Salvage of Failed Endovascular Management of Internal Carotid Artery Injury during Endoscopic Endonasal Pituitary Surgery
Chandra Veer Singh1, Shraddha Jain2, Sagar Gourkar3, Sandeep Iratwar4
1 Assistant Professor, Department of E.N.T., J.L.N. Medical College, Sawangi, Wardha, Maharastra, India.
2 Professor, Department of E.N.T., J.L.N. Medical College, Sawangi, Wardha, Maharastra, India.
3 Assistant Professor, Department of E.N.T., J.L.N. Medical College, Sawangi, Wardha, Maharastra, India.
4 Professor, Department of Neurosurgery, J.L.N. Medical College, Sawangi, Wardha, Maharastra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Chandra Veer Singh, M5-10, Meghdoot Building, Paloti Road, Sawangi Meghe, Wardha, Maharastra, India.
E-mail: cheer7us@yahoo.com
Rupture of Internal Carotid Artery (ICA) during trans-sphenoidal surgery can have high morbidity, as it results in altered mental status, stroke or cranial nerve palsies or is fatal for the patient as well. Hereby, Authors describe a case of 23-year-old female who underwent trans-sphenoidal surgery for recurrent pituitary macroadenoma. Removal of the pituitary tumour under general anaesthesia resulted in a bleeding pseudoaneurysm. Distal access catheter across the bleeding pseudoaneurysmal segment of right ICA was made and embolisation of the bleeding pseudoaneurysmal segment was done by placing stent graft. Then check angiogram was performed, which showed that significant embolisation was not achieved. Since, stent graft was unsuccessful to control bleeding, a decision was taken to perform neck dissection to clamp and control the ICA in the neck. Part of the procedure was to harvest a part of vastus lateralis muscle (1 cm × 0.5 cm), crushing it and mixing it with alternating layers of fibrin sealant. This mixture was put over the injured site for better clotting effect. The patient tolerated the procedure well, was shifted to the Intensive Care Unit and vitals were stable thereafter. There are very few instances in published literature which describe the repair of injured ICA using muscle and fibrin sealant. The present case highlights the importance of executing urgent and innovative techniques to control bleeding ICA.
Endovascular treatment, Internal carotid artery rupture, Stent graft, Transsphenoidal surgery
Case Report
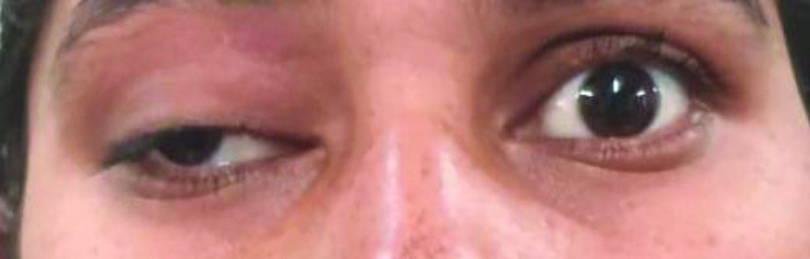
A 23-year-old female was admitted in the neurosurgery ward with complaints of intermittent headache and pain in the right eye in the past two months. She also complained of loss of vision in the right eye with the blurring of vision in a left eye. Patient had no history of fall, vomiting, convulsions or fever and her past medical history was insignificant as well. Her general physical examination and systemic examination were within normal limits except for the presence of ptosis in the right eye [Table/Fig-1].
Pre-operative image of the patient showing ptosis of right eye.
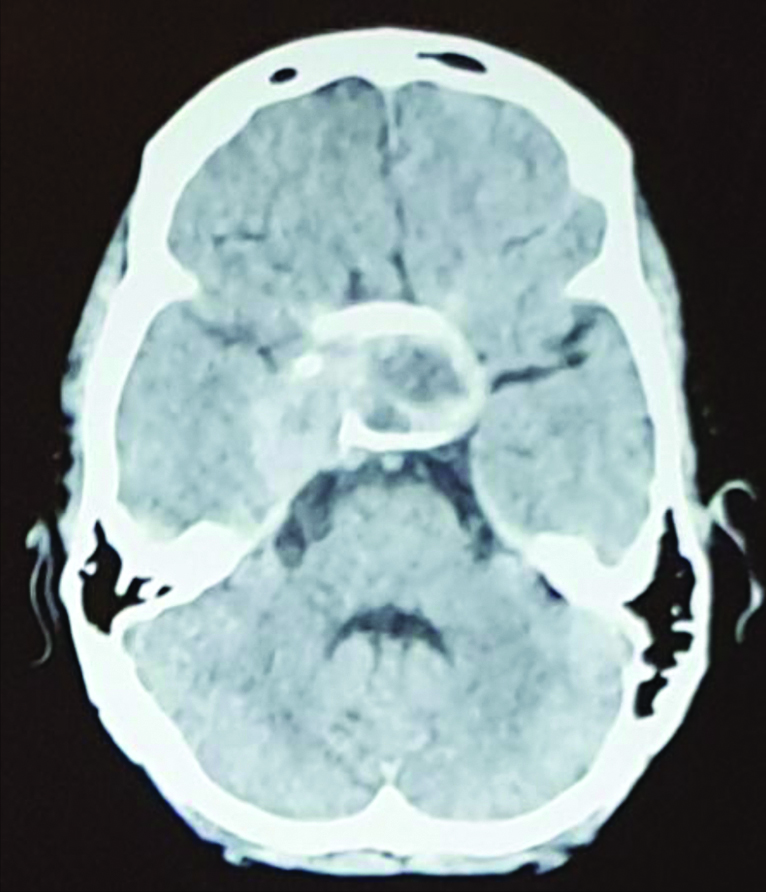
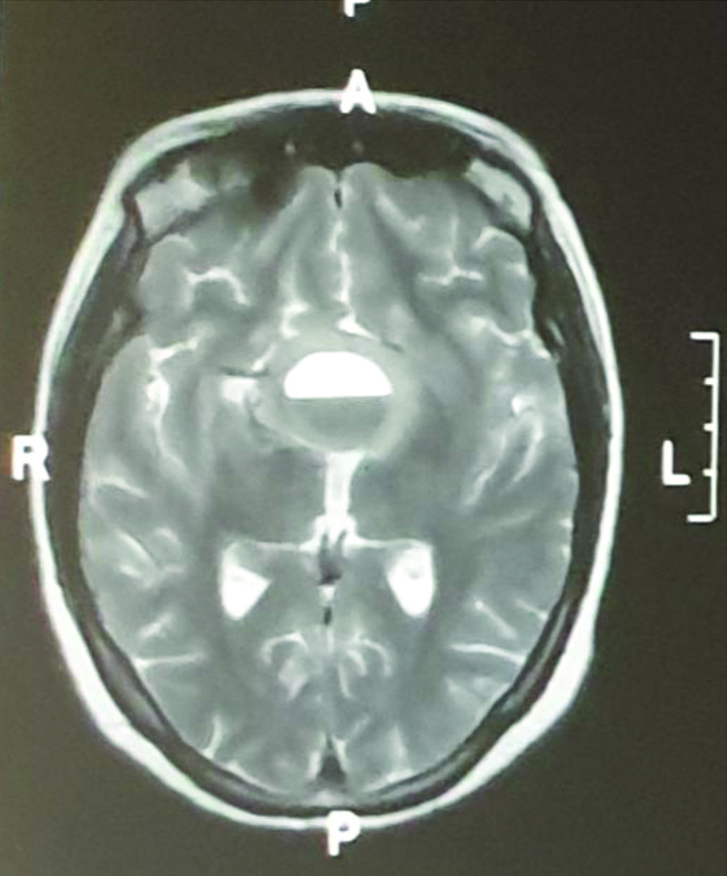
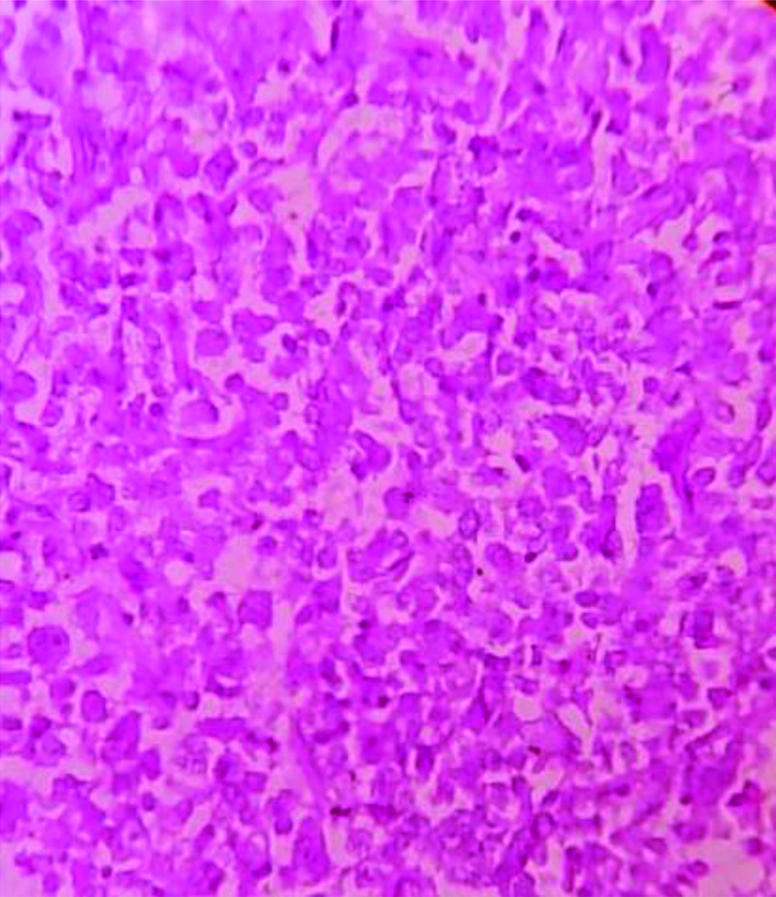
Computerised Tomography (CT) scan brain revealed a mixed density lesion noted in sellar and suprasellar region with a fluid level measuring approximately 43×35×38 mm extending to the right cavernous sinus [Table/Fig-2]. Magnetic Resonance Imaging (MRI) brain showed a well-defined lobulated mass lesion in the sellar and suprasellar region with a fluid level measuring approximately 43×35×35 mm and extended into the surrounding regions [Table/Fig-3]. A small hypodense area was also noted in right gangliocapsular region which was suggestive of previous surgery. Thus, a diagnosis of recurrent pituitary macroadenoma was made. After discussing the treatment options with the patient, she underwent endoscopic transnasal transpheniodal removal of the pituitary tumour under general anaesthesia. Part of the pituitary tumour was removed and sent for histopathology [Table/Fig-4]. However a few minutes later, bleeding was noted from a post-traumatic pseudoaneurysm. Authors observed blood leakage from the right supraclinoid ICA. We tried to stop bleeding using gel foam and roller pack, but the leak continued and approximately 2.8 litres of blood loss was noted. Immediately, the patient was given blood transfusions, colloid and inotropic agents, while shifting her to an angiography table under the same General Anaesthesia (GA). Under all aseptic precautions and local anaesthesia, right femoral artery access was taken, and selective angiogram of Common Carotid Artery (CCA) and ICA was taken, which revealed bleeding pseudoaneurysm from the right ICA. Thereafter, using triaxil system over the Traxcess guide wire and Terumo Progreat Microcatheter advanced co-axially through ACE-68, manufactured by Micro Vention company, distal access catheter across the bleeding pseudoaneurysmal segment of right ICA was made and embolisation of the bleeder pseudoaneurysmal segment was done by placing stent graft (Abbott Vascular Graftmaster 3.5 mm×16 mm). Then check angiogram was performed which showed that significant embolisation was not achieved [Table/Fig-5] and the surgical route was decided.
Preoperative CT Brain axial view mixed density lesion noted in sellar and suprasellar region.
Magnetic Resonance Imaging (MRI) brain showed a well-defined lobulated mass lesion in sellar and suprasellar region with fluid level.
Histopathology image show cellular monographism of acidophilic cells placed in cords and sheets (Haematoxylin and Eosin, 10X).
Intraoperative failed endovascular stunting.
A horizontal upper neck skin incision was made from the anterior border of the Sternocleidomastoid Muscle (SCM) to the midline of the neck just two fingers below the angle of the mandible. Subplatysmal flap was elevated upto the lower border of the mandible and inferiorly to the omohyoid muscle. The External Jugular Vein and Great Auricular Nerve identified. Dissection followed the medial structure of SCM and deeper structures including Internal Jugular Vein (IJV) and CCA were exposed used retractors to pull IJV and SCM and ICA was identified, which was clamped to control bleeding. A part of vastus lateralis muscle 1×0.5 cm was taken crushed and mixed with alternating layers of fibrin sealant (Tisseel glue, Baxter India). Clamp pressure over the right side of ICA and nasal packing was carried out with saline-soaked gauze which stopped the active bleeding. This crushed part of vastus lateralis muscle was sent to the pseudoaneurysm endonasally. After 20 minutes using the two-surgeon four-hand technique, the nasal pack was removed and there was no bleeding. A definitive packing with crushed muscle tissue from the vastus lateralis and a surgical combination was put over the injured site for better clotting effect and it was reinforced and compressed with gel foam and saline-soaked long ribbon gauze. The patient tolerated the procedure well, was shifted to the Intensive Care Unit and vitals were stable thereafter. [Table/Fig-6] shows a post-operative image of neck Dissection. Post-operative CT Angiography done on the same day after three hours revealed well-mixed density lesion noted in sellar and suprasellar region with fluid level measuring approx. 43×35×38 cm extending to the right cavernous sinus. Bony defects or dehiscence has been seen in roof of sphenoid sinus nasal septum inter ethmoid and intersphenoid septum. CT Brain was done which showed no early ischaemic changes in brain parenchyma with no active leak of contrast or extravasations seen [Table/Fig-7]. Nasal pack removed under GA on fifth post-operative days with no re-bleeding from the injured site. Post-procedure, antiplatelets or heparin were avoided due to the fear of re-bleeding. The patient received intravenous fluids, broad spectrum antibiotic coverage with Injection Piperacillin 4.5 gm IV TDS, steroids, pain control with injection paracetamol and intensive physiotherapy. The patient was extubated after 24 hours, neurologically intact and discharged on the seventh post-operative day. [Table/Fig-8] shows a follow-up image of the patient after one month. Consent was obtained from the patient for the use of images.
Postoperative pic of neck dissection.

Postoperative CT brain axial view day one.
Follow-up picture of patient after one month.

Discussion
Intraoperative injuries of the ICA have been reported to occur in up to 3.8% of the patients in a large case series [1] and have a high morbidity and mortality when they occur during trans-sphenoidal surgery [2]. A ten-year data reported that trans-sphenoidal surgery is followed by an endovascular intervention in about 0.1% of the cases [3]. Factors which tend to increase the risk of ICA injury include acromegaly, revision surgery, history of radiation therapy, bromocriptine therapy, calcification lesions and carotid artery anomalies [4]. In literature, mainly four kinds of covered stents i.e., autologous vein-covered stents, Symbiot-covered stent, Jostent-covered stent, and carotid Wallstent have been described. Autologous vein-covered stents were first used for the treatment of native and saphenous vein graft coronary perforation [5]. Instances of iatrogenic ICA injury can be prevented by careful preoperative planning and understanding the anatomy of carotid arteries [6].
Micro-doppler has been reported to offer real-time localisation of carotid arteries, which can help the surgeon to adjust intraoperatively. Depending on the collateral flow, one can consider either sacrificing or preserving the carotid. In the latter case an endovascular procedure is needed. There are numerous endovascular techniques like coil embolisation, stent-assisted coiling, covered stent placement, and onyx embolisation, which can be chosen by the interventional radiologist depending on their years of clinical experience and patient characteristics [6].
The Symbiot-covered stent manufacturer by Boston Scientific is an appropriate small nitinol self-expandable stent, which was originally designed for vascular use in coronary saphenous vein grafts [7]. Jostent-covered stent (Abbott Vascular) is a balloon-expandable stent with an ultrathin layer of Polytetrafluoroethylene (PTFE) placed between two high grade surgical steel stents [7]. The carotid Wallstent (Boston Scientific) is used for extracranial carotid diseases. The choice of stent varies with the preferences of the surgical team and needs to be best suited for patient needs.
Unfortunately, there is no clear protocol or consensus about the use of any particular technique. In our patient, embolisation of the bleeder pseudoaneurysmal segment of ICA was done by placing a stent graft. Saatci I et al., used stent graft in the parent vessel to exclude the intracranial aneurysm sac from circulation in 25 ICA aneurysms. They reported no technical difficulties, which included dissection and perforation of the vessel, or thromboembolism. Also, no mortality or morbidity developed during or after the procedure, including the follow-up period [8]. Although, this covered stent is not designed for intracranial use which may raise some concern exists regarding its long-term safety and efficacy, Li MH et al., reported the successful use of a new covered stent, designed for the intracranial vasculature, in eight patients with intracranial carotid pseudoaneurysm. They used the Willis stent covered with PTFE on the abluminal side and with an outer diameter of 3.8 F (12.7 mm) is specifically designed for use in the intracranial vasculature [9]. Shakir HJ et al., reported a case of 61-year-old woman with clival tumour resected by trans-shpenoidal approach having right ICA injury. The patient underwent repeated failed endovascular Jostent Graftmaster stenting, followed by multiple balloon attempts and Pipeline Embolisation Devices (PED) was used twice. At one-month follow-up, central nervous system evaluation of the patient remained was with in normal limits and no neurologic complications were reported. The authors used PED as the Jostent did not fully oppose the vessel wall around an adjacent curve despite being delivered across the injured segment, resulting in reduced but continued extravasation [10].
Saatci I et al., used stent graft in the parent vessel to exclude the intracranial aneurysm sac from circulation in 25 ICA aneurysms [8]. Local compression of bleeding ICA followed by cautery, sealants with or without crushed muscle, use of clips, and endovascular stent placements have been described as possible rescue options [11]. Using haemostatic agents may prove ineffective [12]. Including crushed vastus lateralis muscle patch helped in obtaining primary haemostasis and also maintained normal vessel architecture [13]. However, it may redirect the bleeding posteriorly or upward toward the intracranial space. Also, muscle and glue tamponade could occlude the ICA, causing ischaemia [13].
Conclusion(s)
Early recognition and management is the key to prevent worsened outcomes in ICA bleed. Ours is the first reported case in which to control ICA bleeding, neck dissection was done to clamp and control the ICA in the neck. A part of crushed vastus lateralis muscle fibres and fibrin sealant was sent to the pseudoaneurysm endonasally. So, muscle fibres and fibrin sealant successfully stopped ICA bleeding after a covered stent failed to manage acute vascular injury resulting from trans-sphenoidal surgery for a pituitary tumour. With advances of endovascular techniques’ new materials and approaches are being developed to improve the ease of stenting and success rate. Future studies are needed to refine the endovascular techniques and to compare their clinical outcomes.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 29, 2020
Manual Googling: Oct 14, 2020
iThenticate Software: Nov 25, 2020 (19%)
[1]. Cappabianca P, Cavallo LM, Colao A, de Divitiis E, Surgical complications associated with the endoscopic endonasal transsphenoidal approach for pituitary adenomasJ Neurosurg 2002 97(2):293-98.10.3171/jns.2002.97.2.029312186456 [Google Scholar] [CrossRef] [PubMed]
[2]. Oskouian RJ, Kelly DF, Laws ER Jr, Vascular injury and transsphenoidal surgeryFront Horm Res 2006 34:256-78.10.1159/00009158616474224 [Google Scholar] [CrossRef] [PubMed]
[3]. Brinjikji W, Lanzino G, Cloft HJ, Cerebrovascular complications and utilization of endovascular techniques following transsphenoidal resection of pituitary adenomas: A study of the Nationwide Inpatient Sample 2001-2010Pituitary 2014 17:430-35.10.1007/s11102-013-0521-124048654 [Google Scholar] [CrossRef] [PubMed]
[4]. Park YS, Jung JY, Ahn JY, Kim DJ, Kim SH, Emergency endovascular stent graft and coil placement for internal carotid artery injury during transsphenoidal surgerySurgical Neurology 2009 72(6):741-46.10.1016/j.surneu.2009.05.00319604552 [Google Scholar] [CrossRef] [PubMed]
[5]. Van Nieuwenhove Y, Van den Brande P, Van Tussenbroek F, Debing E, Von Kemp K, Iatrogenic carotid artery pseudoaneurysm treated by an autologous vein-covered stentEur J Vasc Endovasc Surg 1998 16(3):262-65.10.1016/S1078-5884(98)80230-X [Google Scholar] [CrossRef]
[6]. Shah N, Deopujari CE, Endoscopic transsphenoidal surgery: A practical guide 2019 ThiemeISBN 978 9 38825 723 7 pp. 11, 152 [Google Scholar]
[7]. Maras D, Lioupis C, Magoufis G, Tsamopoulos N, Moulakakis K, Andrikopoulos V, Covered stent-graft treatment of traumatic internal carotid artery pseudoaneurysms: A reviewCardiovasc Intervent Radiol 2006 29(6):958-68.10.1007/s00270-005-0367-716897263 [Google Scholar] [CrossRef] [PubMed]
[8]. Saatci I, Cekirge HS, Ozturk MH, Arat A, Ergungor F, Sekerci Z, Treatment of internal carotid artery aneurysms with a covered stent: Experience in 24 patients with mid-term follow-up resultsAm J Neuroradiol 2004 25(10):1742-49. [Google Scholar]
[9]. Li MH, Li YD, Gao BL, Fang C, Luo QY, Cheng YS, A new covered stent designed for intracranial vasculature: Application in the management of pseudoaneurysms of the cranial internal carotid arteryAm J Neuroradiol 2007 28(8):1579-85.10.3174/ajnr.A066817846216 [Google Scholar] [CrossRef] [PubMed]
[10]. Shakir HJ, Garson AD, Sorkin GC, Mokin M, Eller JL, Dumont TM, Combined use of covered stent and flow diversion to seal iatrogenic carotid injury with vessel preservation during transsphenoidal endoscopic resection of clival tumourSurgical Neurology International 2014 5:8110.4103/2152-7806.13363825024881 [Google Scholar] [CrossRef] [PubMed]
[11]. Valentine R, Boase S, Jervis-Bardy J, Dones Cabral JD, Robinson S, Wormald PJ, The efficacy of hemostatic techniques in the sheep model of carotid artery injuryInternational Forum of Allergy & Rhinology 2011 1(2):118-22.10.1002/alr.2003322287330 [Google Scholar] [CrossRef] [PubMed]
[12]. Paluzzi A, Fernandez-Miranda JC, Tonya Stefko S, Challinor S, Snyderman CH, Gardner PA, Endoscopic endonasal approach for pituitary adenomas: a series of 555 patientsPituitary 2014 17(04):307-19.10.1007/s11102-013-0502-423907570 [Google Scholar] [CrossRef] [PubMed]
[13]. Weidenbecher M, Huk W J, Iro H, Internal carotid artery injury during functional endoscopic sinus surgery and its managementEur Arch Otorhinolaryngol 2005 262(8):640-45.10.1007/s00405-004-0888-815657746 [Google Scholar] [CrossRef] [PubMed]