Multiple Keratocyst Glimpses Falx Cerebri and Bifid Rib- A Case of Gorlin-Goltz Syndrome
Vrushali Baburao Zamare1, Rahul Bhowate2, Vidya Lohe3, Mrunal Meshram4
1 Postgraduate Student, Department of Oral Medicine and Radiology, Sharad Pawar Dental College and Hospital, DMIMS, Sawangi, Maharashtra, India.
2 Professor, Department of Oral Medicine and Radiology, Sharad Pawar Dental College and Hospital, DMIMS, Wardha, Maharashtra, India.
3 Professor and Head, Department of Oral Medicine and Radiology, Sharad Pawar Dental College and Hospital, DMIMS, Wardha, Maharashtra, India.
4 Lecturer, Department of Oral Medicine and Radiology, Sharad Pawar Dental College and Hospital, DMIMS, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Vrushali Baburao Zamare, Radhikabai, PG Girls Hostel, Sharad Pawar Dental College and Hospital, Sawangi (M), Maharashtra, India.
E-mail: vrushalimzamare@gmail.com
Multiple Odontogenic keratocysts with multi-organ abnormalities are a feature of Gorlin-Goltz Syndrome (GGS) which is an autosomal dominant inherited disorder. The most common oral manifestation of GGS is odontogenic keratocyst. Early diagnosis of GGS without cutaneous manifestations is important as this syndrome has basal cell carcinoma as one of its major criteria. This paper includes a case report of a 24-year-old female who reported with swelling and pus discharge in lower right posterior region. The swelling was clinico-radiologically diagnosed as odontogenic keratocyst on a panoramic radiograph which revealed the presence of multiple cystic lesions in symphysis, parasymphysis, and bilateral maxillary region. Postero-Anterior (PA) chest showed bifid ribs and PA skull showed calcification of falxcerebri. Histopathological diagnosis confirmed the Odontogenic keratocyst. Ultrasonography (USG) abdomen revealed a simple ovarian cyst on the right side. Clinical examination findings and radiological imaging evaluation with histopathological examination of cystic lesion confirms Gorlin-Goltz. Surgical enucleation of the keratocyst, peripheral ostectomy followed by bone graft substitute, and primary closure under General Anaesthesia (GA) were done in the Department of Oral and Maxillofacial Surgery. Follow-up healing was uneventful after one month.
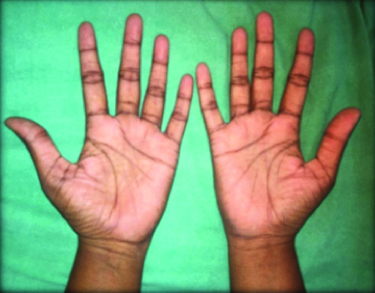
Multiple cystic lesions, Ovarian cyst, Palmer pits
Case Report
A 24-year-old female reported with a chief complaint of painful intraoral swelling in the lower right back region of jaw, difficulty in mastication, and gingival pus discharge since one month. The pain was dull aching, intermittent, and localised to the lower right mandibular premolar and molar region. Family history was not significant. There was no evident swelling on the extraoral examination. Temporomandibular Joint (TMJ) examination revealed a deviation of mandible to the left side. The right submandibular lymph node was enlarged about 1×1 cm in size, firm, mobile, and tender.
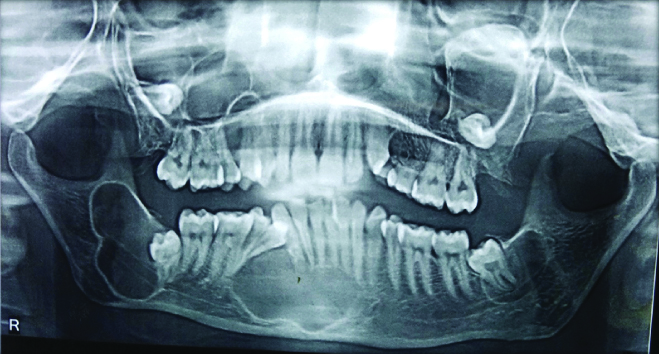
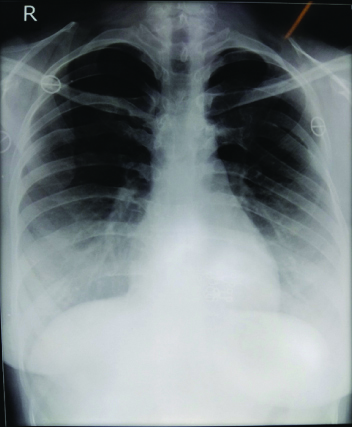
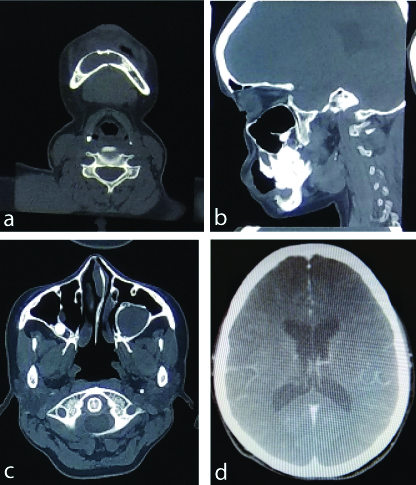
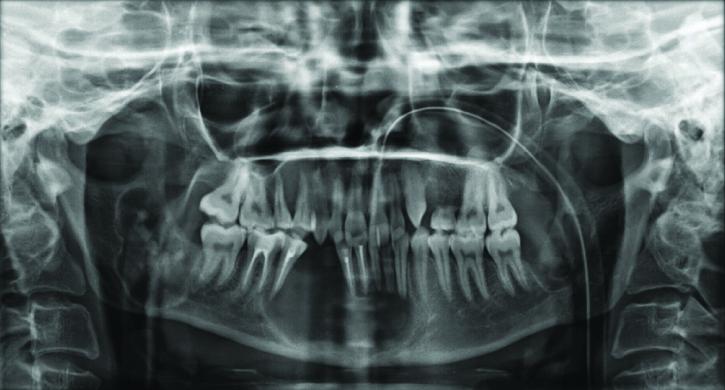
Intraoral examination revealed a lingual shift of tooth number 44 due to lingual gingival swelling with pus discharge. On palpation, diffused bony hard swelling in the lower labial sulcus of 46 regions which was extended from mesial of 46 to distal of 32. There was a slight expansion of the buccal cortical plate. Gingivobuccal sulcus was obliterated in 46 and 47 region and no lingual sulcus involvement [Table/Fig-1]. Clinically, 18, 24, 25, 28, 38 and 48 were non-erupted with over-retained 64 and 65. Considering minimum buccal expansion clinical provisional diagnosis of Odontogenic Keratocyst was given. OPG was advised which revealed well-corticated three radiolucent lesions with 38 and 48 involving ascending ramus and symphysis and Parasymphysis on the right side. A radiolucent lesion in symphysis, Parasymphysis and 48 regions showed scalloping with the involvement of ramus up to a coronoid notch and imperceptibly merging cortication laterally at 33 regions. A Radiolucent lesion with 38 was mimicking like a circumferential periapical cyst. Maxillary bilateral third molars were displaced and occupied the horizontal position with the involvement of the postero-lateral wall of maxillary sinuses [Table/Fig-2]. As there were the presence of multiple lesions, Postero-Anterior (PA) chest and Antero-Posterior (AP) skull radiographs, Computed Tomography (CT) and Ultrasonography (USG) abdomen were advised. Clinical examination revealed palmer pits [Table/Fig-3]. AP skull showed calcification of falx cerebri and PA chest showed bifid rib with 4th rib [Table/Fig-4]. CT evaluation revealed bony expansile unilocular cystic lesions of variable sizes. There was a presence of cortical thinning in symphysis mentis and right side body of the mandible and bilateral rami of the mandible, postero-lateral wall of the maxillary sinus, and also in the alveolar process of the maxilla. Third molars were impacted bilaterally [Table/Fig-5a-c]. There was a presence of thin calcification along the falx cerebri [Table/Fig-5d]. The patient came with reports of USG abdomen which was done at a private clinic revealed left ovarian simple cyst of size 5.3×4.3 cm. These radiological features of Multiple Keratocyst with Bifid rib, palmer pits, calcification of falx cerebri, and simple ovarian cyst favours GGS.
Swelling in lower labial sulcus from distal of 32 to mesial of 46 with slight expansion of buccal cortical plate and lingual gingival swelling, lingual shift of 44 is also present.

Orthopantomogram (OPG) shows well corticated three radiolucent lesions in 38, 32 to 44 & 48 region involving ascending ramus, symphysis and Parasymphysis on right side. Bilaterally Maxillary third molars are impacted.
PA chest showing bifid rib with 4th rib.
a), b) Computed Tomography (CT) shows multiple bony expansile unilocular cystic lesions of variable sizes with cortical thinning in symphysis mentis and right side body of mandible and bilateral rami of mandible; c) Posterolateral wall of maxillary sinus and also in alveolar process of maxilla with impacted third molar bilaterally; d) Calcification along the falx cerebri.
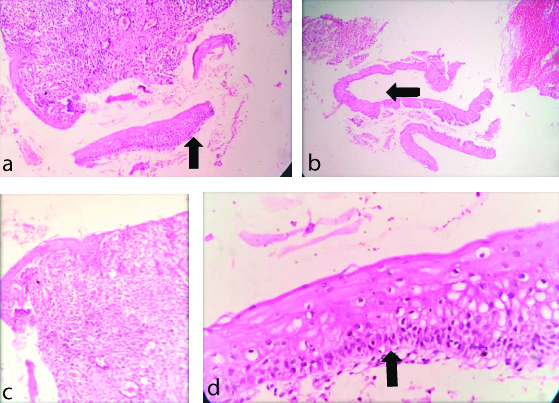
To confirm the diagnosis biopsy was performed under local anaesthesia and patient consent was taken. Hematoxylin and Eosin (H&E) stained histopathological evaluation showed a cystic space lined by non-keratinised stratified squamous epithelium and surrounding connective tissue capsule [Table/Fig-6a]. The epithelium appeared corrugated and 2-4 cells layer thick. The basal epithelial layer was made up of palisaded tall columnar epithelial cells with hyperchromatic nuclei and the detachment of epithelium from connective tissue was seen. H&E stained tissue showed corrugated epithelium [Table/Fig-6b]. The epithelium and border of connective tissue were flat and rete ridge formation was un-noticeable. Mild inflammatory cell infiltrates, chiefly lymphocytes were present and indicative of Odontogenic Keratocyst [Table/Fig-6c]. Clinical, radiological and histopathological diagnosis confirmed keratocyst with GGS. Cystic enucleation followed by peripheral ostectomy was done and on follow-up healing was uneventful after one month [Table/Fig-7]. The Patient was advised to visit the gynaecologist for the treatment of a simple ovarian cyst and referred to a physician for intracranial calcification of falx cerebri.
a) H&E stained lesional tissue showing keratinised stratified squamous epithelium (X100); b) H&E stained tissue showing corrugated epithelium (arrow mark) (X40); c) H&E stained tissue showing proliferative epithelium, underlying connective tissue showing moderate inflammatory cell infiltrate (X100); d) H&E stained tissue showing odontogenic epithelium showing tall columnar cell tombstone pattern (X400).
Postoperative follow-up radiograph showing the formation of bone at the peripheries of the cystic cavity.
Discussion
The autosomal dominant syndrome called GGS also referred to as basal cell nevus syndrome [1]; or nevoid basal cell carcinoma syndrome or gorlin syndrome [2,3] with the tendency to raise neoplasms and developmental anomalies [4]. Aberrations in the long arm of chromosome 9 (q22.3q31) are recognised pathogenesis of GGS [5]. Jarish and White were the first to describe this syndrome, in 1894 [6]. In 1953, Gross presented a case with GGS [7]. Gorlin and Goltz in 1950 were recognised with the triad of multiple epitheliomas, odontogenic keratocyst, and bifurcated ribs [8]. Rayner CR et al., modified the criteria for diagnosis and states that keratocysts had to appear in combination with calcification in the flax cerebri or pits on palmar and plantar [9]. In the general population, 1 in 50,000 to 150,000 is found with GGS [10] with no gender predilection. The clinical features appear in the age between the first to the third decade of life. According to literature, a clinical feature of GGS have palmar/plantar pitting in 90% of cases, Multiple Odontogenic keratocysts (75-100%), impacted teeth and ectopic teeth (3%), 37-79% patients have calcification of falx, 3% in tentorium cerebellum. Connected sella turcica present in 21% patients, calcified ovarian cysts (3%), bifid ribs (26%) [11]. In some rare cases, the dentigerous cyst is also accompanying with GGS [12]. Evans and colleagues put in to view the diagnostic criteria for GGS. This criterion was revised by Kimonis VE et al., According to them, the diagnosis of GGS could be established following the presence of two major or one major and two minor criteria [13] [Table/Fig-8]. The present reported case of GGS fulfilled three major features of the GGS viz., odontogenic keratocyst in the jaw, calcified falx cerebri, bifid ribs, palmer pits, and minor criteria of ovarian cyst favours GGS.
Criteria for diagnosis of GGS [12] (Kimonis VE et al. in 1997 [13]).
| Major criteria | Minor criteria |
|---|
| Multiple BCC | Macrocephaly |
| Odontogenic keratocysts | Bridging of the sella turcica |
| Bifid ribs | Hypertelorism |
| Calcification of the falxcerebri | Ovarian fibroma or cardiac fibroma Medulloblastoma |
| Palmar or plantar pits | Cleft lip or palate |
| Positive family history of NBCC | Flame-shaped lucencies |
GGS: Gorlin-goltz syndrome; NBCC: Nevoid basal cell carcinoma; BCC: Basal cell carcinoma
Skeletal abnormalities involved short built, the fusion of two or more digits, cleft hand, absence or underdevelopment of the digits, and even lack of an extremity. The characteristic radiological alteration osteopathia striata showing fine linear striation on the long bones [14]. Based on histopathological studies, parakeratinisation, intramural epithelial remnants, and satellite cysts were found to be more frequent among the GGS than in solitary keratocysts [15]. Some investigation protocols must be followed when we suspect for GGS such as history about any medical problem, Clinical examinations for oral and skin lesions, Radiographs such as PA Chest, OPG, and ovarian ultrasound should be done [16]. [Table/Fig-9] shows published cases of GGS in the last 5 years [10,17-25]. Among the 10 cases studied from 2015 to 2019, 3 patients had basal cell carcinoma, and only one case report mentioned about the positive family history of basal cell carcinoma. All the patients out of 10 showed the presence of Odontogenic keratocyst. On through clinical examination, palmar or plantar pits affect 4 patients, 6% of patients with frontal bossing, 4% patients with hypertelorism. On radiographic examination, 7 patients are present with calcification of falx cerebri, 6 with bifid ribs, only 2 case reports out of 10 mentions about bridging of sella turcica [10,17-25].
Published cases of GG syndrome in last 5 years [10,17-25].
| Author name | Year | Major criteria | Minor criteria |
|---|
| BCC | Odontogenic keratocyst | Calcification of falx cerebri | Bifid ribs | Positive family history of NBCC | Palmer pits | Macrocephaly, frontal bossing | Bridging of the sellaturcica | Cleft lip or palate | Hypertelorism | Ovarian cyst or fibroma, Cardiac fibromas |
|---|
| Ramesh M et al., [10] | 2015 | Absent | Present | Absent | Present | Not mentioned | Absent | Absent | Absent | Absent | Present | Absent |
| Tandon S, et al., [17] | 2016 | Absent | Present | Present | Present | Not mentioned | Absent | Absent | Absent | Absent | Absent | Absent |
| Soufizadeh R and Kazemian M [18] | 2016 | Present | Present | Present | Absent | Not mentioned | Absent | Present | Absent | Absent | Absent | Absent |
| Arshad F [19] | 2016 | Absent | Present | Present | Present | Not mentioned | Absent | Absent | Absent | Absent | Absent | Absent |
| Witmanowski H et al., [20] | 2017 | Present | Present | Present | Absent | Not mentioned | Present | Present | Absent | Absent | Present | Absent |
| Şereflican B et al., [21] | 2017 | Present | Present | Present | Absent | Present | Absent | Present | Absent | Absent | Present | Absent |
| Kumar N et al., [22] | 2017 | Absent | Present | Present | Present | Not present | Present | Present | Present | Absent | Present | Absent |
| Khodaverdi S et al., [23] | 2018 | Absent | Present | Absent | Absent | Not mentioned | Absent | Present | Absent | Absent | Absent | Present |
| Kumar NN et al., [24] | 2018 | Absent | Present | Absent | Present | Not mentioned | Absent | Absent | Present | Absent | Absent | Absent |
| Boos Lima FBDJ et al., [25] | 2019 | Absent | Present | Present | Present | Not mentioned | Present | Present | Absent | Absent | Absent | Absent |
GG: Gorlin-goltz; BCC: Basal cell carcinoma; NBCC: Nevoid basal cell carcinoma
While considering the treatment of Odontogenic keratocyst associated with GGS, complete removal of a bony wall, overlying surface epithelium, and cystic lining if preferred to prevent a recurrence. Sometimes keratocyst can be locally invasive aggressive so early diagnosis and management is helpful for the better outcome [18,26,27].
Conclusion(s)
The Gorlin-Goltz Syndrome (GGS) must be considered in all patients with multiple odontogenic keratocysts. Imaging evaluation with OPG, AP Skull and PA chest radiograph are the important basic radiograph required along with the systematic evaluation of the patient for skin lesions, digital, limb and thoracic bony abnormality, endocrine and family history. These patients should be followed for a long time with proper medical care and genetic counselling.
GGS: Gorlin-goltz syndrome; NBCC: Nevoid basal cell carcinoma; BCC: Basal cell carcinoma
GG: Gorlin-goltz; BCC: Basal cell carcinoma; NBCC: Nevoid basal cell carcinoma
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: May 14, 2020
Manual Googling: Oct 08, 2020
iThenticate Software: Nov 25, 2020 (11%)
[1]. DeAmezaga AO, Arregui OG, Nuño SZ, Sagredo AA, Urizar JM, Gorlin-Golltzsyndrome: Clinocopathological aspectsMed Oral Pathol Oral Cir Bucal 2008 13(6):E338-43. [Google Scholar]
[2]. Gu XM, Zhao HS, Sun LS, Li TJ, PTCH mutations in sporadic and Gorlin-syndrome-related odontogenickeratocystsJ Dent Res 2006 85(9):859-63.10.1177/15440591060850091616931872 [Google Scholar] [CrossRef] [PubMed]
[3]. Yang XR, Pfeiffer RM, Goldstein AM, Influence of glutathione-S-transferase (GSTM1, GSTP1, GSTT1) and cytochrome p450 (CYP1A1, CYP2D6) polymorphisms on numbers of basal cell carcinomas (BCCs) in families with the naevoid basal cell carcinoma syndromeJ Med Genet 2006 43(4):e1610.1136/jmg.2005.03500616582078 [Google Scholar] [CrossRef] [PubMed]
[4]. Yamamoto K, Yoshihashi H, Furuya N, Adachi M, Ito S, Tanaka Y, Further delineation of 9q22 deletion syndrome associated with basal cell nevus (Gorlin) syndrome: Report of two cases and review of the literatureCongenit Anom 2009 49(1):08-14.10.1111/j.1741-4520.2008.00212.x19243411 [Google Scholar] [CrossRef] [PubMed]
[5]. Acocella A, Sacco R, Bertolai R, Sacco N, Genetic and clinicopathologic aspects of Gorlin-Goltz syndrome (NBCCS): Presentation of two case reports and literature reviewMinerva Stomatol 2009 58(1-2):43-53. [Google Scholar]
[6]. Jawa DS, Sircar K, Somani R, Grover N, Jaidka S, Singh S, Gorlin-Goltz syndromeJ Oral Maxillofac Surg Med Pathol 2009 13(2):89-92.10.4103/0973-029X.5767721887009 [Google Scholar] [CrossRef] [PubMed]
[7]. Howell J, Caro M, The basal-cell nevus: its relationship to multiple cutaneous cancers and associated anomalies of developmentArch Dermatol 1982 118(10):813-23.10.1001/archderm.1982.016502201170176753760 [Google Scholar] [CrossRef] [PubMed]
[8]. Gorlin R, Goltz R, Multiple nevoid basal-cell epithelioma, jaw cysts and bifid rib. A syndromeN Engl J Med 1960 262:908-12.10.1056/NEJM19600505262180313851319 [Google Scholar] [CrossRef] [PubMed]
[9]. Rayner CR, Towers JF, Wilson JS, What is Gorlin’s syndrome? The diagnosis and management of the basal cell naevus syndrome, based on a study of thirty-seven patientsBr J Plast Surg 1977 30(1):62-67.10.1016/S0007-1226(77)90037-6 [Google Scholar] [CrossRef]
[10]. Ramesh M, Krishnan R, Chalakkal P, Paul G, Goltz-Gorlin Syndrome: Case report and literature reviewJ Oral Maxillofac Pathol 2015 19(2):26710.4103/0973-029X.16455726604511 [Google Scholar] [CrossRef] [PubMed]
[11]. Shimada Y, Non-syndromic familial keratocystic odontogenic tumour: A rare case report in Japanese identical twinsJCDR [Internet] 2016 [cited 2020 Aug 22] 10.7860/JCDR/2016/19411.828927656582 [Google Scholar] [CrossRef] [PubMed]
[12]. Pol CA, Ghige SK, Kalaskar RR, Gosavi SR, Gorlin Goltz syndrome: A rare case reportContemp Clin Dent 2013 4(4):547-550.10.4103/0976-237X.12308524403808 [Google Scholar] [CrossRef] [PubMed]
[13]. Kimonis VE, Goldstein AM, Pastakia B, Yang ML, Kase R, DiGiovanna JJ, Clinical manifestations in 105 persons with nevoid basal cell carcinoma syndromeAm J Med Genet 1997 69(3):299-308.10.1002/(SICI)1096-8628(19970331)69:3<299::AID-AJMG16>3.0.CO;2-M [Google Scholar] [CrossRef]
[14]. Garg P, Karjodkar F, Garg SK, Gorlin-goltz syndrome-case report Clin Diag Res 2011 5:393-95. [Google Scholar]
[15]. Lo Muzio L, Nevoid basal cell carcinoma syndrome (Gorlin syndrome)Orphanet J Rare Dis 2008 3:3210.1186/1750-1172-3-3219032739 [Google Scholar] [CrossRef] [PubMed]
[16]. Ljubenović M, Ljubenović D, Binić I, Jovanović D, Stanojević M, Gorlin-Goltz syndromeActa Dermatovenerol Alp Pannonica Adriat 2007 16(4):166-69. [Google Scholar]
[17]. Tandon S, Chauhan Y, Sharma M, Jain M, Gorlin-goltz syndrome: A rare case report of an 11-year-old childInt J Clin Pediatr Dent 2016 9(3):264-68.10.5005/jp-journals-10005-137427843260 [Google Scholar] [CrossRef] [PubMed]
[18]. Soufizadeh R, Kazemian M, Goltz-Gorlin Syndrome: Report of two casesAnn Clin Case Rep 2016 1:1205 [Google Scholar]
[19]. Arshad F, Syndromic odontogenic keratocyst: A case report and review of literatureJ Int Soc Prevent Communit Dent 2016 6(1):84-88.10.4103/2231-0762.17541427011939 [Google Scholar] [CrossRef] [PubMed]
[20]. Witmanowski H, Szychta P, Błochowiak K, Jundziłł A, Czajkowski R, Basal cell nevus syndrome (Gorlin-Goltz syndrome): Genetic predisposition, clinical picture and treatmentPostepy Dermatol Alergol 2017 34(4):381-87.10.5114/ada.2017.6932328951717 [Google Scholar] [CrossRef] [PubMed]
[21]. Şereflican B, Tuman B, Şereflican M, Halıcıoğlu S, Özyalvaçlı G, Bayrak S, Gorlin-Goltz syndromeTurk Pediatri Ars 2017 52(3):173-77.10.5152/TurkPediatriArs.2017.299229062253 [Google Scholar] [CrossRef] [PubMed]
[22]. Kumar N, Tewary S, Zope S, Patel J, Vande A, Dental, dermatological and radiographic findings in a case of Gorlin-Goltz Syndrome: Report and reviewPan Afr Med J 2017 27:96doi: 10.11604/pamj.2017.27.96.1202510.11604/pamj.2017.27.96.1202528819517 [Google Scholar] [CrossRef] [PubMed]
[23]. Khodaverdi S, Nazari L, Mehdizadeh-Kashi A, Vahdat M, Rokhgireh S, Farbod A, Conservative management of ovarian fibroma in a case of gorlin-goltz syndrome comorbid with endometriosisInt J Fertil Steril 2018 12(1):88-90. [Google Scholar]
[24]. Kumar NN, Padmashree S, Jyotsna TR, Shastry SP, Gorlin-Goltz Syndrome: A rare case reportContemp Clin Dent 2018 9(3):478-83. [Google Scholar]
[25]. Boos Lima FBDJ, Viana APC, Lima LHF, Ribeiro BC, Dutra CEA, Stabile GAV, A rare case of Gorlin-Goltz Syndrome in childrenCase Rep Dent 2019 2019:160878310.1155/2019/160878331934460 [Google Scholar] [CrossRef] [PubMed]
[26]. Gadbail AR, Hande A, Chaudhary M, Nikam A, Gawande M, Patil S, Tumor angiogenesis in keratocystic odontogenic tumor assessed by using CD-105 antigen: Tumor angiogenesis in keratocystic odontogenic tumorJ Oral Pathol Med 2011 40(3):263-69.10.1111/j.1600-0714.2010.00962.x20969632 [Google Scholar] [CrossRef] [PubMed]
[27]. Gadbail AR, Mankar Gadbail MP, Hande A, Chaudhary MS, Gondivkar SM, Korde S, Tumor angiogenesis: role in locally aggressive biological behavior of ameloblastoma and keratocystic odontogenic tumorHead Neck-J Sci Spec 2013 35(3):329-34.10.1002/hed.2296022431258 [Google Scholar] [CrossRef] [PubMed]