Unidentical Double Trouble- A Rare Case Report
Tanisha Singh1, Gramani Arumugam Vasugi2, Swaminathan Rajendiran3, Manickavasagam4, Shanmuganathan5
1 MBBS Student, Department of Pathology, SRIHER, Chennai, Tamil Nadu, India.
2 Assistant Professor, Department of Pathology, SRIHER, Chennai, Tamil Nadu, India.
3 Professor, Department of Pathology, SRIHER, Chennai, Tamil Nadu, India.
4 Professor, Department of Medical Oncology, SRIHER, Chennai, Tamil Nadu, India.
5 Professor, Department of Gastroenterology, SRIHER, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Gramani Arumugam Vasugi, Assistant Professor, Department of Pathology, SRIHER, Chennai, Tamil Nadu, India.
E-mail: arumugamvasugi@yahoo.com
Collision tumours are relatively rare entities and are thus, not well recognised. Collision tumour can be defined as two coexisting but histologically different malignancies involving the same organ or adjacent organ with an equivocal intermediate transitional zone between them. Collision tumours of the lung and oesophagus are very rare. Such cases are diagnosed by Computerised Tomogram (CT) Scan or Chest X-Ray for complaint of dysphagia. Definitive diagnosis is made by tissue biopsy. Here, a 66-year-old male is admitted for evaluation of an anterior mediastinal mass. Radiology revealed an anterior mediastinal mass extending in to the left hilar region and upper lobe of right lung anteriorly and in to the lower end of oesophagus posteriorly. Biopsy was performed. Microscopically, transbronchial biopsy revealed a cellular lesion, composed of round-to-oval cells with streaming nucleus, positive for Immunohistochemistry (IHC) markers, CD-56 and Synaptophysin pertaining to a diagnosis of small cell carcinoma. Biopsy of the oesophageal growth shows nest of dysplastic squamous epithelium which infiltrates into underlying muscularis propria showing features of a squamous cell carcinoma. Multiple fragments of squamous epithelium are also seen with necrotic tissue in vicinity and acute inflammatory exudate. Few cells show multinucleation, molding and margination of chromatin, showing the characteristic morphological features of Herpes oesophagitis. The patient was administered platinum-based Chemotherpy.
Collision tumour, Small cell carcinoma, Squamous cell carcinoma
Case Report
A 66-year-old male patient reported to the Outpatient Department with complaints of dysphagia, dry cough with wheezing and chest pain after oral intake of food, since one month. The patient also complained of persistent fever and loss of weight and appetite. Patient gave a history of chronic smoking for the past 15 years. Physical examination revealed that the patient was moderately malnourished and had facial puffiness. Respiratory system examination showed dilated veins in the chest and decreased vesicular breath sounds in both lungs. Based on the presenting symptoms and findings, a clinical diagnosis of lung malignancy was made. CT revealed an anterior mediastinal mass, casting irregular shadows in the mediastinum. Ill-defined soft tissue density mass was seen associated with the lesion having its epicenter in superior and anterior mediastinum and further extending into the left hilar region and the upper lobe of right lung anteriorly. The mass completely encloses both the bronchi. The mass infiltrates into the oesophageal wall posteriorly with narrowing of lumen which can be seen with the help of oral contrast [Table/Fig-1,2]. The provisional diagnosis, clinically and radiologically was made of a primary lung malignancy.
X-ray oral contrast showing narrowing of oesophageal lumina in the lower third of the oesophagus.

Computerised Tomogram (CT) showing hypoechoic mass lesion in the anterior mediastinum.

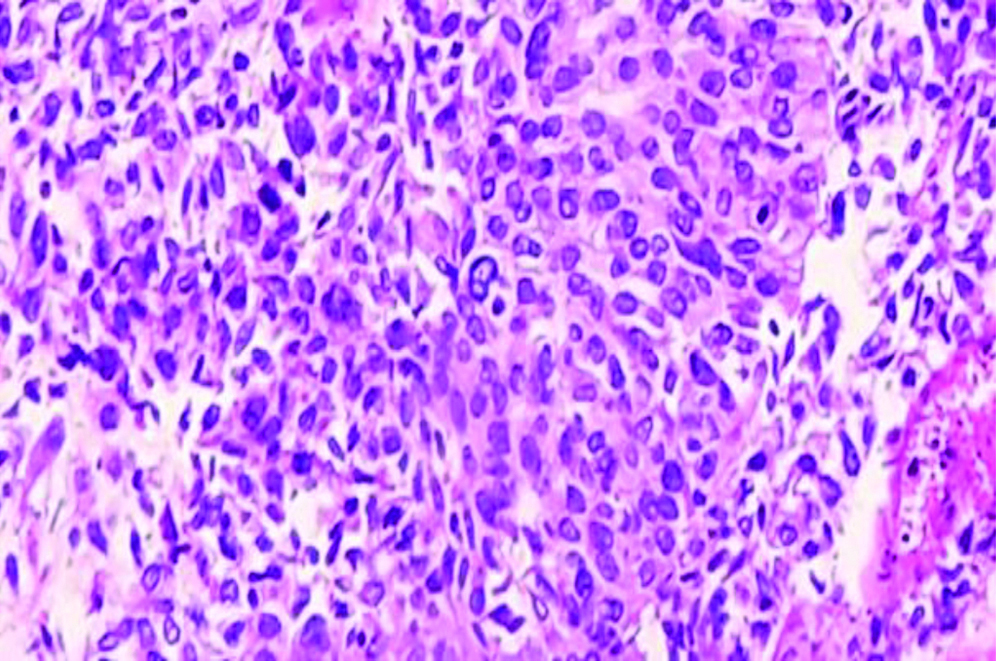
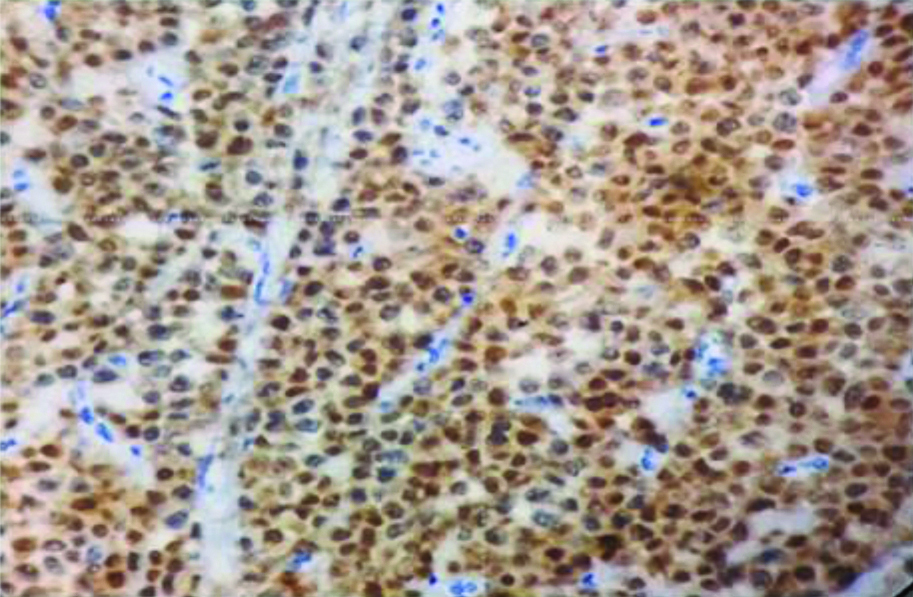
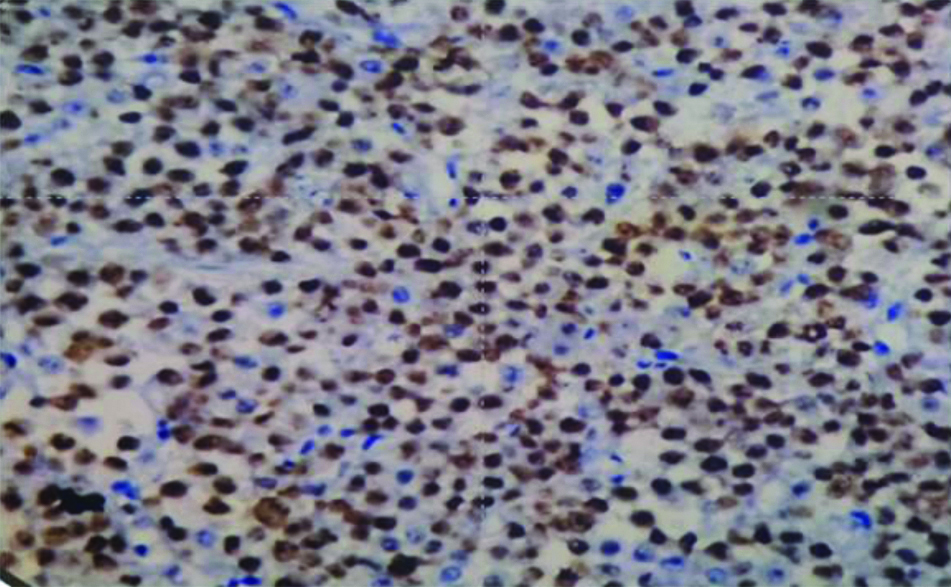
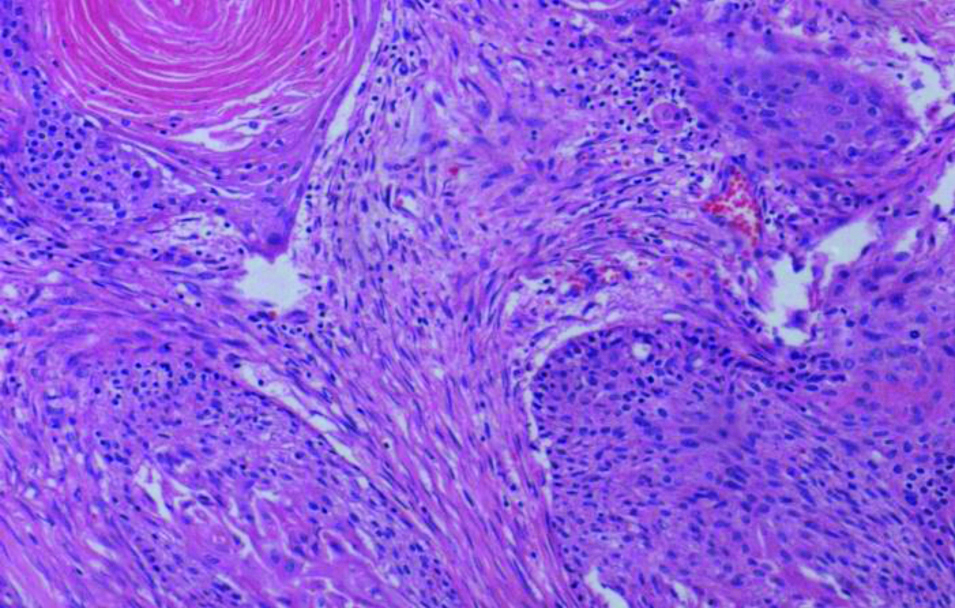
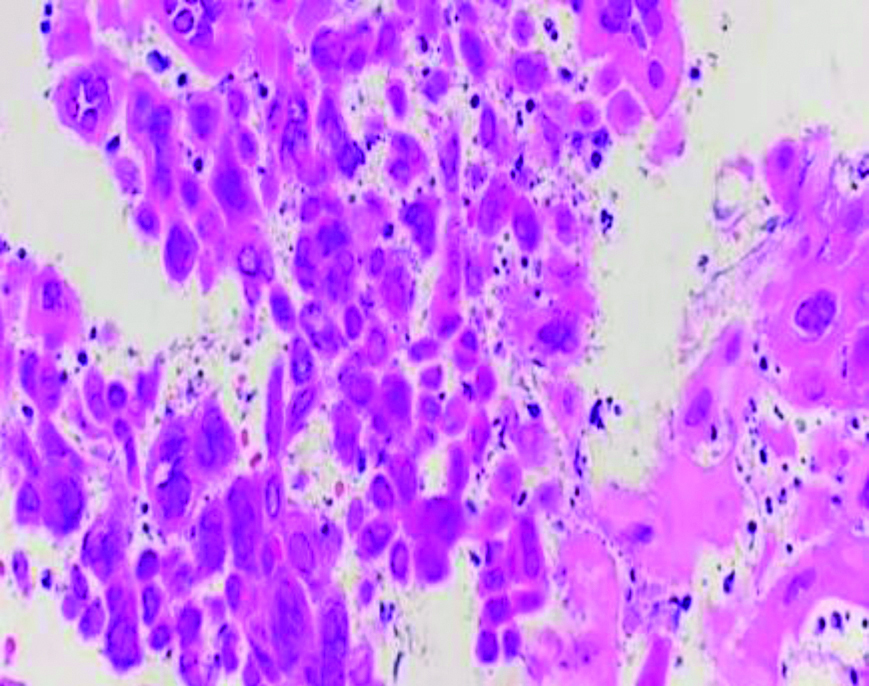
Biopsy was performed. The representative lesional bits from anterior portion were obtained by transbronchial approach and oesophageal portion was biopsied through upper gastrointestinal endoscopy. Grossly, there were multiple grey tan bits from the transbronchial biopsy aggregating to 0.5×0.5×0.3 cm. Microscopy showed three fragments, two of which revealed a cellular lesion composed of sheets of tumour cells with streaming effect in low power examination. On higher power examination, individual cells had scant cytoplasm and round to oval hyperchromatic nucleus. Adjacent fragment showed alveoli with fibrosis and necrosis amounting to 20% [Table/Fig-3]. With the above Hyalin and Eosin (H&E) features, a provisional diagnosis of small cell carcinoma was considered. Immunohistochemical staining was performed for confirmation of the provisional diagnosis. By IHC, the tumour cells stained positive for Synaptophysin [Table/Fig-4] and CD-56 [Table/Fig-5], which are the markers of neuroendocrine origin, rendering a diagnosis of small cell carcinoma. Also, lesion bits from upper GI endoscopic biopsy, of the mass infiltrating into the oesophagus showed nests of dysplastic squamous epithelium, infiltrating the underlying muscle and keratin pearl formation. Based on the classic H&E features, a diagnosis of moderately differentiated Squamous cell carcinoma was rendered [Table/Fig-6]. Adjacent areas of the oesophageal growth showed multiple fragments of squamous epithelium with necrotic tissue in vicinity and acute inflammatory exudate. Few cells showed multinucleation, molding and margination of chromatin in the nucleus. Morphologically, this was indicative of Herpes simplex associated oesophagitis [Table/Fig-7]. Thus, a final diagnosis of Collision Tumour composed of Squamous cell carcinoma and Small cell carcinoma with superadded Herpes oesophagitis was rendered.
Transbronchial biopsy showing tumour cells having hyperchromatic nucleus and features of Small cell carcinoma (H&E x 200x).
Immunohistochemical staining showing positivity for Synaptophysin (IHC x 100x).
Immunohistochemical staining showing positivity for CD-56 (IHC x 100x).
Upper gastrointestinal endoscopy biopsy from oesophagus showing features of squamous cell carcinoma (H&E x 200X).
Oesophageal biopsy showing cells with margination, molding and multinucleation resembling Herpes oesophagitis (H&E 400x).
Discussion
Collision tumours are relatively rare entities consisting of two histologically varied tumour cell populations developing in juxtaposition to one another with little or no transition zone [1]. They are thought to be the composed of two neighbouring independent neoplasms because a common carcinogenic stimulus evokes a neoplastic response in the cells of two adjacent, but different types of epithelium [2]. On the other hand, composite tumours are characterised by two divergent lineages originating in the same neoplastic clonal proliferation [3]. Most such tumours are reported in the gastroesophageal junction. Collision tumours with epicentre in the mediastinum involving lung and oesophagus are very rare. The two different histological components and their grading can be identified with the aid of immunohistochemical studies using neuroendocrine markers, epithelial markers and Ki-67 labelling index.
These tumours were reported in age group between 43 to 76 years, with an average age of 59 years. There was a male preponderance with a male to female ratio of 4:1 [4]. Most of these patients presented with dysphagia, which is the most common symptom of oesophageal cancer. Since these lesions grow exophytically inside the lumen of the oesophagus, the patient was 60-years-old male presenting with complaints of dysphagia. Collision tumour often occurs in the gastroesophageal junction, with most cases reported in the lower third of the oesophagus. The epicentre of the present case was seen in the anterior mediastinum extending in to left hilar region and upper lobe of right lung anteriorly and into the oesophagus posteriorly.
The diagnosis criteria of collision tumour as proposed by Spagnolo DV and Heenan PJ is that, there should be two topographically separate sites of origin for the different components present in the tumour [5]. In the present case, the small cell component was present in the lung and squamous component was present in the oesophagus. They have also mentioned that there must be some separation of the two components so that, the dual origin can be recognised despite intimate mixing at points of juxtaposition. There may be some transition patterns in the areas of collision, in addition to intimate mixing of the two components. Brahmania M et al., have provided the three possible mechanisms for the development of collision tumours [6]. Accordingly, the rare possibility that two primary tumours develop adjacent to each other at the same time or one tumour develops and changes local microenvironment to promote the development of the second tumour; and the third possibility is that the two types of tumours share a common origin of pluripotent precursor stem cells that differentiate into the different histological components of tumour cell types.
Genetic alterations associated with Squamous cell carcinoma include mutations or amplification of p53, p16INK4a, cyclin D1, cyclin E, c-MYC and EGFR. Common cytogenetics associated with Small cell carcinoma are p53 mutations due to deletion at 17p and RB1 loss of function at 13q14 and both histological subtype are known to be associated with tobacco use and smoking. Histopathological and immunohistochemical analysis play a major role in confirming these rare collision tumour types. Histologically, Squamous cell carcinomas show an infiltrative growth pattern of tumour cells with varying degrees of nuclearatypia. Small cell carcinomas are considered to be poorly differentiated endocrine tumours and are described to be indistinguishable from its counterpart in the lung in terms of histological, immunohistochemical and clinical features [7]. The biological behaviour and prognostication of these tumours are not well-established because of the rarity of these combined tumours. Tadashi T et al., described that collision tumours with Small cell carcinoma component can be treated as per primary Small cell carcinoma protocol because of its aggressive tumour biology compared to the other component [8]. The prognosis appears to depend on the stage of the tumour at the time of initial diagnosis and the degree of differentiation, since the poorest differentiated component will determine the prognosis. The National Comprehensive Cancer Network (NCCN) guidelines recommend cisplatin or carboplatin and etoposideprotocols for Small cell lung carcinoma [9]. The patient has completed concurrent radiotherapy and platinum-based chemotherapy and currently on follow-up for a period of 8 months. A thorough literature search suggested that only few cases has been documented in literature till date [Table/Fig-8].
Literature search of similar case reports [6,10-13].
| Auhtor name and Reference | Patient details | Location | Components in collision tumour |
|---|
| Peng L and Schwarz RE [10] | 52/M | Duodenum | Adenocarcinoma+Neuroendocrine carcinoma |
| Brahmania M et al., [6] | 64/F | Colon | Granulosa cell tumour +Adenocarcinoma |
| Marco F et al., [11] | 64/M | Duodenum | Carcinoid+ Adenocarcinoma |
| Varikatt W et al., [12] | 37/F | Ampulla of vater | Somatostatinoma+Neurofibroma |
| Hirono S et al., [13] | 75/M | Ampulla of vater+common bile duct | Adenocarcinoma+Cholangiocarcinoma |
| Present case | 66/M | Anterior mediastinum | Small cell carcinoma+Squamous cell carcinoma |
M: Male; F: Female
Conclusion(s)
Collision tumours are relatively rare, their clinical and biological behaviour including tumourigenesis and differentiation remain unclear. However, diagnosing this entity is significant therapeutically, since the individual tumour histological types may require different treatments protocols.
M: Male; F: Female
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 26, 2020
Manual Googling: Sep 18, 2020
iThenticate Software: Nov 20, 2020 (8%)
[1]. Majmudar B, Dillard R, Susann PW, Collision carcinoma of the gastric cardiaHum Pathol 1978 9:471-73.10.1016/S0046-8177(78)80032-X [Google Scholar] [CrossRef]
[2]. Terada T, Maruo H, Esophageal combined carcinomas: Immunohistochemical and molecular genetic studiesWorld J Gastroenterol 2012 18(13):1545-51.10.3748/wjg.v18.i13.154522509088 [Google Scholar] [CrossRef] [PubMed]
[3]. Nakata S, Nagata Y, Sugaya M, Yasuda M, Yamashita T, Takenoyama M, Primary pulmonary collision cancer consisting of large cell carcinoma and adenocarcinomaAnn Thorac Surg 2005 80(1):340-42.10.1016/j.athoracsur.2003.12.05315975404 [Google Scholar] [CrossRef] [PubMed]
[4]. Wang L, Ma L, Zahn C, Shi Y, Collision tumour of esophagus: Report of three casesThe Annals of Thoracic Surgery 2014 97(3):1075-77.10.1016/j.athoracsur.2013.06.09024580931 [Google Scholar] [CrossRef] [PubMed]
[5]. Spagnolo DV, Heenan PJ, Collision carcinoma at the esophagogastric junction: Report of two casesCancer 1980 46(12):2702-08.10.1002/1097-0142(19801215)46:12<2702::AID-CNCR2820461228>3.0.CO;2-M [Google Scholar] [CrossRef]
[6]. Brahmania M, Kanthan C, Kanthan R, Collision tumour of the colon-colonic adenocarcinoma and ovarian granulosa cell tumourWorld J SurgOncol 2007 5:11810.1186/1477-7819-5-11817949502 [Google Scholar] [CrossRef] [PubMed]
[7]. Tennvall J, Johansson L, Albertsson M, Small cell carcinoma of the oesophagus: A clinical and immunohistopathological reviewEur J SurgOncol 1990 16(2):109-15. [Google Scholar]
[8]. Tadashi T, Nishimaki T, Kanda T, Nakagawa S, Ohashi M, Hatakeyama K, Esophageal composite carcinoma with tripartite differentiation: Clinicopathological analysis of three casesEsophagus 2005 2(2):91-96.10.1007/s10388-005-0039-3 [Google Scholar] [CrossRef]
[9]. Neuroendocrine Tumours, NCCN Clinical Practice Guidelines in OncologyNCCN Guidelines 2015 [Google Scholar]
[10]. Peng L, Schwarz RE, Collision tumour in form of primary adenocarcinoma and neuroendocrine carcinoma of the duodenumRare Tumours 2012 4(2):e2010.4081/rt.2012.e2022826777 [Google Scholar] [CrossRef] [PubMed]
[11]. Ferrando Marco J, Pallas Regueira A, Moro Valdezate D, FernándezMartínez C, Tumour de colisiónperiampular [Collision tumour of the ampulla of Vater: Carcinoid and adenocarcinoma]Rev EspEnferm Dig 2007 99(4):235-38.10.4321/S1130-0108200700040001017590108 [Google Scholar] [CrossRef] [PubMed]
[12]. Varikatt W, Yong JL, Killingsworth MC, Somatostatinoma: Collision with neurofibroma and ultrastructural featuresHistolHistopathol 2006 21(11):1171-80. [Google Scholar]
[13]. Hirono S, Tani M, Terasawa H, Kawai M, Ina S, Uchiyama K, A collision tumour composed of cancers of the bile duct and ampulla of Vater-immunohistochemical analysis of a rare entity of double cancerHepatogastroenterology 2008 55(84):861-64. [Google Scholar]