Dental Implant for a Patient with Narcolepsy: A Case Report
Hani Mawardi1, Yasser Mahfouz2, Siraj Dakhil3, Mohammed Zahran4, Lena Elbadawi5
1 Associate Professor, Department of Oral Diagnostic Sciences, Faculty of Dentistry, King Abdulaziz University, Jeddah, Western, Saudi Arabia.
2 Assistant Professor, Department of Dentistry, Saudi German Hospital, Jeddah, Western, Saudi Arabia.
3 Assistant Professor, Department of Endodontics, Faculty of Dentistry, King Abdulaziz University, Jeddah, Western, Saudi Arabia.
4 Assistant Professor, Department of Prosthodontics, Faculty of Dentistry, King Abdulaziz University, Jeddah, Western, Saudi Arabia.
5 Assistant Professor, Department of Periodontics, Faculty of Dentistry, King Abdulaziz University, Jeddah, Western, Saudi Arabia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Hani Mawardi, 2792 Abdullah IBN Musidah, Jeddah, Western, Saudi Arabia.
E-mail: hmawardi@kau.edu.sa
Narcolepsy is a neurological disorder characterised by cataplexy, sleep paralysis and excessive daytime sleepiness. The literature on dental managements of patients with narcolepsy is lacking with no set guidelines for dental practitioners. A 31-year-old female presented to the dental office with a dull pain related to the maxillary left lateral incisor with Grade 2 mobility and isolated 8 mm periodontal pocket. In addition, there was loss of buccal gingiva with radiographic changes suggestive of caries and fractured crown. The patient had a history of narcolepsy with cataplexy and hypertension controlled with bisoprolol and desvenlafaxine in addition to clonazepam 1 mg/day as needed to prevent episodes of cataplexy. Patient was asked to take 2 mg clonazepam and 600 mg ibuprofen one hour before procedure. The maxillary left lateral incisor was extracted atraumatically and an immediate implant combined with allogenic bone graft and collagen membrane was placed. The procedure was uneventful, and patient left conscious and stable. After three months, the implant was restored with porcelain fused-to-metal crown and followed-up for six months without any complications. This is the first case describing a narcolepsy patient who successfully received a dental implant without developing a cataplexy episode. Clonazepam prophylaxis may be considered prior to dental procedures for similar situations.
Benzodiazepines, Cataplexy, Single tooth
Case Report
A 31-year-old female patient presented to King Abdulaziz University-Faculty of Dentistry, Jeddah, Saudi Arabia complaining of a dull pain related to the maxillary left lateral incisor which had started four weeks prior to the consultation visit. The patient’s medical history was significant for narcolepsy with cataplexy and hypertension controlled with bisoprolol (2.5 mg/day) and desvenlafaxine (50 mg/day). The patient was originally diagnosed with narcolepsy five years ago with 2-4 cataplexy episodes/year and no reported attacks in the last three years. In addition, she was taking clonazepam 1 mg/day at bedtime as needed to prevent or manage acute episodes of cataplexy. As per patient report, the most recent cataplectic attack was three years prior to the consultation visit which had lasted for one minute and was associated with facial weakness and slurred speech. There was no significant allergy history; however, she had been smoking hookah socially for the past four years. Dental history was significant for multiple restorations, root canal therapy and fixed prosthetics treatment without reported complications.
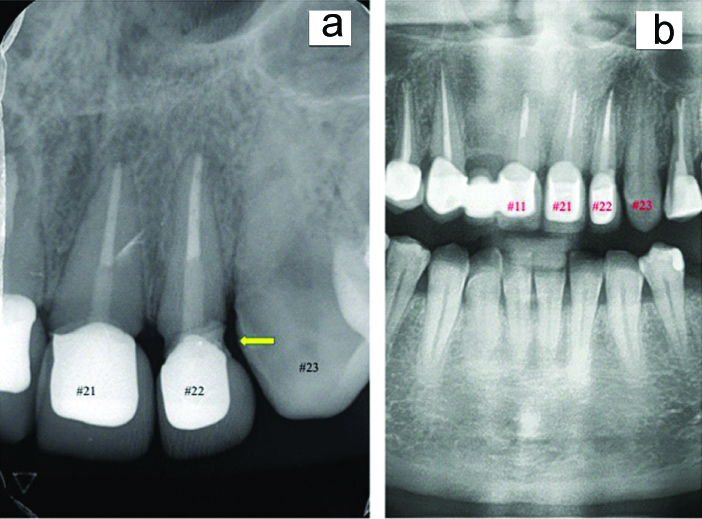
Extraoral examination was non-contributory with no masses or swelling noted. Intraoral examination was significant for mobile maxillary left lateral incisor (Grade 2) which was tender to palpation and vertical percussion. In addition, there was gingival bleeding on probing with respect to the maxillary left lateral incisor. In order to confirm the diagnosis, a periapical and panoramic radiograph was taken and demonstrated maxillary left lateral incisor with root canal treatment to the apex and no periapical radiolucency [Table/Fig-1]. There were radiographic changes noted under the existing crown of the maxillary left lateral incisor and a thin radiolucent line in-between suggestive of caries with crown fracture. Combining patient’s reported history with clinical and radiographic findings; the maxillary left lateral incisor was given a poor prognosis due to insufficient tooth structure and indicated for extraction [Table/Fig-2]. Several treatment options were discussed with the patient and the decision was made to extract the maxillary left lateral incisor and attempt to replace it with an immediate implant.
Radiographic assessment of the existing maxillary incisors on: a) periapical; and b) panoramic radiographs showing completed root canal treatment to the apex of maxillary anterior teeth with porcelain-fixed to metal crowns except the left maxillary canine and no periapical radiolucency. In addition, there were radiographic changes under the existing crown and thin radiolucent line in-between suggestive of caries with crown fracture (yellow arrow).
Clinical assessment of patient’s smile line.

As a part of the comprehensive evaluation process, the patient was referred for medical/neurological consultation based on her underlying diagnosis of narcolepsy and hypertension. A detailed report describing the proposed dental treatment plan was provided to the neurologist and requested recommendations based on the patient’s current status. Afterward, the case was discussed among the treating team considering all the potential risks. Due to lack of literature on dental management for narcolepsy patients, a plan was generated based on known features of narcolepsy and triggers for cataplexy in addition to anticipated emergencies in the dental office. This plan included doubling the current dose of clonazepam (to a total of 2 mg) to reduce the risk of emotional excitement in addition to 600 mg ibuprofen for the purpose of pre-emptive analgesia effect to be taken one hour before procedure.
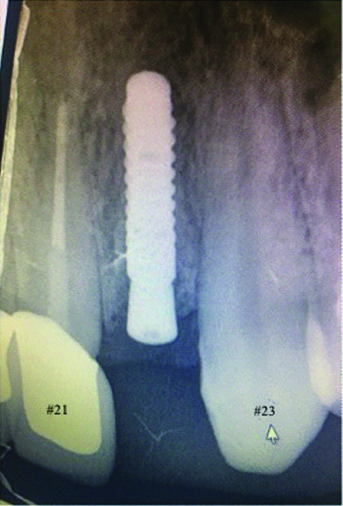
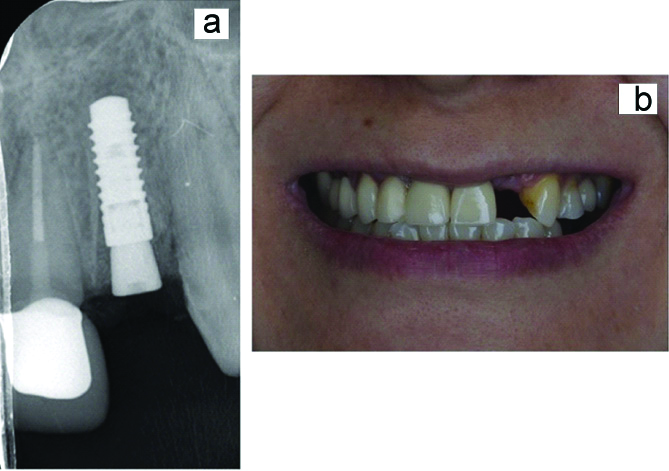
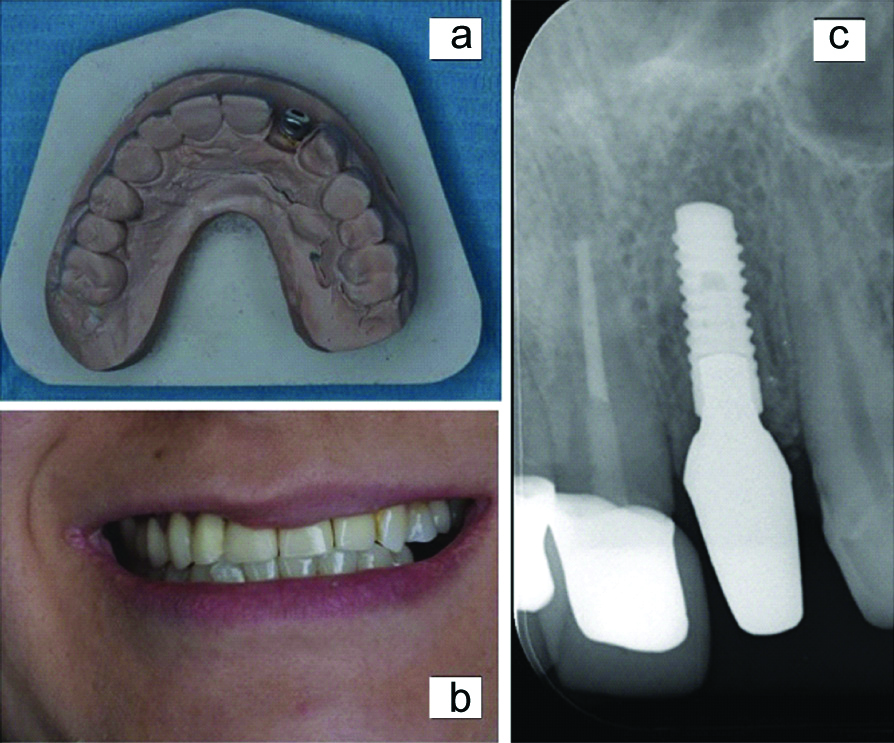
On the day of the procedure, an oxygen tank with a fitted mask was set and ready in the room to be used if a cataplexy episode with respiratory suppression to take place to maintain an optimum flow of oxygen within the patient system. Following explanation of the procedure risks and potential complications in addition to signing a consent form, extraction of maxillary left lateral incisor was completed atraumatically with 2% lidocaine was 100,000 epinephrine using a periotome. Assessment of the maxillary left lateral incisor extraction socket revealed three intact walls and dehiscence of the buccal plate of bone with more than 5 mm of interproximal bone height. Considering the following factors: a stable medical status; no significant smoking history; 2 mm of socket wall width; and thick gingival biotype, a decision was made to place an immediate implant Straumann® bone level 3.3×10 mm at 2 mm below crestal bone level with primary stability and covered with covering screw. The procedure was combined with demineralized freeze-dried allogenic bone graft (CenoBone®, UK) and resorbable collagen membrane (Bioteck®, UK) to regenerate the missing buccal plate. The surgical site was sutured with primary intention through horizontal mattress and simple interrupted sutures using polyglactin material (5-0 and P3 needle; Ethicon, Ohio, USA) to achieve haemostasis [Table/Fig-3]. The procedure was uneventful, and patient left conscious and stable. After two weeks, the patient presented for follow-up on the surgical site which continued to heal without signs of infection. After three months, the implant site was exposed for Stage II and implant osseointegration was assessed using mobility and response to percussion [Table/Fig-4]. The implant was restored with porcelain-fused-to-metal crown in the following two weeks [Table/Fig-5]. The patient was followed-up for six months without any complications or signs of peri-implant mucositis.
Periapical radiograph of the immediate implant after extraction of hopeless maxillary left lateral incisor assisted with a periotome.
At 3-months follow-up, the implant was assessed for osseointegration radiographically and clinically (a and b).
A porcelain-fused to metal crown was constructed on a cast (a) and delivered (b and c).
Discussion
Narcolepsy is a disabling neurological disorder characterised by cataplexy, sleep paralysis and excessive daytime sleepiness which may exhibit significant psychosocial stress on affected subjects [1]. It is classified as hypersomnia from a central origin with a pathogenesis involving abnormality in the Rapid Eye Movement (REM)- inhibiting sleep mechanism [2]. Cataplexy is an acute event often associated with narcolepsy described as intermittent loss of voluntary muscle tone associated with REM, likely to be precipitated by extreme excitements or stressful emotions [2]. According to the International Classification of Sleep Disorders (ICSD-3), narcolepsy can present with cataplexy (Type 1) or without (Type 2) [3]. The proposed mechanism includes destruction of hypocretin peptide-producing neurons in the hypothalamus causing reductions of cerebrospinal fluid hypocretin resulting in narcolepsy with cataplexy (Type 1) [4].
The overall reported prevalence of narcolepsy is 79.4/100,000 persons in which 65.4/100,000 are without cataplexy and 14.0/100,000 had at least one cataplexy episode [5]. Demographically, narcolepsy has been reported 50% greater in females compared to males’ population with age range of 21-30 years [6]. Due to the nature of this disease, significant impairment of different life aspects including social relationships, career in addition to increase in traumatic accident rates are anticipated [6]. As of today, no cure exists for narcolepsy. However, management of symptoms and prevention of cataplectic attacks are key [4]. Non-pharmacological approach to manage narcolepsy includes reinforcement of proper sleep hygiene and modification of lifestyles [6]. More advanced cases may require immunomodulatory or hypocretin replacement therapies (neural stimulant) as well as avoiding extreme excitement events which can act as triggers [6].
In general, including patient in the decision-making process for best management approach is crucial in order to address the most disruptive symptoms with major impact on lifestyle. For most cases, patients with narcolepsy are able to maintain a balanced daily routine and keeping the disease under control [4]. Often, patients with narcolepsy may experience dental problems requiring interventions by dental professionals. Therefore, dental practitioners should be aware of potential complications associated with delivery of dental care to narcolepsy patients. Out of all potential complications, sudden sleepiness and cataplexy attacks may be the most serious narcolepsy emergencies that the dentist should be aware of. This dental emergency is more likely to be triggered by laughter, positive or negative emotions (e.g., fear and anxiety) and stressful events related to dental procedures experienced by patients in the dental office [7]. These acute episodes usually present as complete or partial loss of neck, face or whole body muscles tones causing slurred speech, facial twitching and jerky tremor of the head [4]. Often, the experienced weakness may spread cephalo-caudally in few seconds leading to body collapse on the floor with mouth open and eyes shut [4]. Typically, this acute episode lasts for 10 seconds with a full recovery taking place in few minutes in which the patient’s awareness is completely preserved. During this phase, only extraocular and respiratory muscles are functional [7].
The relation between narcolepsy and oral health has been under-studied. One reason could be the fairly low prevalence rate of narcolepsy and/or under-reporting in the dental literature [5]. In the current case, an immediate dental implant was indicated which is a common dental procedure performed to replace missing teeth with high success rate [8]. However, patients’ fear and anxiety in relation to this procedure are prevalent among the general population [9]. The most common reason for this psychological challenge is the exposure to pre-procedural audiovisual information from variable resources [9]. Therefore, the risk of developing a cataplectic attack during the implant procedure was considered for the current case [10]. Even with the last reported cataplectic attack by patient was three years prior to the implant procedure, the potential risk of a new episode to be triggered on the dental chair was discussed among the medical and dental team in charge of the patient. Due to lack of literature on best practice to approach similar cases, the decision was made to increase the dose of clonazepam (total of 2 mg) prophylactically based on available reports of its use in narcolepsy patients [11]. Clonazepam is a benzodiazepine with antiepileptic and anxiolytics effects used commonly to reduce patient’s anxiety and decrease the risk of associated-emotional trigger [12]. Historically, clonazepam has been considered as a prophylactic option for managing cataplexy which was replaced by other agents due to its potential risk for dependence [12]. It is a common sedative with an acceptable safety profile and multiple indications in the dental field including management of burning mouth syndrome cases with a dose ranging between 0.5-2 mg/day [11]. In addition to clonazepam, ibuprofen was given one hour before the procedure in order to achieve pre-emptive analgesia which is a common practice among dental practitioners to reduce the patient’s anticipated pain experience [13].
Another potential effect of narcolepsy on oral health is the effect of active, prescribed medications. Considering the main goal of pharmacological therapy in narcolepsy is to address symptoms of excessive day time sleepiness, sleep fragmentation and cataplexy, most of patients are on polypharmacy of medications. These include wake-promoting agents (e.g., modafinil and armodafinil), neural stimulants (e.g., methylphenidate and amphetamines) and Gamma-aminobutyric Acid (GABA) receptor agonist (sodium oxybate) [2]. Some or all of these medications may change the oral environment of patients in different ways. A report by Nordgarden H et al., have demonstrated reduced salivary flow and buffering capacity in a group of 12 narcolepsy patients likely related to prescribed central stimulant medication [14]. Drug interaction is another factor to be considered in the setting of narcolepsy. Combined with anticoagulation agents, antidepressants may increase the risk of internal bleeding in certain patient [15]. Hence, local measures such as haemostatic agents, gel-foam application and additional suturing to minimise the risk of postoperative oral bleeding should be considered [15].
Conclusion(s)
This case describes a 31-year-old female patient with a history of narcolepsy who received an immediate dental implant to replace the maxillary left lateral incisor. This is the first report with a focus on pre-surgical preparation in this population of patients. Clonazepam prophylaxis was found to be safe and may be considered prior to dental procedures for similar cases. We believe that this report will help to better serve patients with this condition and provide different dental treatments in a medically safe environment. Future studies to better understand dental needs and standard of care for narcolepsy patients are warranted.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 06, 2020
Manual Googling: Oct 26, 2020
iThenticate Software: Oct 28, 2020 (2%)
[1]. Bassetti CLA, Adamantidis A, Burdakov D, Han F, Gay S, Kallweit U, Narcolepsy-clinical spectrum, aetiopathophysiology, diagnosis and treatmentNat Rev Neurol 2019 15(9):519-39.10.1038/s41582-019-0226-931324898 [Google Scholar] [CrossRef] [PubMed]
[2]. Morse AM, Narcolepsy in children and adults: A guide to improved recognition, diagnosis and managementMed Sci (Basel) 2019 7(12)10.3390/medsci712010631783668 [Google Scholar] [CrossRef] [PubMed]
[3]. Ruoff C, Rye D, The ICSD-3 and DSM-5 guidelines for diagnosing narcolepsy: Clinical relevance and practicalityCurr Med Res Opin 2016 32(10):1611-22.10.1080/03007995.2016.120864327359185 [Google Scholar] [CrossRef] [PubMed]
[4]. Slowik JM, Collen JF, Yow AG, NarcolepsyStatPearls 2020 Treasure Island (FL) [Google Scholar]
[5]. Scheer D, Schwartz SW, Parr M, Zgibor J, Sanchez-Anguiano A, Rajaram L, Prevalence and incidence of narcolepsy in a US health care claims database, 2008-2010Sleep 2019 42(7)10.1093/sleep/zsz09131004158 [Google Scholar] [CrossRef] [PubMed]
[6]. Khatami R, Luca G, Baumann CR, Bassetti CL, Bruni O, Canellas F, The European Narcolepsy Network (EU-NN) databaseJ Sleep Res 2016 25(3):356-64.10.1111/jsr.1237426809504 [Google Scholar] [CrossRef] [PubMed]
[7]. Mirabile VS, Sharma S, CataplexyStatPearls 2020 Treasure Island (FL) [Google Scholar]
[8]. Howe MS, Keys W, Richards D, Long-term (10-year) dental implant survival: A systematic review and sensitivity meta-analysisJ Dent 2019 84:09-21.10.1016/j.jdent.2019.03.00830904559 [Google Scholar] [CrossRef] [PubMed]
[9]. Camacho-Alonso F, Vilaplana-Vivo J, Caballero-Guerrero PM, Pato-Mourelo J, Sanchez-Siles M, Impact of audiovisual information on anxiety and fear in patients undergoing dental implant treatmentClin Implant Dent Relat Res 2019 21(6):1189-98.10.1111/cid.1285131639265 [Google Scholar] [CrossRef] [PubMed]
[10]. Cohen FL, Nehring WM, Cloninger L, Symptom description and management in narcolepsyHolist Nurs Pract 1996 10(4):44-53.10.1097/00004650-199607000-000088717997 [Google Scholar] [CrossRef] [PubMed]
[11]. Chen Q, Shi Y, Jiang L, Zhou Y, Dan H, Jin X, Management of burning mouth Syndrome: A position paper of the Chinese Society of Oral MedicineJ Oral Pathol Med 2020 49(7):701-10.10.1111/jop.1308232589772 [Google Scholar] [CrossRef] [PubMed]
[12]. Dokkedal-Silva V, Berro LF, Galduroz JCF, Tufik S, Andersen ML, Clonazepam: Indications, side effects, and potential for nonmedical useHarv Rev Psychiatry 2019 27(5):279-89.10.1097/HRP.000000000000022731385811 [Google Scholar] [CrossRef] [PubMed]
[13]. Pereira GM, Cota LO, Lima RP, Costa FO, Effect of preemptive analgesia with ibuprofen in the control of postoperative pain in dental implant surgeries: A randomized, triple-blind controlled clinical trialJ Clin Exp Dent 2020 12(1):e71-e78.10.4317/medoral.5617131976047 [Google Scholar] [CrossRef] [PubMed]
[14]. Nordgarden H, Jensen JL, Arneberg P, Storhaug K, Salivary secretion and oral health in narcolepsy: A pilot studySpec Care Dentist 1996 16(3):128-33.10.1111/j.1754-4505.1996.tb00846.x9084326 [Google Scholar] [CrossRef] [PubMed]
[15]. Komen JJ, Hjemdahl P, Mantel-Teeuwisse AK, Klungel OH, Wettermark B, Forslund T, Concomitant anticoagulant and antidepressant therapy in atrial fibrillation patients and risk of stroke and bleedingClin Pharmacol Ther 2020 107(1):287-94.10.1002/cpt.160331506933 [Google Scholar] [CrossRef] [PubMed]