Ergonomics (from Greek word ‘ergo’ means work; ‘nomos’ means natural law) is the science of interaction between human and their working environment. Basic ergonomics had existed since the creation of primitive tools by early men to make his task easier. Even Hippocrates had given a description of surgeon’s posture and arrangement of his tools during the procedure [1].
Murrel coined the term ‘Ergonomics’ during the Second World War, which formed the basis for the studies of human interaction with machines and environment [2]. Then, it started expanding to other fields to improve performance and to ensure safety and wellbeing of the individual. The international ergonomic association defines “Ergonomics is the scientific discipline concerned with the understanding of interaction among human and other elements of a system and the profession that applies theory principles, data and methods to design in order to optimise human wellbeing and overall system performance [3]. The application of ergonomic strategies requires the study of body mechanics, nature of the work and environmental factors.
Many authors have described the ergonomic aspects in relation to Critical Care Units [4], Endoscopy [5], Laparoscopy [6] and Ultrasonography [7]. The use of US in regional anaesthesia has significantly increased in last few years. Advantages of Ultrasound-Guided Regional Anaesthesia (UGRA) are the ability to identify the anatomical structures in real time, which allows precise administration of local anaesthetic around the nerves [8]. Compared with peripheral nerve stimulation, UGRA procedures are fast, quick in onset and provide longer duration of action, low failure rate, with low-risk of vascular puncture and local anaesthetic toxicity [9]. The growing use of UGRA has created the need to consider ergonomic aspects relevant to regional anaesthetic procedures also. Since most of the procedures are being done in the environment that is not designed for these procedures, optimal positioning of ultrasound machine is not always possible. This may be because of limited workspace, patient positioning and equipment size. Working in these ergonomically-challenged spaces may aggravate pre-existing back or neck pain. Sites [10] found that turning the trunk and turning the head ≥45° is a source of error among novice operator when performing UGRA procedures and is often associated with fatigue and poor performance. Even though the benefits of ergonomic aspects are being recognised, it is not included in most of the academic training programs.
TAP block is a commonly performed procedure as a component of multimodal analgesia for various lower abdominal surgeries like caesarean section [11], appendicectomy [12] and inguinal herniorrhaphy [13]. This study was designed to analyse the ergonomic considerations of USG TAP block for inguinal hernia repair between experienced and novice anaesthesiologists. The main focus is on the dynamic interaction between the anaethesiologist-patient, and environmental factors, based on ergonomic principles [14,15] during the performance of the block.
Materials and Methods
After approval of Ethical Committee (IHEC/0292/2017) and getting written informed consent from both the participating anaesthesiologists and patients, a prospective observational study on ergonomic consideration was conducted for six months from April, 2018 including all the TAP block procedures after inguinal hernia repair, which fulfilled the criteria.
Twenty one male patients of age 18-60 years with American Society of Anaestheiologists (ASA) grade I-II posted for inguinal hernia repair under spinal anaesthesia were included in the study. Exclusion criteria were: patient refusal, BM1 >30 kg/m2 and bilateral hernia. Among the 21 anaesthesiologists, 10 had performed more than 20 TAP block procedures (Experienced/E) and 11 had performed at least 5 TAP block procedures (Novice/N). Recruitment was dependent on both patient’s and anaesthesiologist’s consents and availability of a dedicated single investigator who was responsible for real time data collection.
All the procedures were done under spinal anaesthesia with standard sterile protocol. On the completion of surgical procedure, USG TAP block was performed in Operating Room (OR) or Recovery Room (RR) under standard sterile protocol. Heart rate, oxygen saturation, noninvasive blood pressure, electrocardiograph were monitored during the procedure. Height of the operator before and during the procedure was measured using the measuring scale. Height of the OR table and cot in RR was measured at its centre, in neutral position. Adjustment of table and chair done by the operator before the procedure was recorded. Height of the ultrasound machine was measured from the centre of the screen to the bottom of the machine. Ratio of height of the operator during the procedure and height of ultrasound machine was calculated [16]. Positioning of neck, back and shoulder during the procedure were recorded. Location of performance of block was noted. Position of the ultrasound machine in relation to operator was noted. Position of assistant and trolley in relation to operator was also recorded.
After the identification of iliac crest and sub-costal margin, the linear probe of frequency (6-14 MHz) of sonosite SII was placed in mid axillary line on a transverse plane. After visualisation of abdominal layers, 22G 50 mm insulated nerve block needle was inserted 1 cm medial to the probe and was advanced using in plane technique. Nature of available assistance was similar in all procedures. The observation period started from positioning of patient to the end of injection of 20 mL of 0.25% bupivacaine in the fascial plane. Data were collected by direct observations and photographs taken during the procedure [17] and using goniometer [18].
Statistical Analysis
Statistical analysis was performed using statistical package for social sciences version 16.0. Numerical data were presented as mean (Standard deviation) and between groups, differences were compared using independent sample student t-test. For categorical variables Fisher’s-exact test was used. P<0.05 was considered statistically significant.
Results
Among the 21 anaesthesiologists, 19 were right-handed and two were left-handed, [Table/Fig-1]. All the procedures were successful. Among 21 patients, 14 patients had surgery on right side and seven had surgery on the left side. While during a procedure, a novice couldn’t reach the target plane accurately, experienced operator intervened and repeated the procedure, which was included in experienced data.
| Parameters | Experienced (E) | Novice (N) |
|---|
| Experience of operators | > TAP block 20 procedures | At least 5 TAP block procedures |
| Male/Female | 8/2 | 6/5 |
| Handedness (Right/Left) | 10/0 | 9/2 |
Operator Factors
Height of experienced operators during the procedure was 148±5.01 cm whereas the height of novice was 153±8.78 cm which was not statistically significant. The mean difference of height of experienced operator was 12.7±5.9 cm and novice was 6.8±6.3 cm. The difference was statistically significant p=0.041 (p<0.05). Height of OR table or cot on RR on which patients were lying supine during procedure was 72.7±3.09 cm for experienced and 72.45±2.62 cm for novice which was not statistically significant [Table/Fig-2].
| Parameters (cm) | Experienced | Novice | p-value |
|---|
| Height of operator | 161.3±3.4 | 159.8±5.8 | 0.49 |
| Height of the operator during procedure | 148.0±5.04 | 153.0±8.78 | 0.13 |
| Mean difference of Height | 12.7±5.9 | 6.8±6.3 | 0.041 |
| Ratio of the height of operators during procedure to the height of Ultrasound machine | 1.13±0.03 | 1.17±0.06 | 0.126 |
| Height of the table | 72.7±3.09 | 72.45±2.62 | 0.846 |
Values are expressed as mean±SD Standard Deviation; t-Test p<0.05 significant
A 7E and 2N performed the procedure in sitting position and others in standing position which was statistically significant (p=0.03). A 7E and 2N checked and adjusted the position of table before performing the procedure which was statistically significant (p=0.03). A 2E and 8N flexed their back; 7E kept their neck flexed less than 20° and 9N kept their neck flexed more than 20°, the different was statistically significant (p=0.001) [Table/Fig-3]. All the operators kept the probe in non-dominant hand and needle in dominant hand.
Comparison of operator factors.
| Parameters | Experienced | Novice | Fisher’s-Exact test p-value |
|---|
| Position |
| Sitting | 7 | 2 | 0.030 |
| Standing | 3 | 9 |
| Adjustment of table |
| Done | 7 | 2 | 0.030 |
| Not done | 3 | 9 |
| Thoracolumbar position |
| Flexion | 2 | 8 | 0.030 |
| Neutral | 8 | 3 |
| Position of neck |
| Flexion <20° | 7 | 0 | 0.001 |
| >20° | 0 | 9 |
| Extension <15° | 3 | 0 | 0.100 |
| >15° | 0 | 2 |
| Rotation <45° | 0 | 5 | 1.00 |
| >45° | 0 | 1 |
| Position of shoulder |
| Tilt | 3 | 7 | |
| Neutral | 7 | 4 | 0.198 |
p<0.05 significant
Environmental Factors
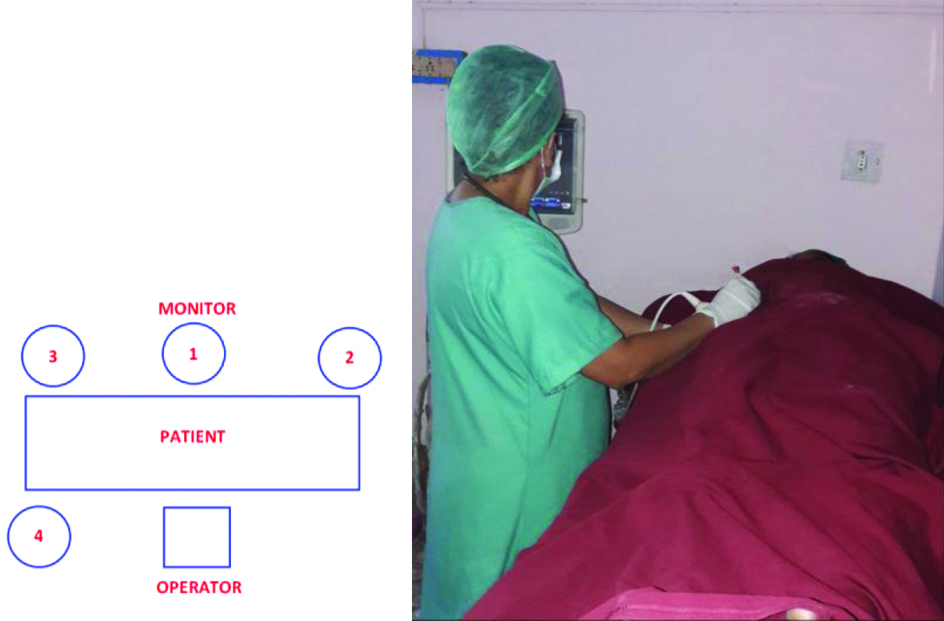
A 10E and 5N kept ultrasound monitor in front in line. A 3N kept ultrasound monitor in front towards right side and 2N kept in front towards left side. A 1N kept monitor in same side to his left. The difference was statistically significant (p=0.0124) as shown in [Table/Fig-4a,b].
(a) Schematic representation of USG monitor position in relation to operator. 1. Monitor front in line; 2. Front towards right; 3. Front towards left; 4. Same side towards left; (b) Same side positioning of Ultrasound Monitor.
There was no significant difference found between experienced and novice in terms of side of the block performed, location of the procedure, position of assistants and trolleys in relation to operator during the procedure as shown in [Table/Fig-5]. Compact kit was not available for four of the procedures. A total of 17 procedures were assisted by anaesthesiologists and four were assisted by nursing staff. US screen was obstructed by the assistants, when two procedures when done by novice.
Comparison of environmental factors.
| Parameters | Experienced | Novice | Fisher’s-Exact test p-value |
|---|
| Location of block |
| Operating room | 8 | 8 | 1.00 |
| Recovery room | 2 | 3 |
| Side of the block |
| Right | 7 | 7 | 1.00 |
| Left | 3 | 4 |
| Position of assistants |
| Same side | 10 | 9 | 0.476 |
| Front | 0 | 2 |
| Position of trolley |
| Right | 3 | 6 | 0.387 |
| Left | 7 | 5 |
| Position of Ultrasound machine |
| Front in line | 10 | 5 | 0.0124 |
| Not in line | 0 | 6 |
p<0.05 significant
Discussion
The current study found that the performance of USG TAP block in a setting described is usually ergonomically sub-optimal. Operators assume unstable position to coordinate hand eye movements during the procedure. Lack of attention to check the position of machine, patient, assistant, tray in the available space and time pressure were other contributing factors.
In this study the experienced operators appeared to perform better in terms of ergonomics compare to novice operators which is in accordance with the study conducted by Ajmal M et al., where all the experienced operators performed better than the novice ergonomically [16].
The mean difference of height of E operator was 12.7±5.9 cm and N was 6.8±6.3 cm. The difference was statistically significant. Experience operator (7) sat and adjusted their chair to maintain eye level on the screen of ultrasound machine; whereas only 2N sat and others flexed their back to visualise the screen. Chapman GA et al., suggested to keep the US screen at the eye level of the operator in front, in his description of dynamic interaction between operator and ultrasound machine [19]. He also stated that the operator must focus on the monitor and on the patient, hence the importance of having anatomical area and ultrasound machine in same line of view. This was supported by another study [15], which suggested the adjustments of operator chair and ultrasound monitor should be done to avoid neck extension. The authors also suggested that neck should be slightly flexed to approximately 15-20° during procedure. Morton B, Delf P stated that short stature can increase the risk of Work Related Musculoskeletal Disorders (WRMSD), which may be due to the need to over extend while scanning [20].
Mathews AJ et al., and Walker J in two identical studies of posture of anaesthetists during laryngoscopy and intubation, linked improper posture with immediate outcome of the procedure and its aesthetic appreciation [21,22]. They also stressed that the posture of novice were incorrect when compared to experienced operators. Similar findings were seen in this study. Novice operators had rotated their head, neck, trunk more than the experienced. Maintaining incorrect posture puts stress on joints and its associated muscles and it reduces the performance of the operator. Most commonly affected joints are shoulders (76%), neck (74%), wrists (59%) and back 58% [23]. Baker JP and Coffin CT also stated that twisting of the body during sonography can lead to back pain and injury [15]. He also stressed the importance of ergonomic workstation in his review to reduce the incidence of Work Related Musculoskeletal Disorders (WRMSD) for sonographers.
Anson JA et al., found the prevalence of back pain among anaesthesiologists to be 46.6% [24]. More over 70% of the study participants had no low back symptoms prior to anaesthesia training. Janki S et al., stated that musculoskeletal complaints and subsequent work absence are still present among surgeons especially with positive medical history [25]. He also stated that half of the respondents with complaints made intraoperative ergonomic adjustments to prevent future complaints. To maintain optimal position during UGRA procedures, the ergonomic work area should include adjustable table with lateral retractile supports, adjustable chairs with wheels, spacious rooms with indirect light to avoid glare on the monitor [15].
Speer M et al., described two ways to position the transducer and needle in relation to visual axis of the operator while performing in plane needle insertion [26]. He also found that when two axes are parallel there is significant reduction in time to perform block and improved image quality. This is supported by Sundaram S et al., who stated that keeping the monitor in front in line made the operators more comfortable during the procedure and it also improved the performance of block [27]. However, in this study except 10E and 5N, others rotated their neck either <45° or >45° to visualise the screen which was not kept in line. It is stated that neck is a common site of injury and 65.8% of sonographers suffered from neck pain or discomfort [23].
Wilson JM et al., also supported that Along the Line of Visual Axis (ALVA) technique which had improved the performance of procedure ergonomically in short time with high success rate [28]. Langford RA et al., had stated that the needle placement was significantly more accurate when ultrasound machine was kept in front compare to same side, in his single blinded study on accuracy and speed of USG block with two different monitor positions [29].
In this study, 7E and 2N operators sat during the procedure and their forearms were horizontal to floor. This is in accordance with Murphy C and Russo A who suggested that forearm should be horizontal to floor to keep the shoulder in neutral [30], which is also stressed by Baker JP and Coffin CT to reduce the incidence of injury [15]. When procedure is performed in standing posture, the operators are advised to stand with both feet placed firmly on the floor and keep the shoulder vertical to the side of the body to avoid rotation of the body.
Baker JP and Coffin CT; and Coffin C and suggested the best practices like slight neck flexion 15-20°; forearm horizontal to couch; shoulder vertical at the side of body while scanning to reduced Work Related Musculoskeletal Disorders (WRMSDs) [15,31]. Even though it had been suggested for sonographers, similar consideration will be useful for anaesthetists as suggested by Ospina ODA et al., [32]. He described appropriate ergonomics for all regional techniques like working from a sitting position with the arm supported on bed; avoid inadequate positioning of hand, wrists, neck, trunk and shoulders. Height of the table should be adjusted and ultrasound machine should be placed on the opposite side of the body where the nerve blocks would be performed rotation of the head 450 or more should be avoided. Dominant hand should be used and pinch grip should be avoided to improve the performance of block and to reduce the incidence of WRMSD.
Udani AD et al., in his study on ergonomic behaviour between novice and experienced anaesthesiologists during simulated USG popliteal sciatic nerve black using head mounted display on porcine model found that [33], both performed the procedure without directly viewing the ultrasound monitor and neither showed poor ergonomic behaviour. Novice operator preferred head mounted display because of ease of needle control and hand eye coordination.
Limitation(s)
Even though the data were collected by single investigator to reduce the observer bias, the practicing anaesthesiologists were aware of the study.
Conclusion(s)
Ultrasound improve the safety and efficacy of regional anaesthetic techniques. To attain success without any complication, not only knowledge of anatomy is sufficient but also understanding and application of the ergonomic aspects relevant to regional anaesthesia procedure is must. Compared to experienced anaesthesiologists, novice lacks these skills. Inclusion of ergonomic concepts in academic training programme will improve the performance of novice.