 65% of cases [35,36]. Side-effects comprise nausea, giddiness and hypotension in 69% of patients.
Among 65 patients of group D, E and F 45 (69.23%), 11 (16.92%) and 9 (13.85%) were started with evening primrose, Vitamin E and managed by reassurance without drugs, respectively. For breast pain, vitamin E is taken most frequently. Previous works with less number of patients recommended a probable helpful consequence of vitamin E (α-tocopherol) in fibrocystic breast ailment [37-39]. There is no evidence that support the uses of vitamins to treat mastalgia, moreover, there are studies that have documented that the doctors use vitamin B1, B6 and E [40]. Long term use of vitamins may enhance the risk of haemorrhagic stroke. In another study, they found considerable benefits of evening primrose oil and vitamins. However, use of placebo had a questionable effect on these patients [41].
The probable mechanisms of action of Vitamin E are through its ability to modify steroidal hormone synthesis, to correct abnormal serum cholesterol-lipoprotein distribution, and to function as an antioxidant [42-44]. For women with cyclic breast pain who do not wish to take medications, evening primrose oil has been extensively suggested as a safe alternative [7,45-49]. Two small randomised, double-blind, placebo-controlled studies on evening primrose oil have shown efficacy in reduction of breast pain [50,51].
Limitation(s)
This study had a small sample size. Still there is paucity of data, so there is need for large cohort studies to improve understanding of mastalgia. It will help to reveal the other causes and better management of women with moderate to severe pain. The current study was small and did not consider the response to surgical intervention.
Conclusion(s)
Breast pain is a common clinical condition among females of reproductive age groups. This work showed that cyclical and non-cyclical mastalgia is very common in 3rd decade of life. In this study, the response to therapy was best with danazol, followed by bromocriptine and to topical NSAIDs.
t-test done * p<0.05 significant
[1]. Cooper A, Illustrations of the Diseases of the Breast, Part 1 1829 London, EnglandLongman, Rees, Orme, Brown & Green [Google Scholar]
[2]. Grimm K, Fritsche E, Reduction of breasts: Hans Schaller and the first mammaplasty in 1561 [in German]Handchir Mikrochir Plast Chir 2000 32:316-20.10.1055/s-2000-1093611103688 [Google Scholar] [CrossRef] [PubMed]
[3]. Cairncross L, MastalgiaContin Med Ed 2010 28(11):504 [Google Scholar]
[4]. Arslan M, Küçükerdem HS, Can H, Tarcan E, Retrospective analysis of women with only mastalgiaJ Breast Health 2016 12(4):151-54.10.5152/tjbh.2016.294428331753 [Google Scholar] [CrossRef] [PubMed]
[5]. Ader DN, South-Paul J, Adera T, Deuster PA, Cyclicalmastalgia: Prevalence and associated health behavioral factorsJ Psychosom Obstet Gynaecol 2001 22:71-76.10.3109/0167482010904995611446156 [Google Scholar] [CrossRef] [PubMed]
[6]. Mansel RE, Webster DJT, Sweetland HM, Breast pain and nodularity. In: Mansel RE, Webster DJT, Sweetland HM (eds)Benign disorders and disease of the breast 2009 3rd ednPhiladelphiaSaunders Elsevier:107-38.10.1016/B978-0-7020-2774-1.00012-8 [Google Scholar] [CrossRef]
[7]. Morrow M, The evaluation of common breast problemsAm Fam Physician 2000 61:2371-78. [Google Scholar]
[8]. Kumar S, Rai R, Das V, Dwivedi V, Kumar S, Agrawal GG, Visual analogue scale for assessing breast nodularity in nondiscrete lumpy breasts: The Lucknow Cardiff breast nodularity scaleThe Breast 2010 19:238-42.10.1016/j.breast.2010.02.00220223665 [Google Scholar] [CrossRef] [PubMed]
[9]. Wisbey JR, Kumar S, Mansel RE, Preece PE, Pye JK, Hughes LE, Natural history of breast painLancet 1983 ii:672-74.10.1016/S0140-6736(83)92543-6 [Google Scholar] [CrossRef]
[10]. Salzman B, Fleegle S, Tully AS, Common breast problemsAm Fam Physician 2012 86:343-49. [Google Scholar]
[11]. Thakur N, Zargar B, Nazeer N, Parray F, Wani R, Mastalgia- Use of evening primrose oil in treatment of mastalgiaInt J Surg 2010 24(2):01-06.10.5580/2630 [Google Scholar] [CrossRef]
[12]. Iddon J, Mastalgia; in Dixon JM (ed): ABC of breast disease 2006 3rd edEdinburgh, UKBlackwell Publishing:15-18. [Google Scholar]
[13]. Leung JW, Korguth PJ, Gotway MB, Utility of targeted sonography in the evaluation of focal breast painJ Ultrasound Med 2002 21:521-26.10.7863/jum.2002.21.5.52112008815 [Google Scholar] [CrossRef] [PubMed]
[14]. Smith RL, Pruthi S, Fitzpatrick LA, Evaluation and management of breast painMayo Clin Proc 2004 79:353-72.10.4065/79.3.35315008609 [Google Scholar] [CrossRef] [PubMed]
[15]. Ader DN, Shriver CD, Cyclical mastalgia: Prevalence and impact in an outpatient breast clinic sampleJ Am Coll Surg 1997 185(5):466-70.10.1016/S1072-7515(97)00095-1 [Google Scholar] [CrossRef]
[16]. Geschickter CF, Mastodynia (Painful breasts)In: Diseases of the Breast 1945 2nd EditionPhiladelphiaJB. Lippincott Co.:183-99. [Google Scholar]
[17]. Davies EL, Gateley CA, Miers M, Mansel RE, The Long-Term Course of MastalgiaJ R Soc Med 1998 91(9):462-64.10.1177/0141076898091009039849515 [Google Scholar] [CrossRef] [PubMed]
[18]. Rungruang B, Kelley JL, Benign breast diseases: Epidemiology, evaluation, and managementClinical Obstetrics and Gynecology 2011 54(1):110-24.10.1097/GRF.0b013e318208010e21278510 [Google Scholar] [CrossRef] [PubMed]
[19]. Guerriero S, Alcazar JL, Ajossa S, Galvan R, Laparte C, García MM, Transvaginal colour doppler imaging in the detection of ovarian cancer in a large study populationInt J Gynecol Cancer 2010 20(5):781-86.10.1111/IGC.0b013e3181de948120973268 [Google Scholar] [CrossRef] [PubMed]
[20]. Hughes LE, Mansel RE, Webster DJT, Aberrations of normal development and involution (ANDI): A concept of benign breast disorders based on pathogenesis, in Hughes LE, Mansel RE, Webster DJT (eds)Benign Disorders and Diseases of the Breast Concepts and Clinical Management 2000 2nd edPhiladelphiaWB Saunders:21:73 [Google Scholar]
[21]. Chowdhury RA, Hasan SK, Masud JMD, Analysis of breast pain: A study of 110 casesJ Medi 2009 10(2):77-81.10.3329/jom.v10i2.2818 [Google Scholar] [CrossRef]
[22]. Khanna AK, Tapodar J, Misra MK, Spectrum of benign breast disorders in a university hospitalJ Indian Med Assoc 1997 95(1):05-08. [Google Scholar]
[23]. Rosolowich V, Saettler E, Szuck B, Lea RH, MastalgiaJ Obstet Gynaecol Can 2006 28(1):49-71.10.1016/S1701-2163(16)32027-8 [Google Scholar] [CrossRef]
[24]. Tumyan L, Hoyt AC, Bassett LW, Negative predictive value of sonography and mammography in patients with focal breast painBreast J 2005 11(5):333-37.10.1111/j.1075-122X.2005.00018.x16174154 [Google Scholar] [CrossRef] [PubMed]
[25]. Mansel RE, Wisbey JR, Hughes LE, Controlled trial of the antigonadotropin danazol in painful nodular benign breast diseaseLancet 1982 1:928-30.10.1016/S0140-6736(82)91932-8 [Google Scholar] [CrossRef]
[26]. Ramsey-Stewart G, The treatment of symptomatic benign breast disease with danazolAust N Z J Obstet Gynaecol 1988 28:299-304.10.1111/j.1479-828X.1988.tb01686.x3074777 [Google Scholar] [CrossRef] [PubMed]
[27]. Watts JF, Butt WR, Logan Edwards R, A clinical trial using danazol for the treatment of premenstrual tensionBr J Obstet Gynaecol 1987 94:30-34.10.1111/j.1471-0528.1987.tb02248.x3545282 [Google Scholar] [CrossRef] [PubMed]
[28]. O’Brien PM, Abukhalil IE, Randomised controlled trial of the management of premenstrual syndrome and premenstrual mastalgia using luteal phase-only danazolAm J Obstet Gynecol 1999 180(1, pt 1):18-23.10.1016/S0002-9378(99)70142-0 [Google Scholar] [CrossRef]
[29]. Gorins A, Perret F, Tournant B, Rogier C, Lipszyc J, A French double-blind crossover study (danazol versus placebo) in the treatment of severe fibrocystic breast diseaseEur J Gynaecol Oncol 1984 5:85-89. [Google Scholar]
[30]. Sutton GL, O’Malley VP, Treatment of cyclical mastalgia with low dose short term danazolBr J Clin Pract 1986 40:68-70. [Google Scholar]
[31]. Tobiassen T, Rasmussen T, Doberl A, Rannevik G, Danazol treatment of severely symptomatic fibrocystic breast disease and long-term follow-up-The Hjorring projectActa Obstet Gynecol Scand Suppl 1984 123:159-76.10.3109/000163484091570066594009 [Google Scholar] [CrossRef] [PubMed]
[32]. Maddox PR, Harrison BJ, Mansel RE, Low-dose danazol for mastalgiaBr J Clin Pract Suppl 1989 68:43-47. [Google Scholar]
[33]. Harrison BJ, Maddox PR, Mansel RE, Maintenance therapy of cyclical mastalgia using low-dose danazolJ R Coll Surg Edinb 1989 34:79-81. [Google Scholar]
[34]. Ouimet-Oliva D, Van Campenhout J, Hebert G, Ladouceur J, Effect of danazol on the radiographic density of breast parenchymaJ Can Assoc Radiol 1981 32:159-61. [Google Scholar]
[35]. Mansel RE, Dogliotti L, European multicentre trial of bromocriptine in cyclical mastalgiaLancet 1990 335:190-93.10.1016/0140-6736(90)90278-D [Google Scholar] [CrossRef]
[36]. Blichert-Toft M, Andersen AN, Henriksen OB, Mygind T, Treatment of mastalgia with bromocriptine: A double blind cross-over studyBMJ 1979 1(6158):23710.1136/bmj.1.6158.237369653 [Google Scholar] [CrossRef] [PubMed]
[37]. Solomon D, Strummer D, Nair PP, Relationship between vitamin E and urinary excretion of ketosteroid fractions in cystic mastitisAnn N Y Acad Sci 1972 203:103-10.10.1111/j.1749-6632.1972.tb27862.x4266685 [Google Scholar] [CrossRef] [PubMed]
[38]. Sundaram GS, London R, Manimekalai S, Nair PP, Goldstein P, Alpha-tocopherol and serum lipoproteinsLipids 1981 16:223-27.10.1007/BF025350207242274 [Google Scholar] [CrossRef] [PubMed]
[39]. Ernster VL, Goodson WH III, Hunt TK, Petrakis NL, Sickles EA, Miike R, Vitamin E and benign breast “disease”: A double-blind, randomised clinical trialSurgery 1985 97:490-94. [Google Scholar]
[40]. Colak T, Ipek T, Kanik A, Efficacy of topical nonsteroidal anti-inflammatory drugs in mastalgia treatmentJ Am Coll Surg 2003 196:525-30.10.1016/S1072-7515(02)01893-8 [Google Scholar] [CrossRef]
[41]. Shurks M, Glynn RJ, Rist PM, Tzourio C, Kurth T, Effects of vitamin E on stroke subtypes: Meta-analysis of randomised controlled trialsBMJ 2010 341:c5702-1315.10.1136/bmj.c570221051774 [Google Scholar] [CrossRef] [PubMed]
[42]. Meyer EC, Sommers DK, Reitz CJ, Mentis H, Vitamin E and benign breast diseaseSurgery 1990 107:549-51. [Google Scholar]
[43]. London RS, Sundaram GS, Murphy L, Manimekalai S, Reynolds M, Goldstein PJ, The effect of vitamin E on mammary dysplasia: A double-blind studyObstet Gynecol 1985 65:104-06. [Google Scholar]
[44]. BeLieu RM, MastodyniaObstet Gynecol Clin North Am 1994 21:461-77.10.1016/S0889-8545(21)00646-X [Google Scholar] [CrossRef]
[45]. Dixon JM, Managing breast painPractitioner 1999 243:484-86.:488-89.:91 [Google Scholar]
[46]. Klimberg VS, Etiology and management of breast pain. In: Harris JR, Lippman ME, Morrow M, Hellman S, edsDiseases of the Breast 1996 Philadelphia, PaLippincott-Raven:99-106. [Google Scholar]
[47]. Gateley CA, Mansel RE, Management of cyclical breast painBr J Hosp Med 1990 43:330-32. [Google Scholar]
[48]. Steinbrunn BS, Zera RT, Rodriguez JL, Mastalgia: Tailoring treatment to type of breast painPostgrad Med 1997 102:183-84.:187-89.:193-94.10.3810/pgm.1997.11.3699385340 [Google Scholar] [CrossRef] [PubMed]
[49]. Pashby NL, Mansel RE, Hughes LE, Hanslip J, Preece PE, A clinical trial of evening primrose oil in mastalgiaBr J Surg 1981 68:801 [Google Scholar]
[50]. Preece PE, Hanslip JI, Gilbert L, Evening primrose oil (efamol) for mastalgia. In: Horrobin DF, edClinical Uses of Essential Fatty Acids 1982 Montreal, QuebecEden Press:147-54. [Google Scholar]
[51]. Wetzig NR, Mastalgia: A 3 year Australian studyAust N Z J Surg 1994 64:329-31.10.1111/j.1445-2197.1994.tb02221.x8179529 [Google Scholar] [CrossRef] [PubMed]