An Interesting Case of Rhino-Orbito Cerebral Mucormycosis: A Case Report
R Minnu Lekshmi1, Stephen Sudhakar2, S Rajasekharan3
1 Postgraduate Resident, Department of Ophthalmology, Chettinad Hospital and Research Institute, Kelambakkam, Tamil Nadu, India.
2 Professor and Head, Department of Ophthalmology, Chettinad Hospital and Research Institute, Kelambakkam, Tamil Nadu, India.
3 Professor and Head, Department of Otolaryngology, Chettinad Hospital and Research Institute, Kelambakkam, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Stephen Sudhakar, Professor and Head, Department of Ophthalmology, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
E-mail: dr.stephen@chettinadhealthcity.com
Fungal infections are the most challenging problems in an immunocompromised individuals. Mucormycosis is a life-threatening fungal infection with rapid progression and high mortality in immunocompromised individuals. A case of 58-year-old female, with uncontrolled diabetes is presented here with five days history of headache, fever, and acute-onset drooping of the eyelid. The initial vision was normal which dropped to no Perception of Light (PL) in the following days, with ophthalmoplegia and dilated non-reactive pupil in the right eye. Fundus and Intra-ocular Pressure (IOP) were normal on presentation. Magnetic Resonance Imaging (MRI) and Magnetic Resonance Venography (MRV) brain showed subtle ethmoidal cysts. Computerised Tomography-Paranasal Sinuses (CT-PNS) showed mild ethmoidal thickening and cyst. Diagnostic Nasal Endoscopy (DNE) showed unhealthy mucosa with no lesion suggesting eschar. A provisional diagnosis of orbital mucormycosis was made. The patient was started on antibiotics and Intravenous (IV) amphotericin B but she went on to further neurological complications. Despite treatment, she developed necrotising eschars in eyelid for which debridement was done. Further, exenteration was advised and patient developed septicaemia, however he died. The culture from debrided tissue showed growth of mucor. The objective of presenting this particular case is to emphasise the importance of considering mucormycosis as diagnosis despite subtle radiological and endoscopic findings in symptomatic immunocompromised patients. Early diagnosis and aggressive management improve and give better chances for survival.
Amphotericin, Ethmoid sinus, Immunosuppression, Uncontrolled diabetes
Case Report
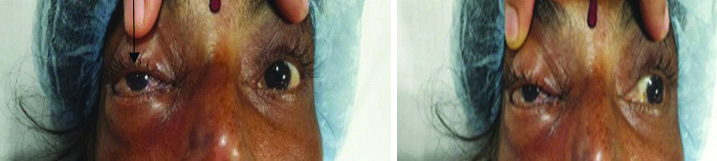
A 58-year-old female presented with complaints of severe headache in the temporal area, redness of eye and drooping of the eyelid of one-day duration in the right eye, fever for five days duration. She was a known case of Diabetes Mellitus (DM) on irregular treatment for past five years. On presentation, she was febrile, conscious and oriented, emaciated with stable vitals. On ocular examination, the right eye showed complete ptosis, with total ophthalmoplegia [Table/Fig-1], absent corneal sensation with mid-dilated and non-reactive pupil. IOP was within a normal range, vision was 6/18 with no improvement with the pinhole in the right eye. The left eye was within normal limits. Colour vision was normal in both eyes. Fundus examination was normal on the day of presentation in both eyes.
Patient on levoversion showing ophthalmoplegia in the right eye. Proptosis of right eye and chemosis evident.
The patient was admitted with a preliminary diagnosis of multiple cranial nerve palsy (3rd, 4th, 5th, and 6th nerve complete palsy) involving pupil, superior orbital fissure syndrome and orbital cellulitis suspecting fungal aetiology.
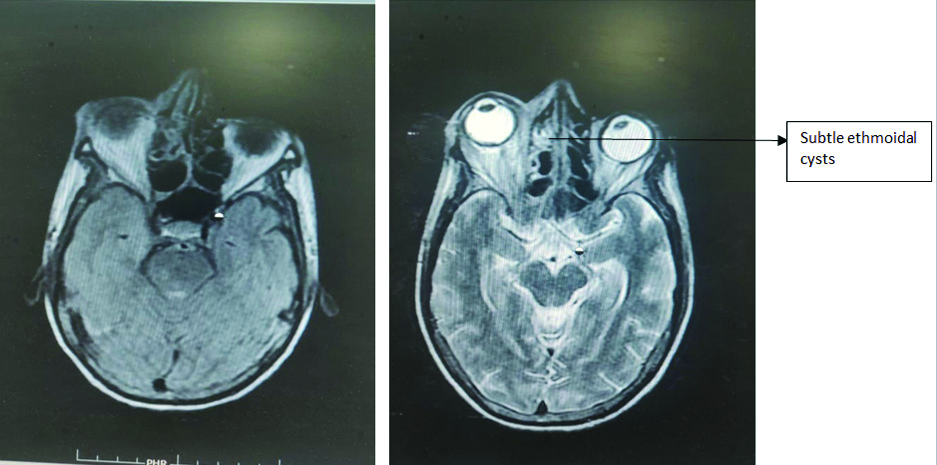
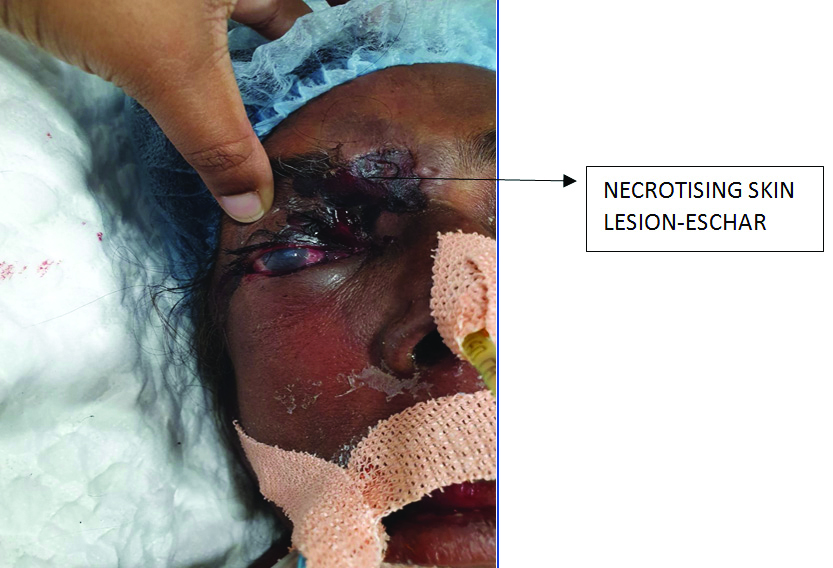
Following the day of admission, patient’s headache worsened, MRI and MRV brain [Table/Fig-2] showed subtle ethmoidal cysts which were confirmed with CT-PNS. DNE was done which showed unhealthy mucosa with no lesion suggesting eschar. Vision on the second day of admission was observed to have deteriorated to hand movements IOP was raised to 34 in the right eye. Blood sugar values were observed to be in 400 mg/dL with urine report showing ketone bodies. The patient was shifted to Intensive Care Unit (ICU) and was started with IV antibiotics and IV liposomal amphotericin B slow infusion and insulin injections in view of controlling blood sugar with strict monitoring of vitals, despite being started with antifungal and antibiotics patient was seen to be worsening and she went on to cavernous sinus thrombosis and middle cerebral artery occlusion leading to stroke. On fundus examination, vessel were attenuated cattle tracking with retinal oedema suggesting retinal artery occlusion. She was started on heparin for the same. On the third day, the patient started developing dark colour eschars [Table/Fig-3], for which wound debridement was done and tissue was sent for culture. Observing the fast extension of the lesion and worsening of the general condition despite the aggressive treatment, the patient was advised excentration. Following day, the patient developed septicaemia and went into cardiac arrest. Posthumously, culture reports came showing vigorous growth of fungi suggesting mucormycosis.
Magnetic Resonance Imaging (MRI) images showed subtle ethmoidal cysts.
Eschar formation on the skin over eyelid on 4th day.
1. Proptosis of right eye and chemosis
Discussion
Mucormycosis is an opportunistic, aggressive fatal fungal infection, in immunocompromised patients. This infection begins from the sinonasal mucosa on inhaling fungal spores; the aggressive and rapid progression leads to orbital and brain involvement. Recently, a reported change in epidemiology of mucormycosis, with rise in incidence in Asian Continent has been observed [1]. The most common predisposing factor is DM (60-80%) in poor control, any immunocompromised individual may be infected in this case discussed above the patient was uncontrolled diabetes with really high blood sugar values [2,3]. She was reluctant to follow insulin orders from medical practitioners hence, presented with uncontrolled diabetes with urine report suggesting diabetic ketoacidosis. According to many studies observed, diabetes remains the most common cause of fungal infections like mucormycosis with a very high mortality rate in view of the immunecompromised state. Mortality is due to complications associated with fungal infections [2,3].
Studies in previous years show presentations of cases with mucormycosis infection depend on the site of presentation. Rhino-Orbital mucormycosis being the most common type, it Is seen that most common clinical presentations of rhino-orbital mucormycosis in different study groups were periorbital oedema, pain, proptosis, ophthalmoplegia and decreased vision. In the above discussed, patient had a similar presentation [4].
Mucormycosis diagnosis is mainly relied on the MRI findings. CT-PNS reports and culture reports as add to the radiological reports. CT-PNS shows sinus opacification with a rim of soft tissue thickness along with the paranasal sinuses complete sinus opacification, gas-fluid levels and obliteration of nasopharyngeal tissue planes can also occur. In the above discussed case, the MRI report showed subtle ethmoidal cysts. CT-PNS with mild ethmoidal thickness and cyst. The MRI reports were inconclusive, and the culture reports were obtained only later, nasal endoscopy showed subtle colour changes compared to the normal side. So, the patient was started on antifungal drugs considering the immunocompromised state and the clinical findings.
Mucormycosis in later stages presents with complication as cavernous sinus thrombosis, and eschar formation [5]. Mbarek C in his study, reported a case of extensive hemifacial cutaneous necrosis and nasal endoscopy revealed black necrotic lesions [6,7]. In present case, the patient on the third day went on to cavernous sinus thrombosis and stroke and later started developing eschar on day four.
Amphotericin B is considered as the gold standard in the medical management of mucormycosis. Aggressive debridement is the surgical management of choice. Rhinocerebral cases require exenteration [8]. However, amphotericin B being nephrotoxic, therefore, blood levels should be monitored carefully [9]. The patient was also planned to start on posaconazole but could not be arranged due to unavailability [10,11].
The patient was treated clinically with systemic antifungal agents (amphotericin B), intravenous antibiotics with heparinization and with debridement of necrotic areas. The patient was worsening for which exenteration was advised. But bystanders were not willing. Because of uncontrolled diabetes, the patient developed septicaemia and went into cardiac arrest.
Conclusion(s)
Total ophthalmoplegia with evolving proptosis and fever in an immunocompromised person should be diagnosed early as a possible case of rhino orbital mucormycosis even when there is only subtle radiological and nasal endoscopic evidence. Apart from medical management, early debridement and possible exenteration of orbit could prevent the Central Nervous System spread in this rapidly progressing and fatal infection.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 01, 2020
Manual Googling: Aug 03, 2020
iThenticate Software: Nov 18, 2020 (4%)
[1]. (PDF) Global Epidemiology of Mucormycosis [Internet]. Research Gate. [cited 2020 Aug 27]. Available from: https://www.researchgate.net/publication/331946787_Global_Epidemiology_of_Mucormycosis [Google Scholar]
[2]. Karadeniz Uğurlu Ş, Selim S, Kopar A, Songu M, Rhino-orbital Mucormycosis: Clinical findings and treatment outcomes of four casesTurk J Ophthalmol 2015 45(4):169-74.10.4274/tjo.8247427800226 [Google Scholar] [CrossRef] [PubMed]
[3]. Yohai RA, Bullock JD, Aziz AA, Markert RJ, Survival factors in rhino-orbital-cerebral mucormycosisSurv Ophthalmol 1994 39(1):03-22.10.1016/S0039-6257(05)80041-4 [Google Scholar] [CrossRef]
[4]. Ferry AP, Abedi S, Diagnosis and management of rhino-orbitocerebralmucormycosis (phycomycosis). A report of 16 personally observed casesOphthalmology 1983 90(9):1096-104.10.1016/S0161-6420(83)80052-9 [Google Scholar] [CrossRef]
[5]. Dimaka K, Mallis A, Naxakis SS, Marangos M, Papadas TA, Stathas T, Chronic rhinocerebralmucormycosis: A rare case report and review of the literatureMycoses 2014 57(11):699-702.10.1111/myc.1221925039925 [Google Scholar] [CrossRef] [PubMed]
[6]. Mbarek C, Zribi S, Khamassi K, Hariga I, Ouni H, Ben Amor M, Rhinocerebralmucormycosis: Five cases and a literature reviewB-ENT 2011 7(3):189-93. [Google Scholar]
[7]. Rhinocerebralmucormycosis | Radiology Reference Article | Radiopaedia.org [Internet]. [cited 2020 Aug 27]. Available from: https://radiopaedia.org/articles/rhinocerebral-mucormycosis [Google Scholar]
[8]. Weerakkody Y, Rhinocerebralmucormycosis | Radiology Reference Article | Radiopaedia.org [Internet]Radiopaedia[cited 2020 Aug 27]. Available from: https://radiopaedia.org/articles/rhinocerebral-mucormycosis [Google Scholar]
[9]. Lipid formulations of amphotericin B as first-line treatment of zygomycosis- Clinical Microbiology and Infection [Internet]. [cited 2020 Aug 27]. Available from: https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(14)60736-9/fulltext [Google Scholar]
[10]. Dayal D, A multimodal approach is necessary to manage mucormycosis in patients with diabetesJ Clin Diagn Res 2016 10(9):SL0110.7860/JCDR/2016/21349.847727790541 [Google Scholar] [CrossRef] [PubMed]
[11]. Mohammadi R, Nazeri M, Sayedayn SMA, Ehteram H, A successful treatment of rhinocerebralmucormycosis due to Rhizopus oryzaeJ Res Med Sci Off J Isfahan Univ Med Sci 2014 19(1):72-74. [Google Scholar]