Endoscopically-Assisted Intraoral Resection of Compound Odontoma Arising from the Inferomedial Surface of the Mandibular Ramus using Piezosurgery
Toshinori Iwai1, Satomi Sugiyama2, Hiroaki Kitajima3, Makoto Hirota4, Kenji Mitsudo5
1 Doctor, Department of Oral and Maxillofacial Surgery/Orthodontics, Yokohama City University Hospital, Yokohama, Kanagawa, Japan.
2 Doctor, Department of Oral and Maxillofacial Surgery/Orthodontics, Yokohama City University Hospital, Yokohama, Kanagawa, Japan.
3 Doctor, Department of Oral and Maxillofacial Surgery/Orthodontics, Yokohama City University Hospital, Yokohama, Kanagawa, Japan.
4 Doctor, Department of Oral and Maxillofacial Surgery/Orthodontics, Yokohama City University Medical Center, Yokohama, Kanagawa, Japan.
5 Doctor, Department of Oral and Maxillofacial Surgery/Orthodontics, Yokohama City University Hospital, Yokohama, Kanagawa, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Toshinori Iwai, 3-9 Fukuura Kanazawa-ku, Yokohama, Kanagawa, Japan.
E-mail: iwai104oams@yahoo.co.jp
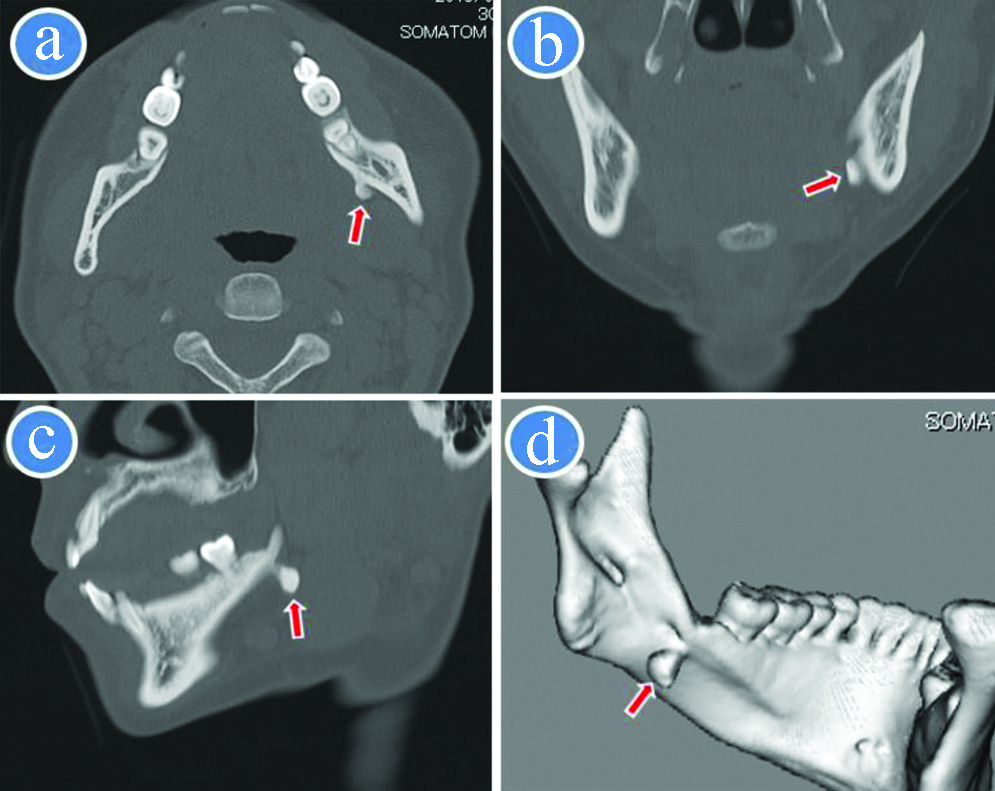
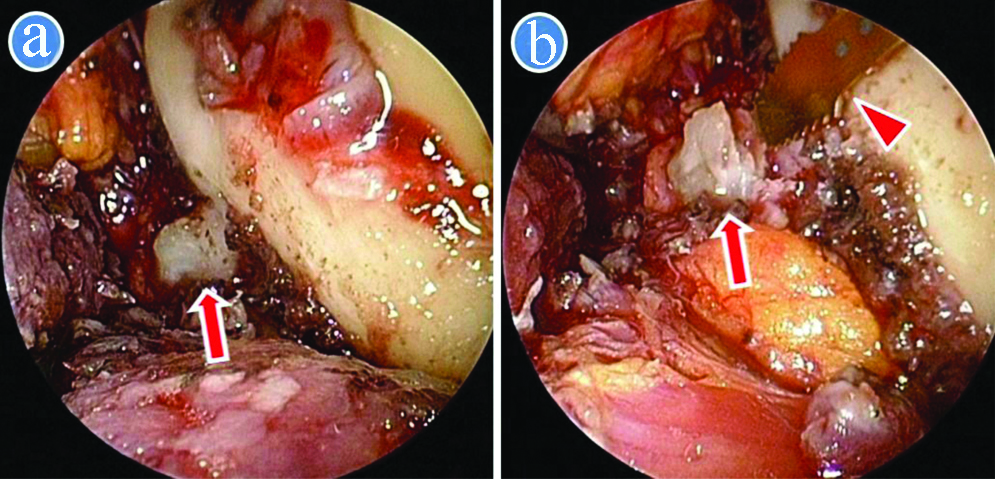
Bone, Endoscope, Mandible, Minimally invasive surgical procedures
A 45-year-old woman presented with left submandibular discomfort for several years. There was no history of the mandibular trauma or previous medical and family history including Gardner’s syndrome. Although several dental treatments including dental restorations and periodontal therapy were performed, the left lower wisdom tooth was missing by nature. An about 5-mm-diameter painless hard mass was identified by palpation in the inferomedial mandibular ramus, and was immobile. She had no difficulty on swallowing, discharge from the overlying normal skin, facial asymmetry, and regional lymphadenopathy. A left lower second molar was vital. Computed Tomography (CT) showed a hyperdense, well-circumscribed, pedunculated mass attached to the inferomedial surface of the mandibular ramus, measuring 6.7×5.1×7.6 mm [Table/Fig-1]. The radiological diagnosis was peripheral osteoma, because CT values of the lesion were similar to bone. Informed consent was obtained for surgery, but patient refused an extraoral approach. Therefore, as a minimally invasive surgery, she underwent endoscopically-assisted intraoral resection of the lesion using piezosurgery (Mectron Medical Technology, Carasco, Italy) under general anaesthesia. The lingual crevicular incision was made on the gingiva from the lateral incisor to the second molar, with extension to the retromolar area for relief of the flap. The mucoperiosteal flap was elevated to the mylohyoid muscle region. The mylohyoid muscle attachment was incised, and further elevation in the medial surface of the mandible was performed. The bony lesion which intruded into the soft tissue was exposed by the incision of the periosteum and soft tissue, and then the projected bone along the mylohyoid line was removed to improve access to the bony lesion using a rotary bur of AESCULAP® (B.Braun, Melsungen, Germany). A 30-degree, 4-mm-diameter endoscope with tissue retractor (Karl Storz, Tuttlingen, Germany) was inserted into the surgical space, and the bony lesion was resected safely using piezosurgery under endoscopic guidance [Table/Fig-2]. After the complete removal, the bone surface was removed smoothly. The specimen was a hard bony lesion [Table/Fig-3]. Surgical time was 58 minutes. She was discharged on the first day after surgery. The histopathological diagnosis was compound odontoma, because the specimen showed dentin and cementum [Table/Fig-4]. The postoperative course was uneventful without palsy of the mental and lingual nerve, and there was no recurrence two years after surgery.
CT and 3D-CT image. a) Axial image; b) Coronal image; c) Oblique sagittal image; d) 3D image. Arrow indicates bony lesion on the inferormedial surface of the mandibular ramus.
Endoscopic view. a) Exposure of bony lesion (arrow) on the inferormedial surface of the mandibular ramus; b) Resection of bony lesion (arrow) using piezosurgery (arrow head).

A microscopic image of the specimen shows dentin and cementum (haematoxylin and eosin staining).

Odontomas are slow-growing odontogenic tumours which are made of tissues which comprise the teeth like enamel, dentine, cementum, and pulp tissue. They are commonly clinically asymptomatic, and often associated with tooth eruption disturbances for intraosseous lesions. Peripheral (extraosseous) odontomas are extremely rare, and some might be erupted [1]. In the present case, because CT showed a pedunculated mass was located at the inferomedial surface of the mandibular ramus and CT values of the homogeneous lesion were almost similar to cortical bone hence, a provisional diagnosis of osteoma was made. As a differential diagnosis of peripheral bony lesions such as exostoses, osteochondroma, osteoblastoma, and ossifying fibroma, odontoma also should be considered.
Although the treatment of odontoma is surgical resection, the selection of an appropriate surgical approach should be made on an individual basis after considering the size, shape, and origin of the tumour. Because extraoral approaches have a risk of facial nerve injury and visible scar, an intraoral approach as a minimally invasive surgery should be performed as much as possible. However, limited surgical access, poor visualisation, and potential injury of vital structures make the intraoral approach difficult.
An endoscope can provide good illumination and visualisation in a deep and limited surgical field. In the oral and maxillofacial region, endoscopically-assisted intraoral surgery has been performed for plate fixation of subcondylar fracture, removal of an impacted tooth, cyst, tumour and foreign body. Especially, surgical access to the medial side of the mandibular ramus is limited and challenging. But, Yaslikaya S et al., reported endoscopic transoral resection of pharyngeal osteoma arising from the medial ramus to preserve the temporomandibular joint function and to minimise complications and the patient’s aesthetic concerns [2]. The osteoma could be resected intraorally without an external scar using endoscopic assistance.
Piezosurgery (piezoelectric bone surgery) is a novel technique that uses ultrasonic microvibrations to cut bone tissue. Comparing with rotary instruments, piezosurgery can provide more favorable bone healing, soft tissue protection, optimal visibility in the surgical field [3-5]. In oral and maxillofacial region, piezosurgery is used for various bone surgery such as sinus floor elevation, bone graft harvesting, orthognathic surgery [3-5]. The use of both endoscope and piezosurgery can allow even more minimally invasive surgery in the oral and maxillofacial region. Ochiai S et al., reported endoscopic-assisted intraoral resection of peripheral osteoma on the inferolateral border of the mandibular angle using piezosurgery, and the osteoma was resected easily and safely [3]. In the present case, odontoma arising from the inferomedial surface of the mandibular ramus could be resected in an intraoral approach safely and accurately without injury of the marginal mandibular branch of the facial nerve and facial artery by use of piezosurgery and endoscope.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 23, 2020
Manual Googling: Sep 29, 2020
iThenticate Software: Nov 25, 2020 (14%)
[1]. de Oliveira MA, Reis B, Pallos D, Kim YJ, Braz-Silva PH, Martins F, The importance of histopathological examination to the final diagnosis of peripheral odontogenic tumours: A case report of a peripheral odontomaCase Rep Dent 2019 2019:971281610.1155/2019/971281631583140 [Google Scholar] [CrossRef] [PubMed]
[2]. Yaslikaya S, Koca CF, Toplu Y, Kizilay A, Akpolat N, Endoscopic transoral resection of parapharyngeal osteoma: A case reportJ Oral Maxillofac Surg 2016 74(11):2329.e01-05.10.1016/j.joms.2016.06.17727444102 [Google Scholar] [CrossRef] [PubMed]
[3]. Ochiai S, Kuroyanagi N, Sakuma H, Sakuma H, Miyachi H, Shimozato K, Endoscopic-assisted resection of peripheral osteoma using piezosurgeryOral Surg Oral Med Oral Pathol Oral Radiol 2013 115(1):e16-20.10.1016/j.oooo.2011.09.03223217547 [Google Scholar] [CrossRef] [PubMed]
[4]. Gadre P, Singh D, Gadre K, Khan I, Piezosurgery for excision of large osteoid osteomaJ Craniofac Surg 2016 27(7):e701-02.10.1097/SCS.000000000000302827564070 [Google Scholar] [CrossRef] [PubMed]
[5]. Hernando J, Aguilar-Salvatierra A, Leizaola-Cardesa IO, Seijas PM, Aguirre-Echebarria P, Martín J, Piezosurgery for treatment of large recurrent mandibular osteomaJ Craniofac Surg 2018 29(3):e219-21.10.1097/SCS.000000000000414129283937 [Google Scholar] [CrossRef] [PubMed]