The UGIT disorders are quite common in routine clinical practice and have high degree of morbidity and mortality [1]. The UGIT comprises of oral cavity, oesophagus, stomach and duodenum. Several lesions can affect the UGIT which are broadly classified into congenital anomalies, infections, inflammation, benign and malignant neoplasms [2]. To visualise and to get the specimen from the gastrointestinal tract a flexible, fiberoptic endoscopy is used. Endoscopic biopsy in combination with histopathological examination plays an important role in the early diagnosis of oesophago-gastro-duodenal lesions [3]. The flexible fiberoptic endoscope for upper GIT was introduced almost 50 years ago and was used for the first time in 1968. It facilitated the diagnosis of lesions in the oesophagus, stomach and duodenum [1]. Endoscopy provides the ease of direct visualisation of neoplastic and non-neoplastic lesions. By endoscopy a tissue sample from the lesion can be collected and studied by histopathology. This procedure has been well established over the years and is the gold standard to diagnose the nature of UGIT lesions [4]. Endoscopic biopsies are performed to diagnose a disease, to monitor the disease process, to assess the response to treatment and also to diagnose any complications at an earlier stage [5].
As there was no published literature from this area of Southern India, the present study reports the nature of UGIT lesions based on histopathology in our local rural population. The objectives were to look at the age and gender distribution, the sites and the types of lesions affecting the UGIT.
Materials and Methods
This was a prospective observational study conducted in the Department of Pathology at Pinnamaneni Siddhartha Institute of Medical Sciences and Research Foundation, Chinna Avutapalli, Andhra Pradesh, India. The study period was of one year from March 2019 to February 2020. The study had no ethical issues.
Inclusion Criteria
Age range from 20 years to 78 years,
Both genders,
All the upper gastrointestinal endoscopic biopsies, which included the lesions from oesophagus, stomach and upto second part of duodenum.
Exclusion Criteria
Age less than 20 years,
Lesions in the oral cavity and pharynx,
Lesions beyond the second part of duodenum.
Sample Collection
A total of 160 biopsy samples from the UGIT were collected by endoscopy and were received from Department of General Surgery. The biopsies were received in formalin containers along with the histopathology test requisitions. Demographic data such as age, gender, duration of symptoms of the patients were noted from the histopathology requisition forms. Other routine investigation results and radiological examination like x-ray and ultrasound reports wherever available were also recorded. All the upper GI endoscopic biopsies were fixed in 10% neutral buffered formalin for adequate time and were processed in automated tissue processor and embedded in paraffin with mucosal surfaces facing uppermost. Sections were cut at five micron thickness and were stained by Haematoxylin and Eosin (H&E). Special stains such as Giemsa, Warthin-Starry stains were also done whenever indicated. Immunohistochemistry studies were not done. The stained slides were examined and histomorphological patterns were studied. Tumours were diagnosed according to the recent WHO classification (2019) [6].
Statistical Analysis
For statistical analysis, the data was entered into excel sheets and percentages and ratios were calculated.
Results
A total of 160 biopsy samples were studied from Upper GIT i.e., from oesophagus, stomach and duodenum.
Distribution of cases based on the site: There were 50 (31.2%) cases from oesophageal lesions, 80 (50%) cases from stomach and 30 (18.7%) cases with duodenal lesions. Majority of UGIT endoscopic biopsies were obtained from stomach [Table/Fig-1].
Age, gender and site-wise distribution of biopsies. M: Male; F: Female.
| Oesophagus (50) | Stomach (80) | Duodenum (30) | Total |
|---|
| Age (years) | M | F | Total | M | F | Total | M | F | Total | M | F | Total |
|---|
| 20-30 | 01 | 01 | 02 | 07 | 06 | 13 | 03 | 02 | 05 | 11 | 9 | 20 |
| 31-40 | 23 | 05 | 28 | 24 | 12 | 36 | 04 | 03 | 07 | 51 | 20 | 71 |
| 41-50 | 04 | 06 | 10 | 10 | 11 | 21 | 11 | 04 | 15 | 25 | 21 | 46 |
| 51-60 | 02 | 01 | 03 | 03 | 01 | 04 | 02 | 01 | 03 | 7 | 3 | 10 |
| 61-70 | 04 | 01 | 05 | 05 | - | 05 | - | - | - | 9 | 1 | 10 |
| 71-80 | 01 | 01 | 02 | 01 | - | 01 | - | - | - | 2 | 1 | 3 |
| Total | 35 (70%) | 15 (30%) | 50 (100%) | 50 (62.5%) | 30 (37.5%) | 80 (100%) | 20 (66.6%) | 10 (33.3%) | 30 (100%) | 105 (65.6%) | 55 (34.3) | 160 (100%) |
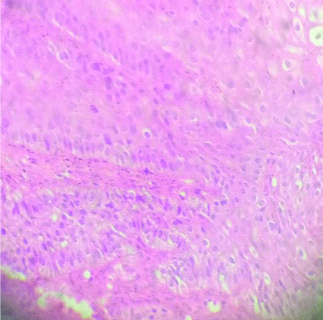
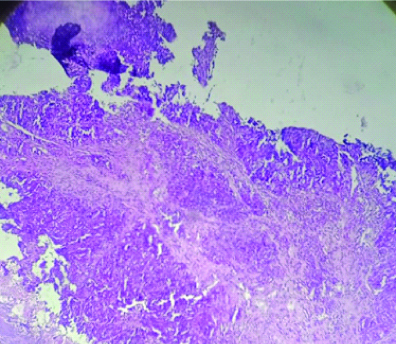
Non-neoplastic versus neoplastic lesions based on site: In the present study among oesophageal biopsies, 30 (60%) were non-neoplastic and 20 (40%) were neoplastic [Table/Fig-2]. There were also a few premalignant/dysplastic lesions in the oesophageal biopsies showing disordered arrangement of the epithelium and nuclear hyperchromasia with intact basement membrane [Table/Fig-3]. There were 4 (8%) cases of frank squamous cell carcinoma of the oesophagus with cellular features of malignancy and infiltration into the underlying stroma [Table/Fig-4]. Among gastric biopsies, 70 (87.5%) were non-neoplastic and 10 (12.5%) were neoplastic. Chronic non-specific gastritis was the most common finding in the non-neoplastic group and was seen in 38 (47.5%) cases [Table/Fig-5]. Among duodenal biopsies all 30 (100%) were non-neoplastic. Males were predominant i.e., 65.6% as compared to females i.e., 34.3% and the male to female ratio was 1.9:1 [Table/Fig-1].
Pattern of histopathological lesions and site of endoscopic biopsies in oesophagus.
| Oesophagus | Site | No. of cases |
|---|
| Non-neoplastic-(30/50) |
| Normal study | Upper 2/3rd | 06 (12%) |
| Chronic non-specific oesophagitis | Upper 1/3rd | 20 (40%) |
| Oesophageal ulcer | Upper 1/3rd | 04 (8%) |
| Neoplastic- (20/50) |
| Benign-06 |
| Squamous papilloma | Upper 1/3rd | 06 (12%) |
| Malignant and premalignant-14 |
| Low grade dysplasia | Middle 2/3rd | 05 (10%) |
| High grade dysplasia | Lower 1/3rd | 04 (8%) |
| Well-differentiated squamous cell carcinoma | Lower 2/3rd | 04 (8%) |
| Adenocarcinoma of oesophagus | Lower 1/3rd | 01 (2%) |
| Total | 50 (100%) |
Non-neoplastic lesions were more common than neoplastic lesions in oesophagus
Oesophageal dysplasia showing dysplastic squamous cells (H&E100X).
Squamous cell carcinoma of oesophagus showing infiltrating squamous cells (H&E 40X).
Pattern of histopathological lesions and site of endoscopic biopsies in stomach.
| Stomach | Site | No. of cases |
|---|
| Non-neoplastic (70) |
| Acute gastric ulcer | Pylorus | 07 (8.7%) |
| Chronic peptic ulcer | Pylorus | 15 (18.7%) |
| Chronic non-specific antral gastritis | Antrum | 38 (47.5%) |
| Chronic atrophic gastritis | Pylorus | 02 (2.5%) |
| Hyperplastic polyp | Pylorus | 08 (10%) |
| Neoplastic (10) |
| Gastric adenocarcinoma | Pylorus | 04 (5%) |
| Signet ring cell adenocarcinoma | Antrum | 06 (7.5%) |
| Total | | 80 (100%) |
Non-neoplastic lesions were more common than neoplastic lesions in stomach
The oesophageal and gastric biopsies were most frequently received from the patients in 3rd decade and biopsies from both locations were common in males as compared to females. Duodenal biopsies were most frequently received from the patients in 4th decade and here also males were predominant as compared to females. Among non-neoplastic lesions chronic non-specific antral gastritis was the most common of all. Among malignancy all 10 cases were seen in antrum and pylorus region of stomach. All the patients with malignant lesions had presented with the complaints of pain in abdomen and loss of appetite.
Pattern of histopathological lesions and site of endoscopic biopsies in duodenum: There were 20 (66.6%) cases of chronic non-specific duodenitis and 10 (33.3%) cases of duodenal ulcer. All the 30 cases had sampling from the first part of duodenum. There were no cases of duodenal neoplasia.
Discussion
Lesions of UGIT are commonly encountered in clinical practice and if they are severe, recurrent or chronic then often they are subjected to endoscopy followed by biopsy. The most common indications for UGIT endoscopy are dyspepsia, dysphagia and odynophagia, Gastroesophageal Reflux Disease (GERD), nausea and vomiting that is persistent, occult gastrointestinal bleeding, and surveillance for malignancy. Upper GI endoscopy is very useful for removal of foreign body and is also indicated for stricture dilatation [7]. In the present study, an attempt was done to evaluate the type of lesions of UGIT in our local population. In the present study, a total of 160 endoscopic biopsies from UGIT were examined histopathologically. Krishnappa R et al., studied 100 cases of upper GI endoscopic biopsies [8]. In their study the male to female ratio was 2.03:1 and more number of cases was seen in the fourth and fifth decades.
In the Bhat N et al., study, 200 cases were studied with a wide range of patient age from 16 years to 95 years and the mean age was 56.63 years [9]. In a similar study by Rani D et al., histopathological examination was done in 100 endoscopic biopsies from the UGIT lesions [10]. In a study by Bhargavi M et al., study a total of 106 cases were studied [11]. In a study by Theresa JM et al., 152 cases of upper gastrointestinal lesions were studied [12]. In the present study, maximum number of cases was among 31-40 years and 41-50 years. The youngest patient in present study was 20-year-old, while the oldest was 78 years [Table/Fig-1]. Rani D et al., in their study observed the youngest patient to be 21-year-old, while the oldest one was of 80 years [10]. Maximum number of cases was in 5th to 7th decades of life in their study. In the Duraisamy PR et al., study, the age range was from 23 years to 90 years with a mean of 57 years [13]. In the Theresa JM et al., study, the commonly affected age group was 31-40 years followed by 41 to 50 years [12]. The youngest age included in the study was 16 years and the eldest age was 72 years.
In present study, there was a slight male preponderance and the male to female ratio was 1.9:1 [Table/Fig-1]. In the Rani D et al., study, there were 61 males and 39 females and the male to female ratio was 1.5:1 [10]. In the Duraisamy PR et al., study, there were 132 males and 64 female patients and the male to female ratio was 2:1 [13]. In the Bhat N et al., and Theresa JM et al., studies, there were 120 (63.54%) males and 80 (36.46%) females, the male:female ratio being 1.5:1 and 87 males and 65 females with a male to female ratio of 1.3:1, respectively [9,12].
In present study, out of 100 cases, 31.2% (50/160) of the biopsies were from the oesophagus, 50% (80/160) were from the stomach and 18.7% (30/160) were from the duodenum [Table/Fig-1]. Bhat N et al., reported the site-wise distribution of endoscopic biopsies as gastric 110 (55%), oesophagus 48 (24%), gastro-oesophageal junction as 22 (11%) and duodenum 20 (10%) [9]. Rani D et al., in their study reported 30% of the biopsies from oesophagus, 46% from stomach and 24% were from duodenum [10]. Bhargavi M et al., observed 60% biopsies from stomach followed by oesophagus (23%) and duodenum (17%) [11]. Theresa JM et al., reported 74% biopsies was from stomach, 15% from oesophagus, and the remaining 1% biopsies from duodenum [12]. Present study observations for the site wise distribution of lesions in UGIT compare well with the observations of above authors. In present study, the non-neoplastic pathologies predominated over neoplastic pathologies in all upper GI sites. Most of the studies have observed predominance of non-neoplastic lesions in upper GIT [Table/Fig-6] [8-12]. Bhargavi M et al., reported squamous cell carcinoma as the most common malignancy in the middle third of the oesophagus [11]. The incidence of oesophageal carcinoma was higher in the study by Bhat N et al., [Table/Fig-7] [9]. It could be due to the geographical region, environmental factors or due to the practice of consuming salted tea with sodium bicarbonate that is common in this region.
Comparative studies of endoscopic lesions [8-12].
| Comparative studies | Oesophagus | Stomach | Duodenum |
|---|
| Non-neoplastic | Neoplastic | Non-neoplastic | Neoplastic | Non-neoplastic | Neoplastic |
|---|
| Krishnappa R et al., (2013) [8] | 14 (56%) | 11 (44%) | 41 (60%) | 27 (40%) | 5 (71%) | 2 (28.5%) |
| Bhat N et al., (2018) [9] | 36 (75%) | 12 (25%) | 76 (69.09%) | 34 (30.90%) | 14 (70%) | 06 (30%) |
| Rani D et al., (2019) [10] | 02 (6.7%) | 28 (93.3%) | 32 (69.6%) | 14 (30.4%) | 20 (83.3%) | 04 (16.7%) |
| Bhargavi M et al., (2019) [11] | 07 (29.2%) | 17 (70.8%) | 28 (43.7%) | 36 (56.3%) | 16 (88.9%) | 02 (11.1%) |
| Theresa JM et al., (2020) [12] | 16 (72.7%) | 06 (27.2%) | 104 (92%) | 9 (7.96%) | 17 (100%) | Nil |
| Present study (2020) | 30 (60%) | 20 (40%) | 70 (87.5%) | 10 (12.5%) | 30 (100%) | Nil |
Comparative studies of endoscopic oesophageal biopsies [9,10].
| Oesophageal biopsies | Bhat N et al., (2018) [9] | Rani D et al., (2019) [10] | Present study (2020) |
|---|
| Reflux oesophagitis | - | 02 (6.7%) | - |
| Chronic non-specific oesophagitis | 3 (6.25%) | - | 20 (40%) |
| Oesophageal dysplasia | 2 (4.16%) | - | 09 (18%) |
| Hyperplastic polyp | 2 (4.16%) | - | - |
| Squamous papilloma | 1 (2.08%) | 3.3% | 06 (12%) |
| Well-differentiated squamous cell carcinoma | 7 (20%) | 06 (20%) | 04 (8%) |
| Moderately differentiated squamous cell carcinoma | 23 (65.71%) | 12 (40%) | - |
| Poorly differentiated squamous cell carcinoma | 05 (14.28%) | 06 (13.3%) | - |
| Adenocarcinoma | - | 05 (16.7%) | - |
| Non-specific pathology | 03 | - | - |
In the study, by Theresa JM et al., common non-neoplastic lesion among the oesophageal biopsies were chronic non-specific oesophagitis [12], followed by oesophageal ulcer. The common neoplastic lesion observed was squamous cell carcinoma and there were three cases of Barret’s oesophagus. Barrett’s oesophagus is worrisome because it predisposes to adenocarcinoma of oesophagus and has 20 times increased risk [14]. One of the advantages of endoscopic biopsy is that it can pick up premalignant lesions. In present study, 9 (18%) cases of oesophageal dysplasia were detected [Table/Fig-2]. This helps the clinician for further patient management and surveillance. Multiple biopsies (≥8) from the base and edges of gastric ulcers are recommended if there is suspicion of malignancy or if the endoscopy is suggestive of malignancy [15]. Exfoliative cytology can also be performed and is complementary to biopsy [16]. Diffuse gastric adenocarcinoma is not so common but even when it is present, the mucosa may appear unremarkable. In such cases, there is low distensibility and with appropriate clinical context it should prompt multiple biopsies [15]. Chronic non-specific gastritis is a most common pathology in the stomach. In the present study, there were 47.5% cases of chronic non-specific gastritis [Table/Fig-5]. Bhat N et al., and Bhargavi M et al., observed similar incidence of 43.6% and 42.9% cases in their studies, respectively [Table/Fig-8] [9,11].
Comparative studies of endoscopic gastric biopsies [9-11].
| Endoscopic gastric biopsies | Bhat N et al., (2018) [9] | Rani Det al., (2019) [10] | Bhargavi M et al., (2019) [11] | Present study (2020) |
|---|
| Gastric ulcer | - | 04 (8.8%) | - | 22 (27.5%) |
| Hyperplastic polyp | 14 (12.72%) | 04 (8.8%) | - | 08 (10%) |
| H. pylori gastritis | 26 (54.16%) | 19.5% | 42.9% | - |
| Chronic non-specific gastritis | 48 (43.63%) | 15% | 38 (47.5%) |
| Chronic atrophic gastritis | - | - | - | 02 (2.5%) |
| Fundic gland polyp | | 17.5% | | - |
| Adenocarcinoma/Signet ring cell carcinoma | 28 (25.45%) | 15% | 34 (94.4%) | 10 (12.5%) |
| Tubular adenocarcinoma | - | 11% | - | - |
| Papillary adenocarcinoma | - | 01 (2.2%) | - | - |
| Diffuse Large B Cell Lymphoma (DLBCL) | - | 01 (2.2%) | - | - |
| Others | 1 (0.90%) | - | - | - |
Suspected celiac disease is a very common indication for duodenal biopsy. As the histological changes may be patchy in distribution, four to six biopsies of the duodenal bulb and distal duodenum are recommended. Whenever celiac disease is not suspected but still if any minor abnormalities of the duodenal mucosa are seen, then biopsies are not indicated [16]. In our study, the most common histopathological diagnosis for duodenal biopsies was non-specific duodenitis. Bhat N et al., reported lower incidence (30%) in their study material [9]. No duodenal malignancies was observed in present study. Similar findings were reported by above authors [Table/Fig-9]. The lower GIT has more of non-neoplastic lesions as compared to neoplastic lesions with non-specific colitis being the most common lesion [17]. A similar trend is seen in the upper GI tract also with predominance of non-specific inflammation. Sometimes limitations of histopathological examination are seen like very tiny tissue samples, fragmented biopsy material, pinching artefacts and processing artefacts. Multiple tissue bits and adequate biopsy material taken from representative areas can overcome these limitations.
Comparative studies of endoscopic duodenal biopsies [8-12].
| Duodenal biopsies | Krishnappa R et al., (2013) [8] | Bhat N et al., (2018) [9] | Rani D et al., (2019) [10] | Bhargai M et al., (2019) [11] | Theresa JM et al., (2020) [12] | Present study (2020) |
|---|
| Celiac disease | - | 3 (15%) | 14 (58.5%) | - | - | - |
| Non-specific duodenitis | 4 (57%) | 6 (30%) | 03 (12.5%) | 16 | 17 | 20 (66.6%) |
| Duodenal ulcer | 1 (14%) | 2 (10%) | - | - | - | 10 (33.3%) |
| Adenocarcinoma | 1 (14%) | 2 (10%) | 03 (12.5%) | 01 | - | - |
| Tubular adenoma | 1 (14%) | 3 (15%) | | - | - | - |
| Normal histology | - | 3 (15%) | 02 (8.3%) | 01 | - | - |
| Giardiasis | - | | 01 (4.1%) | - | - | - |
| Lowgrade neuroendocrine tumour G1 (carcinoid) | - | 1 (5%) | 01 (4.1%) | 01 | - | - |
Limitation(s)
This was only an observational study with limited sample size. Some of the patients had undergone previous biopsy (at outside hospitals) but the reports were not available to compare evolution of the lesions. Also, immunohistochemistry and molecular studies could not be done. Larger and further studies are needed to evaluate the predisposing risk factors for upper GIT lesions.
Conclusion(s)
UGIT lesions are more common in adults in the fourth and fifth decades and are more common in males as compared to females. Non-neoplastic conditions predominate over neoplastic conditions. The antrum and pylorus are favoured sites for gastric malignancy. Malignant lesions are very rare in duodenum. Further large scale studies are recommended to search for environmental causes that give rise to upper GI pathologies. Further studies incorporating genetic and molecular testing are recommended to better understand the molecular mechanisms of upper GI malignancies.
Non-neoplastic lesions were more common than neoplastic lesions in oesophagus
Non-neoplastic lesions were more common than neoplastic lesions in stomach