Stroke is the second leading cause of death. It carries a significant personal, social and financial global burden [1]. Incidence of stroke is higher in developing countries than in developed countries [2]. India shows prevalence of CVD in the range of 52 to 843/100,000 population [3]. The incidence rate is 119-145/100,000 [4]. In India, stroke patients are relatively younger [average age ≥60 years compared to the West (≥65 years) [5]. Since women have longer life expectancies, there is higher stroke prevalence in women [6]. Stroke causes 9% deaths around the world. Death from stroke in the low-income and middle-income countries accounted for 85.5% of stroke deaths worldwide [7]. The socio-economic impact due to stroke on individual, families and health care institutions is enormous [8].
About 85% of all first-time strokes are ischaemic, 10% due to primary intra-cerebral haemorrhages and 5% due to subarachnoid haemorrhages [9]. Athero-thrombosis is the leading cause of stroke [10]. Hypertension, smoking, obesity, excess alcohol intake are the other risk factors for stroke [4].
According to Rajegowda ST et al., stroke related morbidity and mortality could be minimised with early medical interventions. The knowledge on stroke is important in early detection of stroke, and socio-cultural factors may influence access to medical care for many stroke victims [11].
The basic principle of managing stroke includes making an accurate diagnosis, choosing the effective drugs and dose for the stroke type. This study intended to understand the characteristics of patients with stroke and to analyse the variations and its determinants in the pharmacotherapy thereby generate useful data for improving the outcome of treatment. It also intended to get data about the frequency of different types of stroke in the region and to assess the adverse drug reactions; to follow-up the patient for continuation of therapy for secondary prevention of stroke which is the management for life time of the individual involving medical, social and family care.
Materials and Methods
This cohort study was carried out in the Department of Medicine and Neurology at Karnataka Institute of Medical Sciences, Hubballi from January 2015 to December 2015. Study approval was obtained from Institutional Ethics Committee (984/2014-2015).
Inclusion criteria: Patients diagnosed with stroke of any type in the last six months, either initial or recurrent, were included in the study.
Exclusion criteria: Patients treated elsewhere and referred to this hospital for further management without adequate and reliable information on prior treatments received, severely aphasic and demented patients, with no relatives or friends who can provide reliable history were excluded.
After informed consent was obtained from the patients or their relatives, patients were interviewed within 48 hours of admission to the hospital and were again interviewed one day prior or at the time of discharge to collect relevant data.
Patients were followed-up during their visit to the hospital at three and six months. The patients who did not visit the hospital or missed the follow-up were interviewed over a telephone call. Three attempts per patient were made at different times and if unsuccessful, such patients were declared as lost to follow-up.
The data were collected in a specially designed case record form. The data were broadly classified into demographic data, clinical data, treatment at admission and discharge and complications and adverse reactions during hospital stay. Patient’s basic details, present stroke history (onset of symptoms, presentation at hospital, National Institutes of Health Stroke Scale Score (NIHSS) [12] on admission and Modified Rankin Score on discharge and on follow-up), history of chronic diseases, personal history (smoking, alcoholism), drug treatment received in the hospital and outcome. Patients were followed-up at three and six months.
Modified Rankin Scale (mRS) [12] was used to assess the degree of disability or dependence in the daily activities of the patients with stroke and was considered as the study included follow-up also. The scale includes scores from 0 to 6 [Table/Fig-1].
Modified Rankin Scale (mRS).
| 0. No symptoms at all. |
| 1. No significant disability despite symptoms (Able to carry out all usual activities). |
| 2. Slight disability. |
| 3. Moderate disability (Requiring some help but able to walk without assistance). |
| 4. Moderate to severe disability (Unable to walk without assistance and unable to attend to own bodily needs without assistance). |
| 5. Severe disability (Bed-ridden, incontinent and requiring constant nursing care). |
| 6. Death. |
Sample size estimation: Sample size calculation was made using the following formula: n=Z2 p (1-p)/e2, where n=required minimum sample size, e=margin of error (5%) [13], p=estimated proportion (12%) z=standard normal deviate corresponding to 95% confidence level=1.96 and was estimated to be 162.
Statistical Analysis
The data were entered after defining the variables in SPSS (version 16) from case record form. Descriptive statistics were used to summarise baseline data. Continuous data such as age, Blood Pressure (BP), blood sugar, blood cholesterol were analysed using Student’s t-test and categorical data such as severity of stroke, death and drug usage were analysed using Chi-square test. Mann-Whitney U test was used to analyse ordinal data. Repeated measures ANOVA was used to compare means at different time intervals from admission, discharge, three months and six months. Multiple binary logistic regressions were used to determine factors that influenced mortality at six months. The mean survival time of ischaemic stroke and haemorrhagic stroke were compared using log rank test. The data of patients with ischaemic stroke and haemorrhagic stroke were compared using Chi-square test. A p-value of less than 0.05 was considered significant.
Results
In the present study, a total of 162 patients were recruited in a period of 12 months. Seven patients were excluded from study because they were lost to follow-up (two patients discharged against medical advice and five lost follow-up at six months). A total of 155 patients completed the study. The demographic characteristics of the patients are presented in [Table/Fig-2].
Socio-demographic details of the patients (N=155).
| Characteristics | Frequency | Percentage |
|---|
| Age (years) |
| ≤60 | 88 | 56.77 |
| >60 | 67 | 43.23 |
| Sex |
| Male | 108 | 69.67 |
| Female | 47 | 30.32 |
| Marital status |
| Single | 5 | 3.22 |
| Married | 150 | 96.77 |
| Education |
| Illiterate | 55 | 35.48 |
| Primary school | 62 | 40 |
| Secondary school | 31 | 20 |
| Post-secondary | 7 | 4.5 |
| Occupation |
| Government employee | 9 | 5.8 |
| Nongovernment employee | 28 | 18 |
| Self-employed | 65 | 41.9 |
| Unemployed | 53 | 34.2 |
| Place |
| Urban | 105 | 67.74 |
| Rural | 50 | 32.25 |
Clinical Data
There were 130 (83.87%) patients of ischaemic stroke, 16 (10.30%) haemorrhagic stroke {15 (9.67%) were intracerebral haemorrhage + 1 (0.63%) patient had a subarachnoid haemorrhage} and 9 (5.8%) had a TIA.
Median time: The median time taken to reaching the tertiary care hospital from symptom onset in acute ischaemic stroke was 10 hour 45 minutes, for haemorrhagic stroke it was six hours and for TIA it was 13 hours. Twenty (15.38%) ischaemic stroke patients presented within three hour, 95 (73.07%) patients presented between 3 to 24 hours of symptom onset and 15 (11.53%) patients presented after 24 hours. Detailed data are available in [Table/Fig-3].
Time taken to reach hospital after symptom onset.
| Time taken from symptom onset to reaching emergency dept | TIA | Ischaemic | Haemorrhagic |
|---|
| (n=9) | (n=130) | (n=16) |
|---|
| Median time | 13 | 10.45 | 6 |
| <3 hours (n) | 2 | 20 | 4 |
| 3-6 h (n) | 3 | 32 | 3 |
| 6-12 h (n) | 1 | 38 | 3 |
| 12-24 h (n) | 1 | 25 | 2 |
| >24 h (n) | 2 | 15 | 4 |
Blood Pressure (BP): The mean BP during admission and discharge were 146/90 and 130/80 mmHg in ischaemic stroke, 130/88 and 120/80 mmHg in TIA and 160/100 and 130/84 mmHg in haemorrhagic stroke patients. A mean reduction in BP was 16/10 mmHg in ischaemic stroke, 10/8 mmHg in TIA and 30/16 mmHg in haemorrhagic stroke as shown in [Table/Fig-4].
| Risk factors | Ischaemic stroke | Haemorrhagic stroke | p-value |
|---|
| Hypertension | 98 (75.38%) | 14 (87.5%) | 0.587 |
| Diabetes mellitus | 78 (60%) | 6 (37.5%) | 0.311 |
| h/o Myocardial infarction | 24 (18.46%) | 0 | 0.27 |
| h/o Stroke | 35 (26.92%) | 1 (6.25%) | 0.514 |
| h/o TIA | 15 (11.53%) | 1 (6.25) | 0.05* |
| h/o Atrial fibrillation | 2 (1.54%) | 0% | 0.522 |
| Tobacco use | 64 (49.23%) | 5 (31.25%) | 0.514 |
| Alcoholism | 66 (50.76%) | 6 (37.5%) | 0.059 |
Risk factors for stroke were analysed using Chi-square test. A p-value of less than 0.05 was considered statistically significant*; h/o: History of; TIA: Transient ischaemic attack
Investigations: The mean random blood sugar during admission for ischaemic stroke patient (169.2 mg/dL) was more compared to haemorrhagic stroke (134.8 mg/dL) and TIA (109.5 mg/dL). A review of the lipid profile during admission (mean values of the baseline investigations) is shown in [Table/Fig-5].
Mean random blood sugar and lipid profile during admission.
| Investigations mean (SD) (n) in mg/dL | TIA (n=9) | Ischaemic (n=130) | Haemorrhagic (N=16) |
|---|
| RBS | 109.5 (28.2) (n=9) | 169.2 (81.8) (n=119) | 134.8 (57.5) (n=15) |
| Cholesterol | 158.4 (26.3) (n=5) | 188.5 (48.8) (n=78) | 160 (41.6) (n=10) |
| HDL | 30.8 (5.8) (n=5) | 26.6 (8.2) (n=78) | 39.70 (11.9) (n=1) |
| LDL | 108.2 (20.8) (n=4) | 129.6 (80.89) (n=73) | 102.4 (32.16) (n=11) |
| TG | 111.1 (73.7) (n=5) | 135.6 (90.2) (n=78) | 106.9 (67.8) (n=11) |
RBS: Random blood sugar; HDL: High density lipopolysaccharide; LDL: Low density lipopolysaccharide; TG: Triglycerides
Modified Rankin score: The mean mRS at admission was lower in TIA patients (2.5), as compared to ischaemic (3.9) and haemorrhagic (5.1). This order continued at discharge and follow-up. There was a significant difference in improvement of modified Rankin score (1.29, p=0.0035) between admission and discharge. Similar significant mean difference was found at three and six months (0.9, p=0.003). This means both ischaemic and haemorrhagic stroke patients showed improvement in the modified Rankin score after three months following the onset of symptoms [Table/Fig-6].
Temporal changes in mean mRS at admission, discharge, three months and six months.
| Modified Rankin score Mean, (SD) | TIA | Ischaemic | Haemorrhagic | p-value |
|---|
| Admission | 2.5 (0.9) | 3.9 (1.1) | 5.1 (1) | 0.0035 |
| Discharge | 1.83 (1) | 2.6 (1.2) | 3.2 (1.1) | 0.0035 |
| Three months | 1.1 (1.23) | 2.1 (1.33) | 2.6 (1.24) | 0.003 |
| Six months | 1.04 (1.42) | 1.5 (1.4) | 2.1 (1.36) | 0.003 |
mRS: Modified rankin score; TIA: Transient ischaemic attack; p-value <0.05 was considered statistically significant
Complications during Hospital Stay
In patients with TIA [9] there were no complications observed during hospital stay. Total 57 patients in ischaemic stroke and 14 patients in haemorrhagic stroke group had complications during hospital stay. No statistically significant difference was observed. [Table/Fig-7].
Complications/outcomes during hospital stay.
| Complications | Ischaemic (n=130) | Haemorrhagic (n=16) | p-value |
|---|
| Death | 1 (0.76) | 4 (25%) | 0.874 |
| UTI | 19 (14.61) | 2 (12.5%) | 0.771 |
| Seizure | 4 (3.07%) | 2 (12.5%) | 0.398 |
| Pneumonia | 4 (3.07%) | 1 (6.25%) | 0.315 |
| Hyponatremia | 12 (9.23%) | 2 (12.5%) | 0.669 |
| Hypokalemia | 9 (6.9%) | 1 (6.25%) | 0.838 |
| Renal Failure | 2 (1.53%) | 0 | 0 |
| DVT | 2 (1.53%) | 0 | 0 |
| Bed sore | 4 (3.07%) | 2 (12.5%) | 0.378 |
Complications/outcomes during hospital stay were analysed using Chi-square test. A p-value of less than 0.05 was considered statistically significant*; UTI: Urinary tract infection; DVT: Deep vein thrombosis
Events during Follow-Up
Treatment discontinuation: Of 155 patients, 24 (15.4%) patients stopped all drugs during follow-up. Of these 19 had an ischaemic stroke, 2 had TIA and 1 had haemorrhagic stroke. The reasons given by the patients included:
Complete improvement
Changing over to alternative medicine such as Ayurveda, Homeopathy and oil massages with the belief of better and complete recovery
No improvement/partial recovery in the condition
Cost of the drugs
General view of adverse effects in allopathic medicines with long treatment advised for secondary prevention of stroke.
Follow-up discontinuation: Of the total 162 patients, 7 (4.32%) patients were lost to follow-up (5 from haemorrhagic stroke and 2 from TIA).
Treatment Data
Transient Ischaemic Attack (TIA): Antiplatelets use showed a decreasing trend from admission (100%) to six months (55.5%). Amlodipine was the most commonly used drug in TIA patients during admission (55.5%). All antihypertensive drugs showed decreasing trend [Table/Fig-8].
Treatment details for the Transient Ischaemic Attack (TIA) patients (N=9).
| Drugs | Admission | Discharge | Three month | Six months |
|---|
| Antiplatelets | 9 (100%) | 8 (88.8%) | 6 (66.6%) | 5 (55.5%) |
| Aspirin | 6 (66.6%) | 4 (44.4%) | 4 (22.2%) | 3 (33.3%) |
| Clopidogrel | 3 (33.3%) | 4 (44.4%) | 2 (22.2%) | 2 (22.2%) |
| Anticoagulants | 4 (44.4%) | 3 (33.3%) | 2 (22.2%) | 1 (11.1%) |
| Low Molecular Weight Heparin (LMWH) | 4 (44.4%) | 1 (11.1%) | 0 | 0 |
| Warfarin | 0 | 2 (22.2%) | 2 (22.2%) | 1 (11.1%) |
| Antihypertensives | 9 (100%) | 8 (88.8%) | 6 (66.6%) | 4 (44.4%) |
| Atenolol | 3 (33.3%) | 2 (22.2%) | 1 (11.1%) | 0 |
| Amlodipine | 5 (55.5%) | 4 (44.4%) | 4 (44.4%) | 0 |
| Enalapril | 3 (33.3%) | 2 (22.2%) | 2 (22.2%) | 3 (33.3%) |
| Losartan | 3 (33.3%) | 3 (33.3%) | 2 (22.2%) | 1 (11.1%) |
| Lipid lowering agents | 9 (100%) | 9 (100%) | 7 (77.7%) | 5 (55.5%) |
| Atorvastatin | 9 (100%) | 9 (100%) | 7 (77.7%) | 5 (55.5%) |
| Fenofibrate | 1 (11.1%) | 1 (11.1%) | 0 | 0 |
Thrombolytic therapy in ischaemic stroke: Of the 20 (15%) patients with ischaemic stroke that reached hospital within three hours of symptom onset, two of them received thrombolytic therapy.
Antiplatelet Therapy
Ischaemic stroke: A total of 121 (93%) patients with ischaemic stroke received antiplatelets. Majority of patients with ischaemic stroke continued with single antiplatelet (aspirin) for long term management (33 patients discontinued treatment).
Anticoagulants: Of 130 ischaemic patients, during admission, 37 (28.4%) received Low Molecular Weight Heparin (LMWH) to prevent deep vein thrombosis, 2 (1.5%) patients were on warfarin for Cerebral Venous Thrombosis (CVT) [Table/Fig-9,10].
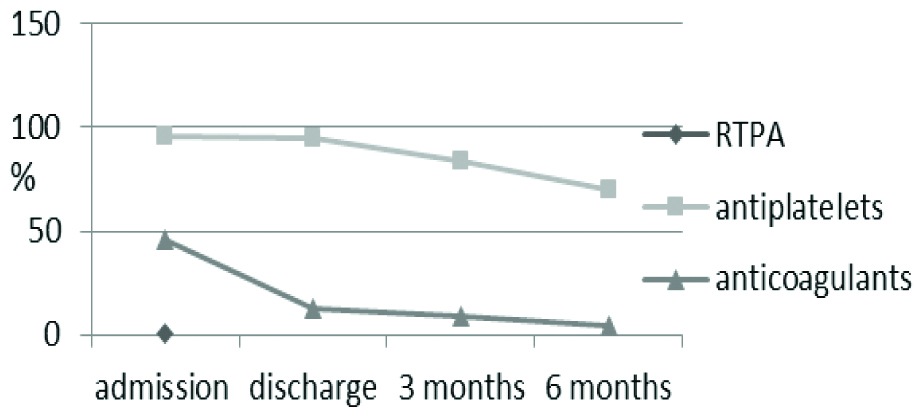
Use of thrombolytic (Recombinant Tissue Plasminogen Activator, RTPA), antiplatelets and anticoagulant for ischaemic and haemorrhagic stroke patients.
| Medications/Therapies | Ischaemic | Haemorrhagic |
|---|
| Admission (n=130) | Discharge (n=106) | Three months (n=101) | Six months (n=91) | Admission (n=16) | Discharge (n=14) | Three months (n=12) | Six months (n=11) |
|---|
| RTPA | 2 (1.53%) | - | - | - | - | - | - | - |
| Aspirin | 100 (76.9%) | 89 (83.9%) | 70 (69.3%)a | 59 (64.8%)C | 1 (6.2%) | 1 (7.1%) | 1 (8.3%) | 1 (9%) |
| Clopidogrel | 86 (66.1%) | 80 (75.4%) | 57 (56.4%)b | 25 (27.4%)d | 1 (6.2%) | 2 (14.2%) | 1 (8.3%) | 1 (9%) |
| LMWH | 37 (28.4%) | 7 (6.6%) | 1 (0.9%) | 0 | 3 (18.7%) | 1 (7.1%) | 2 (16.6%) | 0 |
| Warfarin | 2 (1.5%) | 6 (5.6%) | 4 (3.9%) | 2 (2.19%) | 0 | 0 | 1 (8.3%) | 1 (9%) |
aUse of aspirin showed a decreasing trend at three month compared to admission with statistical significance (McNemar test: p=0.0411); bClopidogrel use showed a decreasing trend at one month compared to admission with statistical significance (McNemar test: p=0.048); cThe use of aspirin showed a decreasing trend at six months compared to admission with statistical significance (McNemar test: p=0.0021); dClopidogrel use showed a decreasing trend (McNemar test: p=0.0121); LMWH: Low molecular weight heparin
p-value <0.05 was considered statistically significant
Use of thrombolytic, antiplatelets and anticoagulants for ischaemic and haemorrhagic stroke patients.
RTPA: Recombinant tissue plasminogen activator
Antihypertensives: Amlodipine 5 mg/OD was the most commonly prescribed antihypertensive. The target BP was 130/80 at the end of five days of initiating the treatment. The trend of antihypertensive use fell from admission to six months. However, patients showed reduced compliance to all medications [Table/Fig-11].
Use of antihypertensive drugs in ischaemic and haemorrhagic stroke patients.
| Medications used | Ischaemic | Haemorrhagic |
|---|
| Admission | Discharge | Three months | Six months | Admission | Discharge | Three months | Six months |
|---|
| (n=130) | (n=108) | (n=101) | (n=91) | (n=16) | (n=14) | (n=12) | (n=11) |
|---|
| Atenolol | 11 (8.4%) | 11 (10.1%) | 8 (7.9%) | 1 (1%)i | 2 (12.5%) | 2 (14.2%) | 2 (16.6%) | 0 |
| Metoprolol | 3 (2.3%) | 3 (2.7%) | 3 (2.9%) | 2 (2.1%) | 1 (6.2%) | 1 (7.1%) | 0 | 1 (9%) |
| Carvedilol | 1 (0.7%) | 4 (3.7%) | 5 (4.9%) | 0 | 0 | 1 (7.1%) | 0 | 0 |
| Amlodipine | 81 (62.3%) | 73 (67.5%)f | 62 (61.3%)g | 4 (4.3%)h | 10 (62.5%) | 10 (71.4%) | 6 (50%) | 8 (72.7%) |
| Ramipril | 51 (39.2%) | 57 (52.7%) | 48 (47.5%) | 32 (35.1%) | 9 (56.2%) | 11 (78.5%) | 8 (66.6%) | 3 (27.2%) |
| Enalapril | 12 (9.2%) | 16 (14.8%) | 10 (9.9%) | 7 (7.6%) | 3 (18.7%) | 6 (42.8%) | 3 (25%) | 1 (9%) |
| Losartan | 18 (13.8%) | 16 (14.8%) | 16 (15.8%) | 12 (13.1%)j | 3 (18.7%) | 1 (7.1%) | 2 (16.6%) | 1 (9%) |
| Telmisartan | 6 (12.3%) | 8 (7.4%) | 8 (7.9%) | 8 (8.7%) | 0 | 0 | 1 (8.3%) | 1 (9%) |
| Frusemide | 9 (6.9%) | 11 (10.1%) | 3 (2.9%) | 0 | 4 (25%) | 3 (21.4%) | 1 (8.3%) | 0 |
f, g, hSignificant fall was seen in use of amlodipine from admission to discharge one month and six months (McNemar test: Discharge p=0.021, one month p=0.01. Six month p<0.0001); iUse of atenolol showed decreased use at six months compared to one month (p=0.043); jLosartan use showed a significant decreasing trend at six months (p=0.031)
p-value <0.05 was considered statistically significant
Use of antiepileptic (24 patients had seizures), lipid lowering, neuroprotective and edema agents as shown in [Table/Fig-12].
Antiepileptic, lipid lowering, neuroprotective and oedema agents.
| Therapies used | Ischaemic | Haemorrhagic |
|---|
| Admission (n=130) | Discharge (n=106) | Three months (n=111) | Six months (n=91) | Admission (n=16) | Discharge (n=14) | Three months (n=12) | Six months (n=11) |
|---|
| Antiepileptics |
| Phenytoin | 13 (10%) | 11 (10.3%)k | 7 (6.3%)l | 4 (4.3%)m | 15 (93.7%) | 11 (78.5%) | 10 (83.3%) | 7 (63.6%) |
| Gabapentine | 11 (8.4%) | 11 (10.3%) | 7 (6.3%) | 2 (2.1%) | 1 (6.2%) | 4 (28.5%) | 1 (8.3%) | 0 |
| Lipid lowering |
| Statins | 79 (60.7%) | 79 (74.5%) | 70 (63%) | 45 (49.4%) | 14 (87.5%) | 12 (85%) | 11 (91.6%) | 10 (90.9%) |
| Fenofibrate | 10 (7.6%) | 19 (17.9%) | 13 (11.7%) | 5 (5.4%) | 1 (6.2%) | 1 (7.1%) | 2 (5.4%) | 1 (9%) |
| Neuroprotective | 81 (62.3%) | 56 (52.8%) | 42 (37.8%) | 5 (5.4%) | 12 (75%) | 5 (35.7%) | 3 (8.1%) | 1 (9%) |
| Antiedema drug |
| Mannitol | 28 (21.5%) | - | - | - | 12 (75%) | - | - | - |
| Glycerol | 7 (5.3%) | - | - | - | 4 (25%) | - | - | - |
k, l, mPhenytoin (patients had seizures) use showed decreasing trend from admission to discharge which was significant (Discharge: p<0.0021, three months: p<0.0021, six months p=0.024); p-value <0.05 was considered statistically significant
Adverse effects: Of 155 patients, 36 had adverse effects (mild) such as pedal oedema in 28 patients due to amlodipine, vomiting and gastritis in six patients due to aspirin and dry cough in two patients due to enalapril.
A total of 28 deaths out of a 155 (18.06%) patients occurred in the study at six months. Twenty four (18.46%) patients out of 130 patients had ischaemic stroke and 4 (25%) patients out of 16 patients had haemorrhagic stroke. Eight (33.33%) of ischaemic and 2 (50%) of haemorrhagic stroke patient deaths occurred during hospital stay.
Discussion
The present prospective observational study was conducted at KIMS, Hubballi on 155 patients with a diagnosis of stroke.
Patient Characteristics
A ~56% patients in this study were aged 60 years or less and rests were aged more than 60 years. This is different from western countries (US) where majority of the strokes occur in older age group (>65 years) [14]. More males were admitted with strokes (70%) compared to females with a ratio of 2.3:1. Anand K et al., reported a male to female ratio of 1.71 [15]. A ~24% participants were employed in the public or private sector, 43% were self-employed and 33% were unemployed. Employment is an indicator of socioeconomic status unemployment was associated with a higher risk of adjusted in-hospital mortality [16].
Clinical Data
There were 83.87% patients of ischaemic stroke, 10.30% haemorrhagic stroke and 5.8% had a TIA. The Indian Collaborative Acute Stroke Study (ICASS) observed ischaemic stroke in 77%, haemorrhagic stroke in 22% and unspecified stroke in 1% cases based on cerebral computed tomography [17].
Time Delay in Presentation
The median time taken to reaching the tertiary care hospital from symptom onset around 11 hours for acute ischaemic stroke, around 6 hours for haemorrhagic stroke and around 13 hours for TIA. According to the study by Srivastava AK and Prasad K out of 110 cases, who were admitted within 72 hours, about 25% patients arrived within three hours, 49% within 6 hours and 87% within 24 hours. Stroke subtype was not found to have any significant relation [18].
Risk Factors
In this study, hypertension was more common among haemorrhagic stroke patients (87.85%) as compared to ischaemic stroke patient approx. 75%. Diabetics were more among ischaemic stroke patients (60%) compared to haemorrhagic stroke patients (30%). A around 72% of stroke patients had abnormal lipid profile. According to Sridharan SE et al., studies, hypertension was the most frequent and occurred in 450 (83.2%) patients. 70 of 261 male patients (26.8%) smoked tobacco. Half of the patients had diabetes mellitus and 26% had dyslipidemia [19].
Complications during Hospital Stay
In patients with TIA (9%), no complications were observed during hospital stay. Haemorrhagic stroke patients (87.5%) had more complications compared to patients with ischaemic stroke patients (43.8%). Pandian JD found high rates of complication in acute stroke. Limb weakness, stroke severity, length of hospital stay and anaemia were the factors associated with complications. Other complications such as urinary tract infection, chest infection, bedsores, other pain, and depression, can lead to poor outcome [20].
Treatment of Transient Ischaemic Attack (TIA)
This study data suggested that about 11.36% of the patients with stroke had a preceding TIA. The risk of stroke following TIA is 10-15% at 90 days. A follow-up shows decreased rate of use of antiplatelet and antihypertensive drugs. The likely reasons are cost of the treatment, complete recovery of the weakness and alternative therapy [21].
Treatment of Ischaemic Stroke
Thrombolytic therapy: In this study, only two patients received thrombolytic therapy. The important reason for patients not receiving thrombolysis include reaching beyond three hours of window period, non-affordability of treatment and caution of the treating physicians [22].
Antiplatelet therapy: A 93% patients with ischaemic stroke received antiplatelets. For first month, aspirin and clopidogrel were given, later, only aspirin was continued as it is cost-effective. The fall in the use of antiplatelet drugs in the study were patient related. Majority of patients stopped treatment due to unsatisfactory improvement in disease condition, adopting alternative therapy and 20 patients stopped because of complete recovery.
Antihypertensive drugs: Amlodipine 5 mg OD was the most commonly prescribed antihypertensive. The second most common drug group was ACE inhibitors (~23%). β blockers (9%) were used less often, which was in accordance with European Stroke Organisation guidelines [23]. Study recommends Enalapril because in this study 28 patients on amlodipine had pedal oedema.
Lipid lowering drugs: In this study, atorvastatin was the most commonly prescribed statin (~60%). Statins have an important role in secondary prevention of ischaemic stroke. In recently published meta-analysis a relative risk reduction of ~21% was estimated for every 1 mg/dL fall in the LDL cholesterol [24].
Treatment of haemorrhagic stroke: Here the mainstay of treatment is to control BP and reduce the cerebral edema. The most common drug used to control hypertension was amlodipine, with ~61% of patients on the drug and the second most common drug group was ACE inhibitors (~30%). A ~9% patients underwent decompressive surgery to release the intracranial tension. This intervention has proven beneficial in many randomised clinical trials [25].
Treatment outcome in the study: There was a significant improvement in all the surviving patients measured by modified Rankin score between admission and discharge and also at three and six months. Patients showed reduced compliance to all medications.
Mortality outcome in the study: A total of 28 deaths out of 155 (approx. 18%) patients occurred in the study at six months. A total of 24 (18.46%) out of ischaemic stroke patients and 4 (25%) out of haemorrhagic stroke patients. Of these, 8 (33%) ischaemic and 2 (50%) haemorrhagic stroke patients died during hospital stay. According to Suthar NN et al., mortality was higher when the size of block exceeded 30 cm3. Poor clinical outcome was associated with high Intracerebral Hemorrhage (ICH) score, low Glasgow Coma Scale (GCS) score at the time of admission, presence of intraventricular haemorrhage and midline shift [26].
Limitation(s)
This was a single institutional study.
Conclusion(s)
In this study, on stroke spanning one year, patients were elderly and males were twice affected as females. Urban patients were twice likely to go to hospital compared to rural patients. Patients reached hospital after variable intervals and this affected the outcome. Ischaemic stroke was approx four times more common than haemorrhagic stroke. Hypertension was more common in haemorrhagic stroke and diabetes in ischaemic stroke. Antihypertensive treatment was initiated in haemorrhagic stroke. Antiplatelet drugs and statins were prescribed in ischaemic stroke. There was a significant improvement in all the patients following treatment. However, patients showed reduced compliance to all medications.
Suggestions for improvement in outcome of stroke include improvement in emergency medical services, faster transportation of patients from remote areas, early recognition of symptoms of stroke, immediate CT/MRI imaging, early institution of treatment and secondary prevention of stroke by educating the patients regarding disease condition, prognosis and regular follow-up, adherence to treatment as recurrent stroke will have more severe morbidity and mortality. Multicentre, large scale, long term follow-up study is required for better analysis and management of stroke, in terms of treatment, education of patient and family members regarding the stroke.