Prevalence of Fracture of Forearm Bones in Obese and Non-obese Children: A Cross-sectional Study
SP Akshatha1, JB Santhosha2
1 Assistant Professor, Department of Paediatrics, ADI Chunchanagiri Institute of Medical Sciences (AIMS), Mandya, Karnataka, India.
2 Assistant Professor, Department of Orthopaedics, ADI Chunchanagiri Institute of Medical Sciences (AIMS), Bangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. JB Santhosha, Assistant Professor, Department of Orthopaedics, ADI Chunchanagiri Institute of Medical Sciences (AIMS), BG Nagar, Nagamangala (Taluk), Mandya-571448, Karnataka, India.
E-mail: foryourhelp55@gmail.com
Introduction
Through much history of mankind, the overt manifestation of bodyweight gain in children and adults have been considered as a sign of personal health and family wealth and an indicator of the economic prosperity of the society. As developing societies are industrialised and urbanised, the standards of living continued to rise; obesity and weight gain began to pose a growing threat to the health of the citizens.
Aim
To determine the prevalence of forearm bones fracture in obese and non-obese children between age group of 2-15 years.
Materials and Methods
A cross-sectional study was conducted in the Department of Orthopaedics and Paediatrics at Dr BC Roy Post Graduate Institute of Paediatric Science, Kolkata, West Bengal, India from September 2017 to October 2018. Children were classified into obese and non-obese group according to Body Mass Index (BMI). Calculation of BMI was done by the formula BMI=weight (kg)/{height(m)}2. Obese children were determined by the BMI percentile by plotting the BMI number on the appropriate Centers for Diseases Control and Prevention (CDC) BMI-for-age growth chart. Doubtful cases classification was confirmed by the paediatric surgeon. Injury mechanism was graded into three trauma kinetics (direct trauma, slow motion trauma and high motion trauma). The validated paediatric Physical Activity Questionnaire (PAQ-A and PAQ-C) were used to grade the average daily activities during the week prior to trauma. Statistical analysis was done by using the Chi-square test and p-value of <0.05 was considered to be statistically significant.
Results
Total 583 children were treated during the study period in the hospital including both Outpatient Department (OPD) and Emergency Department. About 433 children were excluded due to below age two years, refracture, chronic illness, and major congenital malformation. Among them only 150 patients met the criteria of present study. Out of 150 children, 69 (46%) were found obese and non-obese were 81 (54%). The distribution by gender was the same in obese group which had 26 (37.68%) female and 43 (62.32%) male, in non-obese group 34 (41.97%) female and 47 (58.03%) male. It was observed that both bones fracture of forearm in obese children was more at risk than non-obese children, p-value of <0.5 which was statistically significant.
Conclusion
Present study shows higher prevalence of forearm bone fracture in obese children than non-obese children. Obesity and other certain factors might have been significant risk factor for fracture required for operation. Both radius-ulna fracture in obese were found significant.
Body mass index, Children, Fracture, Obesity, Paediatric comprehensive classification of long bone fractures
Introduction
The World Health Organisation (WHO), in 1998 designated obesity as a global epidemic [1]. India is also facing the epidemic of obesity and its associated diseases, especially in children and adolescents [2]. Childhood obesity is associated with an increased mortality and morbidity characterised by coronary artery diseases, diabetes mellitus, hypertension and dyslipidemia [3]. The overt manifestation of bodyweight gain in children and adult has been regarded as a symbol of personal health and family wealth for much of human and urbanised, living standards continue to increase, obesity and weight gain have started to pose a rising threat to citizen’s health [4-7]. Compared to non-obese children, some studies have shown an increased risk of obese children having fracture [8-12], this risk is not only due to the behaviour of the child (play, fall, traffic accident etc.,), but is also due to the biomechanical properties of the bone and kinetics of the injury. The increased risk of fracture is associated with temporary bone weakness (relative osteopenia) during child development [13]. Both hormonal variations and the diet of children influence the accrual of bone and thereby, affect the biomechanical properties of bones [14]. It is uncertain in obese children if the increased risk is due to reduced accrual of bone or to severe kinetic injury [9]. Obesity was suggested to induce poor balance with some transient coordination disorder of development that could increase the risk of fracture [15]. There is growing evidence that children and adolescents of wealthy families are overweight relative to their counterparts in the past in current circumstances, possibly due to physical activities, sedentary lifestyle, altered eating habits and increased fat content of the diet [3,16].
CDC of the United States of America suggest that BMI is the most appropriate and easily available method to screen for childhood obesity. Age and gender cut-off for BMI are readily available. Obesity is increasing globally taking an epidemic significance with merely half a billion of world’s population now considered to be overweight and obese [17,18]. With this background, present study was conducted with an aim to study the prevalence of both bone fracture of forearm in obese and non-obese children between age group of 2-15 years.
Materials and Methods
A cross-sectional study was conducted in collaboration between Department of Paediatrics and Orthopaedics at Dr BC Roy Postgraduate Institute of Paediatric Science, Kolkata, West Bengal, India, from September 2017 to October 2018. After approval from the Institutional Ethics Committee (ethical clearance no.: BCH/ME/ PR:2352), the study was initiated. All the 583 children who were treated during the study period were included and 433 children were excluded due to below age of two years, refracture, chronic illness, and major congenital malformation. Total 150 patients were included in this study. The parents of all children, attending the institute who fulfilled the inclusion criteria were informed about this study. Written informed consent from the parents of all children was taken. History regarding name, age height, weight, any previous fracture, grade of activity level, type of fracture, kinetics of injury and treatment modalities were recorded.
Inclusion criteria: All children between 2-15 years of ages presenting to the emergencies for an Upper Extremity Long Bones Fracture (ULBF), attending the hospital OPD and those who are giving consent for participation in the present study were all included.
Exclusion criteria: Children having major congenital malformation and those who were suffering from any other chronic co-morbid conditions were excluded. Refractures cases were also excluded which are defined as fractures occurring within one year.
The anthropometric parameter was measured at the time of injury in the emergency department. Children having fractures were classified by using (Arbeitsgemeinschaft für Osteosynthesefragen) AO Paediatric Comprehensive Classification of long bone Fractures (PCCF) [Table/Fig-1] [19]. Calculation of BMI was done by the formula.
AO Paediatric Comprehensive Classification of long bone fractures (PCCF) [19].
| Bone | Segment | Morphology | Severity | Displacement for epiphysis |
|---|
| Humerus=1Radius=2rUlna=2u | Proximal/epiphysis or metaphysis=1E or 1M | 1 to 9 | 1 to 2 | Type 1 to 4 |
| Shaft/Diaphysis=2D |
| Distal/epiphysis or metaphysis=3E or 3M |
r: Radius; u: Ulna; E: Epiphysis; M: Metaphysis; D: Diaphysis
BMI=weight (kg)/{height(m)}2
Obese children were determined by the BMI percentile by plotting the BMI number on the appropriate CDC BMI-for-age growth chart [20]. Overweight and Obese children was determined by the BMI percentile by plotting the BMI number on the appropriate CDC BMI-for-age growth chart. Sex- and age-specific percentile cut points of a reference population (≤85th as normal, 85th-95th percentile for overweight and >95th percentile for obesity) [20]. Doubtful cases of obesity classification were confirmed by the paediatric surgeon. Injury mechanism was graded into three trauma kinetics (direct trauma, slow motion trauma and high motion trauma). The validated PAQ-A and PAQ-C were used to grade the average daily activities during the week prior to trauma [21].
Statistical Analysis
Using the Chi-square test, statistical analysis was conducted and the p-value of <0.05 was considered statistically significant. Statistical Package for the Social Sciences (SPSS) software with version 16 was used.
Results
Out of 150 children 69 (46%) with average age of 7.81 were found obese and non-obese were 81 (54%) with average age of 8.27 and p-value was 0.83 [Table/Fig-2]. The distribution by gender was the same in obese group which included 26 (37.68%) females and 43 (62.32%) males, in non-obese group 34 (41.97%) females and 47 (58.03%) males. We observed that both bones fracture of forearm in obese children was more at risk than non-obese children p-value was 0.014 which was statistically significant.
Distribution of age, Body Mass Index (BMI), Physical Activity Questionnaire (PAQ) grade, kinetics of injury, fracture location, treatment modalities and previous history of fracture are shown in table.
| Obese (n=69) | Non-obese (n=81) | p-value |
|---|
| Age mean±SD (2-15 years) | 7.81±2.3 | 8.27±2.1 | 0.83 |
| BMI mean±SD (range) | 22.7±3.6 (17 to 29.8) | 15.92±3.1 (13 to 21.2) | 0.001 |
| PAQ Grade mean±SD (range) | 2.86±1.12 (2.11 to 4) | 2.63±1.32(1.6 to 4.3) | 0.68 |
| Previous history of fracture (%) | 24 (34.78%) | 29 (35.80%) | 0.1 |
| Kinetics of Trauma |
| Direct (%) | 7 (10.14%) | 13 (16.05%) | 0.32 |
| Slow motion (%) | 33 (47.83%) | 29 (35.80%) | 0.63 |
| High motion (%) | 29 (42.03%) | 39 (48.15%) | 0.30 |
| Fractures |
| Radius (%) | 23 (33.33%) | 38 (46.91%) | 0.1 |
| Ulna (%) | 3 (4.35%) | 8 (9.87%) | 0.39 |
| Radius and ulna (%) | 33 (47.83%) | 18 (22.22%) | 0.01 |
| Humerus (%) | 6 (8.69%) | 15 (18.52%) | 0.53 |
| Humerus and radius (%) | 4 (5.80%) | 2 (2.47%) | 0.38 |
| Treatments |
| Immobilisation (%) | 51 (73.91%) | 62 (76.54%) | 0.1 |
| Manipulation under general anaesthesia (%) | 14 (20.29%) | 11 (13.58%) | 0.1 |
| Surgical pins (%) | 4 (5.80%) | 8 (9.87%) | 0.86 |
Chi-square test was used. Mean±Standard Deviation (SD)
Fracture of radius and ulna was seen in 33 children in obese patients and 18 children in non-obese patients respectively, which was statistically significant. Previous fracture history 24 (34.78%) and 29 (35.80%) were observed in obese and non-obese children respectively shown in [Table/Fig-2].
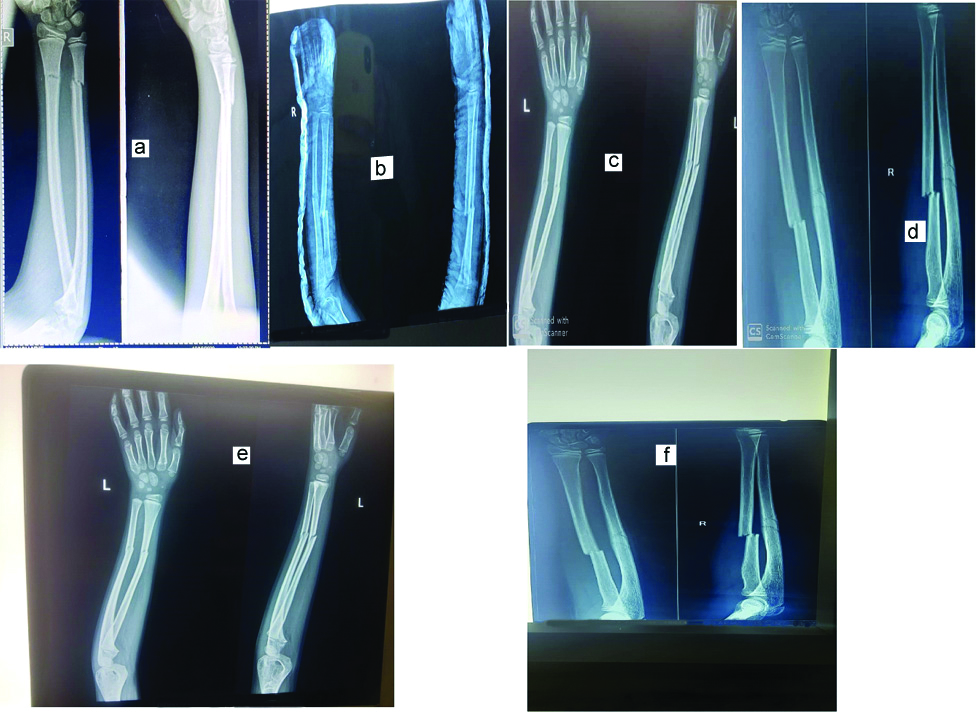
In obese patients humerus proximal and humerus diaphysis, humerus metaphysis distal fracture was seen in 2 (2.89%), 2 (2.89%), 6 (8.70%), respectively [Table/Fig-3]. But these were not statistically significant between the two groups [Table/Fig-3]. Images are demonstrated in [Table/Fig-4].
Different types of fracture in both groups analysed.
| Obese (n=69) | Non-obese (n=81) | p-value |
|---|
| Humerus and radius proximal | 2 (2.89%) | 5 (6.17%) | 0.27 |
| Humerus and radius diaphysis | 2 (2.89%) | 2 (2.47%) | 0.13 |
| Humerus metaphysis distal | 6 (8.70%) | 7 (8.64%) | 0.34 |
| Humerus epiphysis distal | - | 3 (3.70%) | 0.23 |
| Radius and ulna proximal | 4 (5.80%) | 7 (8.64%) | 0.39 |
| Radius and ulna diaphysis | 8 (11.60%) | 6 (7.41%) | 0.42 |
| Radius and ulna metaphysis distal | 37 (53.62%) | 42 (51.85%) | 0.34 |
| Radius and ulna epiphysis distal | 10 (14.50 %) | 9 (11.11%) | 0.19 |
Chi square test was used *In Humerus fracture, humerus and radius which were facture individually was also included; similarly in radius and ulna fracture, ulna fracture and radius fracture separately were also included
a) A 10-year-old obese child with distal 1/3rd radius and ulna fracture; b) Both radius and ulna fracture in eight-year-old male patient; c) Six-year-old patient with distal 1/3rd radius and ulna fracture; d)10-year-old obese child with mid shaft radius and ulna fracture; e) Anteroposterior (AP) and lateral view of nine-year-old child with distal 1/3rd radius and ulna fracture; f) AP lateral view of right radius and ulna mid shaft fracture in 11-year-old child.
Discussion
The gender distribution was the same with 26 (37.68%) females and 43 (62.32%) males in obese groups, 34 (41.97%) females and 47 (58.03%) males in non-obese groups. A similar observation has been observed by different researchers [22-24]. In this study, 46% of prevalence of fracture in obese group was observed. This was higher than studies done by Olds T et al., found 15.2% and Lasserre AM et al., reported 15% [25,26]. As reported in this study, the risk of fracture was greater in obese children, with similar findings reported in other research supporting this study [25,26]. Some research indicated that this increased risk may lead to poorer balance, impaired mobility and greater strength at low fall heights [9,27,28]. The presumption that there is a higher incidence of fracture in overweight/obese is derived from a non-obese/non-overweight retrospective analysis on health chart of children by Taylor ED et al., [27].
Higher incidence of limb fracture in obese paediatric patients (55%vs.40%) and high rate of surgical treatment was observed by Rana AR et al., [29]. No significant differences in the incidences of upper limb fracture were reported by Pomerantz WJ et al., [30]. About 157 distal radius fracture were reviewed and obese patients were highlighted because they were likely to require a second reduction (28%vs. 12%) observed by Auer R et al., [31]. The patients with diaphyseal forearm fracture of both radius and ulna were observed an incomplete reduction after cast treatment of conservative treatment reported by Okoroafor UC et al., and DeFrancesco C et al [32,33]. The similar finding was observed in this study. Goulding A et al., fracture tripled (O.R. 3.47% IC 1.69-7.09) in boys, who experienced forearm fractures, unlike this research findings from the high BMI [28]. While there was also an unexplained difference in present study results, Goulding’s severe complex fractures and a large number of chronic fracture patients involved analysed the male population as in the girl’s study. In children aged 9-16 years, a dose-dependent association was also recorded between TV, video and computer viewing and wrist/forearm fractures [34]. Inactivity can contribute to reduced postural balance and decreased muscle strength and coordination leading to an increased risk of falling. The most powerful surrogate for sedentary lifestyle, TV watching, has been consistently found to be correlated with childhood obesity [35]. In obese and non-obese there was no statistically significant difference in the history of previous fracture, which was in accordance to a recent cross-sectional Canadian study [36]. There is paucity of data on this topic and it is suggested that obesity is associated with various factors like nutrition, hereditary, hormonal, life style and environmental which could play as predisposing factors. Further studies on this and similar are needed to clarify the effect of unclear mechanism.
Limitation(s)
The cost of paediatric fracture management can be minimised without compromising protection. The optimum medical follow-up will also be injury prevention. In reality, they might have been misclassified, the accident might have been occurred when they were moving at very low speed. The information about the movement’s skills and physical fitness is important and it must be objectively assessed.
Conclusion(s)
Both radius-ulna fractures were found to be significant in obese patients. There is a lack of knowledge and more research is required to examine the relationship between obesity, bone growth and trauma. Child safety devices, regulation and system need further implication and revisited as the prevalence of child obesity increases.
r: Radius; u: Ulna; E: Epiphysis; M: Metaphysis; D: Diaphysis
Chi-square test was used. Mean±Standard Deviation (SD)
Chi square test was used *In Humerus fracture, humerus and radius which were facture individually was also included; similarly in radius and ulna fracture, ulna fracture and radius fracture separately were also included
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 22, 2020
Manual Googling: Oct 23, 2020
iThenticate Software: Oct 27, 2020 (21%)
[1]. Special issues in the management of obesity in childhood and adolescence. In World Health Organisation, ed. Obesity- Preventing and managing the global epidemic. Geneva: WHO, 1998; 231-47 [Google Scholar]
[2]. Fall CHD, Barker DJP, The foetal origins of coronary heart disease and non-insulin dependent diabetes in IndiaIndian Paediatric 1997 34(1):05-08. [Google Scholar]
[3]. Preventing childhood obesity is a current research focus: Initiatives corporation to show information and stem epidemicThe PAN Report: Physical Activity and Nutrition, USA International Life Science Institute 2000 2:P5 [Google Scholar]
[4]. Foster WR, Burton BT, Health implications of obesity: National Institutes of Health consequences conferenceAnn Intern Med 1985 103:977-1077.10.7326/0003-4819-103-1-1474003973 [Google Scholar] [CrossRef] [PubMed]
[5]. Van Itallie TB, Kral JG, The dilemma of morbid obesityJAMA 1981 246(9):999-1003.10.1001/jama.246.9.9997253188 [Google Scholar] [CrossRef] [PubMed]
[6]. Goulding A, Taylor RW, Jones IE, McAuley KA, Manning PJ, Williams SM, Overweight and obese children have low bone mass and area for their weightInt J Obes Relat Metab Disord 2000 24:627-32.10.1038/sj.ijo.080120710849586 [Google Scholar] [CrossRef] [PubMed]
[7]. Hubert HB, Feinleib M, McNamara PM, Castelli WP, Obesity as an independent risk factor for cardiovascular disease: A 26-year follow-up of participants in the Framingham Heart StudyCirculation 1983 67(5):968-77.10.1161/01.CIR.67.5.9686219830 [Google Scholar] [CrossRef] [PubMed]
[8]. McCarnen DA, Reusser ME, Body weight and blood pressure regulationAm J Clin Nutr 1996 63(3 suppl):423S-5S.10.1093/ajcn/63.3.4238615333 [Google Scholar] [CrossRef] [PubMed]
[9]. Davidson PL, Goulding A, Chalmers DJ, Biomechanical analysis of arm fracture in obese boysJ Paediatr Child Health 2003 39:657-64.10.1046/j.1440-1754.2003.00243.x14629495 [Google Scholar] [CrossRef] [PubMed]
[10]. Manias K, McCabe D, Bishop N, Fractures and recurrent fractures in children; varying effects of environmental factors as well as bone size and massBone 2006 39:652-57.10.1016/j.bone.2006.03.01816765659 [Google Scholar] [CrossRef] [PubMed]
[11]. Fornari ED, Suszter M, Roocroft J, Bastrom T, Edmonds EW, Childhood obesity as a risk factor for lateral condyle fractures over supracondylar humerus fracturesClinl Orthopaed Rel Res® 2013 471:1193-98.10.1007/s11999-012-2566-222965259 [Google Scholar] [CrossRef] [PubMed]
[12]. Seeley MA, Gagnier JJ, Srinivasan RC, Hensinger RN, VanderHave KL, Farley FA, Obesity and its effects on paediatric supracondylar humeral fracturesThe J Bone Joint Surg (American) 2014 96:e1810.2106/JBJS.L.0164324500590 [Google Scholar] [CrossRef] [PubMed]
[13]. Ferrari SL, Chevalley T, Bonjour JP, Rizzoli R, Childhood fractures are associated with decreased bone mass gain during puberty: An early marker of persistent bone fragility?J Bone Miner Res 2006 21:501-07.10.1359/jbmr.05121516598368 [Google Scholar] [CrossRef] [PubMed]
[14]. Dimitri P, Bishop N, Walsh JS, Eastell R, Obesity is a risk factor for fracture in children but is protective against fracture in adults: A paradoxBone 2012 50(2):457-66.10.1016/j.bone.2011.05.01121619952 [Google Scholar] [CrossRef] [PubMed]
[15]. Zhu YC, Wu SK, Cairney J, Obesity and motor coordination ability in Taiwanese children with and without developmental coordination disorderRes Dev Disabil 2011 32:801-17.10.1016/j.ridd.2010.10.02021109392 [Google Scholar] [CrossRef] [PubMed]
[16]. Gupta AK, Ahmad AJ, Childhood obesity and hypertensionIndian Paediatr 1990 27(4):333-37. [Google Scholar]
[17]. Yamagami T, Naruse M, Kagamimori S, Report of establishment and proceeding in Toyama study, Psychosomatic disturbance research “Research concerning prevention of chronic disease from childhood” March 1992 JapanMinistry of Health and Welfare [Google Scholar]
[18]. Braddon FE, Rodgers B, Wadsworth ME, Davies JM, Onset of obesity in a 36 year birth cohort studyBr Med J (Clin Res Ed) 1986 293(6542):299-303.10.1136/bmj.293.6542.2993089493 [Google Scholar] [CrossRef] [PubMed]
[19]. Slongo TF, Audigé L, Fracture and dislocation classification compendium for children: The AO paediatric comprehensive classification of long bone fractures (PCCF)J Orthop Trauma 2007 21(10 Suppl):S135-60.10.1097/00005131-200711101-0002018277238 [Google Scholar] [CrossRef] [PubMed]
[20]. Fleming-Dutra KE, Mao J, Leonard JC, Acute care costs in overweight children: A paediatric urban cohort studyChild Obes 2013 9:338-45.10.1089/chi.2012.013423767806 [Google Scholar] [CrossRef] [PubMed]
[21]. Kowalski KC, Crocker PRE, Faulkner RA, Validation of the physical activity questionnaire for older childrenPaediatric Exercise Science 1997 9:174-86.10.1123/pes.9.2.174 [Google Scholar] [CrossRef]
[22]. Haricharan RN, Griffin RL, Barnhart DC, Harmon CM, McGwin G, Injury patterns among obese children involved in motor vehicle collisionsJ Paediatr Surg 2009 44:1218-22.10.1016/j.jpedsurg.2009.02.02919524744 [Google Scholar] [CrossRef] [PubMed]
[23]. Zaveri PP, Morris DM, Freishtat RJ, Brown K, Overweight children: Are they at increased risk for severe injury in motor vehicle collisions?Accid Anal Prev 2009 41:959-62.10.1016/j.aap.2009.05.01119664432 [Google Scholar] [CrossRef] [PubMed]
[24]. Ryan LM, Teach SJ, Searcy K, Singer SA, Wood R, Wright JL, Epidemiology of paediatric forearm fractures in Washington, DCJ Trauma 2010 69(4 Suppl):S200-05.10.1097/TA.0b013e3181f1e83720938308 [Google Scholar] [CrossRef] [PubMed]
[25]. Olds T, Maher C, Zumin S, Péneau S, Lioret S, Castetbon K, Evidence that the prevalence of childhood overweight is plateauing: Data from nine countriesInt J Paediatr Obes 2011 6(5-6):342-60.10.3109/17477166.2011.60589521838570 [Google Scholar] [CrossRef] [PubMed]
[26]. Lasserre AM, Chiolero A, Cachat F, Paccaud F, Bovet P, Overweight in Swiss children and associations with children’s and parent’s characteristicsObesity (Silver Spring) 2007 15:2912-19.10.1038/oby.2007.34718198298 [Google Scholar] [CrossRef] [PubMed]
[27]. Taylor ED, Theim KR, Mirch MC, Ghorbani S, Tanofsky-Kraff M, Orthopedic complications of overweight in children and adolescentsPaediatrics 2006 117:2167-74.10.1542/peds.2005-183216740861 [Google Scholar] [CrossRef] [PubMed]
[28]. Goulding A, Jones IE, Taylor RW, Piggot JM, Taylor D, Dynamic and static tests of balance and postural sway in boys: Effects of previous wrist bone fractures and high adiposityGait Posture 2003 17:136-41.10.1016/S0966-6362(02)00161-3 [Google Scholar] [CrossRef]
[29]. Rana AR, Michalsky MP, Teich S, Groner JI, Caniano DA, Schuster DP, Childhood obesity: A risk factor for injuries observed at a level-1 trauma centerJ Paediatr Surg 2009 44:1601-05.10.1016/j.jpedsurg.2008.11.06019635312 [Google Scholar] [CrossRef] [PubMed]
[30]. Pomerantz WJ, Timm NL, Gittelman MA, Injury patterns in obese versus nonobese children presenting to a paediatric emergency departmentPaediatrics 2010 125:681-85.10.1542/peds.2009-236720194280 [Google Scholar] [CrossRef] [PubMed]
[31]. Auer R, Mazzone P, Robinson L, Nyland J, Chan G, Childhood obesity increases the risk of failure in the treatment of distal forearm fracturesJ Paediatr Orthop 2016 36:e86-88.10.1097/BPO.000000000000064926398434 [Google Scholar] [CrossRef] [PubMed]
[32]. Okoroafor UC, Cannada LK, McGinty JL, Obesity and failure of nonsurgical management of paediatric both-bone forearm fracturesJ Hand Surg 2017 42:711-16.10.1016/j.jhsa.2017.06.00628733098 [Google Scholar] [CrossRef] [PubMed]
[33]. DeFrancesco C, Rogers B, Shah A, Obesity increases risk of loss of reduction after casting for diaphyseal fractures of the radius and ulna in children: An observational cohort studyJ Orthop Trauma 2018 32:e46-51.10.1097/BOT.000000000000101028902088 [Google Scholar] [CrossRef] [PubMed]
[34]. Ma D, Jones G, Television, computer, and video viewing; physical activity; and upper limb fracture risk in children: A population-based case control studyJ Bone Miner Res 2003 18:1970-77.10.1359/jbmr.2003.18.11.197014606509 [Google Scholar] [CrossRef] [PubMed]
[35]. Fulton JE, Wang X, Yore MM, Carlson SA, Galuska DA, Caspersen CJ, Television viewing, computer use, and BMI among U.S. children and adolescentsJ Phys Act Health 2009 6:S28-35.10.1123/jpah.6.s1.s2819998847 [Google Scholar] [CrossRef] [PubMed]
[36]. Doan Q, Koehoorn M, Kissoon N, Body mass index and the risk of acute injury in adolescentsPaediatr Child Health 2010 15:351-56.10.1093/pch/15.6.35121731417 [Google Scholar] [CrossRef] [PubMed]