Blepharoptosis means drooping of the upper eyelid and when it is present since birth it is known as congenital ptosis. There is abnormal growth and fatty infiltration of the levator palpebrae superioris muscle which causes fibrosis of the muscle in congenital ptosis [1]. Congenital ptosis not only causes cosmetic problem but also results in visual disturbance which results in amblyopia. Amblyopia occurs if the visual axis is obscured by the droopy eyelid or due to associated corneal astigmatism. In ptosis, intervention is required if it obscures the visual axis causing amblyopia, if child develops abnormal head tilt and sometimes for improving the cosmetic appearance of the child [2]. The unpredictable nature of various surgical techniques performed for treating congenital ptosis with poor levator action is still one of the most difficult tasks for oculoplastic surgeon as surgical procedure is often associated with complication like under-correction, lid asymmetry and poor cosmetic results [2,3].
Frontalis sling surgery has been recommended in the treatment of unilateral ptosis in the past decades. In sling surgery the frontalis muscle is connected with upper tarsal plate which results in better eyelid position in primary gaze and causes elevation of the eyelid whenever frontalis muscle is in action [4]. However, it is associated with complication like sling expulsion, exposure, infection, brow scar, suture granuloma and cosmetic disfigurement [5]. Levator resection yields good cosmesis in terms of acceptable lid contour and symmetry but always result in under-correction. The difficulty in managing unilateral congenital ptosis with poor levator action still persists and the ideal surgical procedure is still evolving [6].
The result in various published data about different surgical procedures for treating congenital ptosis varies. The tarso-frontalis sling surgery is easy to perform but has a high recurrence rate [7-10]. The need of one more procedure to address these issues results in dissatisfaction among patients. This study was executed at the study centre to analyse the postoperative surgical outcomes after supramaximal levator resection in congenital ptosis with poor levator resection and it was a first of its kind in Armed Forces population.
Materials and Methods
A longitudinal study was conducted over a period of six months from July 2019 to December 2019, in the eye department of a Tertiary Care Centre. This study adhered to the tenets of the Declaration of Helsinki.
Inclusion criteria: A total of 15 patients diagnosed with unilateral simple congenital ptosis with poor levator action were included in this study after obtaining informed consent from patients’s next of kin.
Exclusion criteria: Patient with Marcus Gunn jaw-winking phenomenon were excluded from this study.
All patients (n=15) of unilateral congenital ptosis underwent supramaximal levator resection during the study period and all were followed-up for another six months. In all cases detailed history was taken and patients underwent comprehensive eye check-up. Ocular examination included vision, refraction, external and fundus examination. Ptosis examination included measuring vertical palpebral fissure height, margin reflex distance, upper lid crease position, levator muscle action, Bell’s phenomenon and the presence of Marcus Gunn jaw-winking phenomenon [Table/Fig-1]. Margin reflex distance-1 was defined as the distance between the corneal light reflection and the upper eyelid margin (normal value is 4-4.5 mm). The vertical palpebral fissure is the distance between the upper and lower lid margin while the patient is in primary gaze (normal range vary from 8-12 mm). Levator muscle action was defined as excursion of the upper lid from extreme downgaze to extreme upgaze was recorded. Levator function was divided into three groups depending on the amount of lid movement: good (action >8 mm), fair (5-7 mm), and poor (0-4 mm) [11].
Clinical photograph showing unilateral congenital ptosis (black arrow).

Surgical outcome measures were change in margin reflex distance-1, vertical palpebral fissure height and inter-eyelid difference of margin reflex distance-1 with clear visual axis with the eyes in the primary position and resolution of any head tilt. A good surgical outcome was defined as MRD-1 3-4 mm and inter-eyelid difference of MRD-1 between 0.5 to 1 mm in unilateral cases at the last follow-up visit.
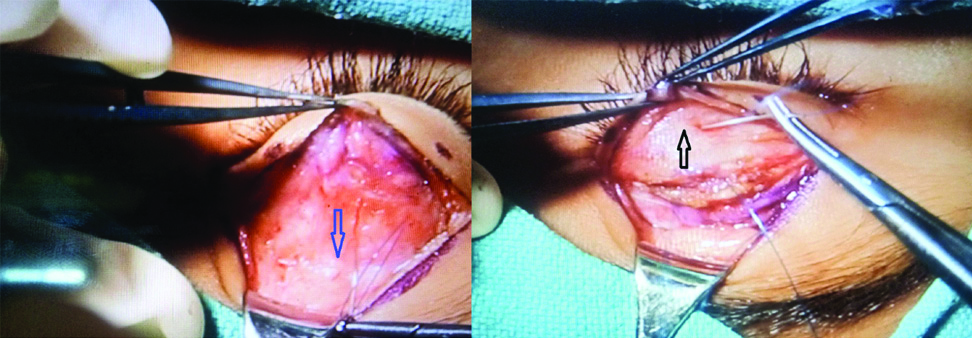
Surgical technique: The surgical technique, which was performed by the same surgeon, involved first making a skin incision to match the contralateral lid crease, if present or 10 mm away from the lid margin. Incision was made with radiofrequency cautery and dissection was done in suborbicularis plane to expose the upper third of the tarsal plate. The undersurface of the levator muscle was dissected from the underlying Muller’s muscle and the conjunctiva. The septum was incised to expose the levator, till Whitnall’s ligament, after retracting the preaponeurotic fat. A 6-0 prolene suture was passed through partial thickness of the tarsus at junction of upper two third and lower one third, then it was placed posterior to the levator muscle and then retrieved through the levator muscle inferior to Whitnall’s ligament [Table/Fig-2]. Two more sutures were passed between the levator muscle near to Whitnall’s ligament and the tarsus on medial and lateral side. Three sutures were adjusted as needed and levator was excised. Lid crease was formed by taking the bite through subepidermal area, stump of levator and preseptal orbicularis layer with 6-0 vicryl. Finally, skin was closed with 6-0 vicryl and frost suture was applied to avoid exposure keratopathy in the postoperative period. The eyelid position was adjusted intraoperatively using Berke’s rule as guide to the expected postoperative descent of the eyelid and hence, the upper eyelid was placed at superior limbus as the levator muscle action was poor in all cases [11,12]. Postoperative antibiotic eye drops for one week and lubricants for six weeks were prescribed. The last visit follow-up data with all the measurements were compared with the preoperative data.
Intraoperative photograph showing dissected levator muscle upto Whitnall’s ligament with placement of suture below Whitnall’s ligament (blue arrow) and through tarsal plate (black arrow).
Postoperative evaluation was done on first day, after one week, one, three and six month. The main surgical parameter/outcomes which assessed during each follow-up visit were MRD-1, vertical palpebral fissure height, inter-eyelid difference of MRD-1, eyelid contour and its comparison with normal eyelid and condition of visual axis of the operated eyelid. Clinical photograph was taken in each visit.
Statistical Analysis
The data collected was entered in Microsoft Excel 2007 and analysed using Epi info version 3.4.3. Mean, standard deviation and percentages were calculated for preoperative and postoperative examination findings. Paired t-test was applied to determine any statistical difference. A p-value of <0.05 was taken as statistically significant. Ninety-five percent confidence interval for the difference of proportion was also calculated.
Results
A total of 15 patients with congenital ptosis with poor levator action underwent supramaximal levator resection. There were 10 females (60%) and 5 males (40%) in the study group. The mean age group at the time of ptosis surgery was 5.73±0.55 years (range from 03 and 11 years). The preoperative [Table/Fig-3] and postoperative evaluation [Table/Fig-4] included recording of vertical fissure height, margin reflex distance and inter-eyelid difference of margin reflex distance which were correlated [Table/Fig-5].
Preoperative examination findings of the patients.
| Patient | Age | Gender | MRD-1 (mm) | VPFH (mm) | Inter-eyelid MRD-1 (mm) difference | LA | Upper LC |
|---|
| 1 | 3 | Female | 1 | 6 | 3 | Not recorded | Absent |
| 2 | 4 | Female | 1 | 6 | 3 | 3 | Absent |
| 3 | 3 | Female | 0 | 5 | 4 | 3 | Absent |
| 4 | 3 | Female | 1 | 6 | 3 | 2 | Absent |
| 5 | 6 | Female | -1 | 4 | 5 | 4 | Faint |
| 6 | 8 | Female | -1 | 6 | 3 | 4 | Faint |
| 7 | 11 | Female | 0 | 5 | 4 | 3 | Absent |
| 8 | 3 | Female | 1 | 6 | 3 | Not recorded | Absent |
| 9 | 5 | Male | 1 | 6 | 3 | 3 | Absent |
| 10 | 6 | Male | 0 | 5 | 4 | 4 | Faint |
| 11 | 8 | Male | -1 | 4 | 5 | 2 | Absent |
| 12 | 10 | Male | 0 | 5 | 4 | 4 | Faint |
| 13 | 5 | Female | 0 | 5 | 4 | 4 | Faint |
| 14 | 8 | Female | -1 | 4 | 5 | 2 | Absent |
| 15 | 3 | Male | 1 | 6 | 3 | Not recorded | Absent |
MRD: Margin reflex distance; VPFH: Vertical palpebral fissure height; LA: Levator action; LC: Lid crease
Postoperative findings of all operated patients.
| Patient | MRD-1 (mm) | VPFH (mm) | Inter-eyelid MRD-1 (mm) difference |
|---|
| 1 | 4 | 9 | 0 |
| 2 | 3.5 | 9 | 0.5 |
| 3 | 3.5 | 9 | 0.5 |
| 4 | 3 | 8 | 1 |
| 5 | 2 | 7 | 2 |
| 6 | 3.5 | 8.5 | 0.5 |
| 7 | 4 | 9 | 0 |
| 8 | 3 | 8 | 1 |
| 9 | 3.5 | 9 | 0.5 |
| 10 | 2 | 7 | 2 |
| 11 | 3.5 | 9 | 0.5 |
| 12 | 3 | 8 | 1 |
| 13 | 4 | 9 | 0 |
| 14 | 3.5 | 8.5 | 0.5 |
| 15 | 3 | 8 | 1 |
MRD: Margin reflex distance; VPFH: Vertical palpebral fissure height
Comparison between preoperative and postoperative surgical outcome parameters.
| Parameter | Preoperative mean | Postoperative mean | p-value | 95% CI |
|---|
| MRD-1 | 0.26±0.77 mm | 3.26±0.6 mm | <0.0001 | 2.48 to 3.51 |
| VPFH | 5.26±0.77 mm | 8.4±0.68 mm | <0.0001 | 2.59 to 3.68 |
| Inter eyelid MRD-1 difference | 3.73±0.62 mm | 0.73±0.62mm | <0.0001 | 2.53 to 3.46 |
Values are represented as Mean±SD. All measurements are in millimetres. p-value of less than 0.05 is considered as significant. Favourable outcome is defined as MRD-1, within 1 mm of the contralateral eye. MRD1, margin reflex distance; PFH, palpebral fissure height
The mean preoperative levator action was 3.16±0.79 mm. Vertical palpebral fissure height increased from mean of 5.26±0.77 mm to a mean of 8.4±0.68 mm (p<0.0001; 95% CI, 2.59 to 3.68) postoperatively after one week which remained same at the last visit (after six months of surgery) . Margin reflex distance-1 increased from a mean of 0.26±0.77 mm to 3.26±0.6 mm (p<0.0001; 95% CI, 2.48 to 3.51) postoperatively after one week which remained same after 06 months and the range was 2. Inter-eyelid difference of margin reflex distance-1 decreased from mean of 3.73±0.62 to 0.73±0.62 mm (p<0.0001; CI, 2.53 to 3.46) postoperatively after one week which remained same after six months. The mean MRD in normal eye was 4 mm. A visible improvement was noted in the lid height and contour with clear visual axis in all patients [Table/Fig-6].
One week postoperative clinical photograph showing improvement following ptosis correction with levator resection (black arrow).

Complications which were encountered were under-correction as MRD-1 was 2 mm in two patients (13.3%) and upper lid swelling in one patient (6.6%), which persisted even after one week of surgery. As visual axis was clear in two cases after one month in whom under-correction (MRD-1 remained 2 mm) was found, observation was advised and three monthly follow-up. Upper lid swelling subsided after a seven days course of Antinflammatory medications.
Discussion
Supramaximal levator resection for severe unilateral ptosis was first introduced in 1984 [13]. Levator resection results in better cosmesis such as the presence of dynamic blink, preservation of natural eyelid contour and a lack of dependency on the frontalis muscle action for opening eyes compared to frontalis suspension surgery. In this study, all patients with poor levator action subjected to supramaximal levator resection instead of tarsofrontalis sling operation. The supramaximal levator resection attained good surgical outcomes for congenital ptosis with poor levator action in 80% of cases as postoperative MRD-1 was found to be 3 mm. These patients had an excellent reduction in ptosis with a free visual axis, reducing the risk of amblyopia. These study findings are in concordance with Cruz AA et al., and Mete A et al., that achieved success rate of 91.4% and 70% in their study, respectively [3,14]. In the study by Chen W et al., which reported excellent results in 8 out of 10 (80%) patients in unilateral congenital ptosis and in 14 of 15 patients (93.3%) in bilateral condition with levator action of 4 mm or less, who underwent maximal levator resection [15]. Supramaximal levator resection was also reported to be effective for correction of congenital ptosis associated with blepharophimosis syndrome in a study by Decock CE et al., [16].
However, Pak J et al., showed good outcome only in 2 of 7 cases (28.6%) and Park DH et al., reported satisfactory outcome in 35 of 65 cases (53.9) [17,18]. Anderson RL et al., also reported success rate of 71% over a one year follow-up in patients, who were treated with supramaximal levator muscle resection [19].
In some patient’s, undercorrection was noticed; however visual axis was clear so observation was advised in these two cases. Postoperatively patient had lagophthalmos and lid lag on downgaze which became less visible after three months. It happened because pretarsal orbicularis muscle regained its strength within few months postoperatively.
Limitation(s)
The limitation of this study is that the surgical outcomes of supramaximal levator resection were not compared with tarsofrontalis sling operation. The other limitation of this study includes its small sample size and short follow-up. A larger study group would be helpful to validate the surgical effectiveness of maximal levator resection.
Conclusion(s)
Levator resection is an effective alternative for tarsofrontalis sling operation as it leads to good surgical outcomes in patients diagnosed with congenital ptosis. It allows normal physiological use of levator action, despite its poor function in congenital ptosis which yields good result by avoiding all complications which are associated with tarsofrontalis sling operation.
MRD: Margin reflex distance; VPFH: Vertical palpebral fissure height; LA: Levator action; LC: Lid crease
MRD: Margin reflex distance; VPFH: Vertical palpebral fissure height
Values are represented as Mean±SD. All measurements are in millimetres. p-value of less than 0.05 is considered as significant. Favourable outcome is defined as MRD-1, within 1 mm of the contralateral eye. MRD1, margin reflex distance; PFH, palpebral fissure height