A Curious Case of Acute Pancreatitis in Pregnancy
Karan Rajgopal Kalani1, Vaishali Kathuria2, Sanjay Pandit3, Dharam Pal Bhadoria4
1 Postgraduate, Department of Medicine, Maulana Azad Medical College, Delhi, India.
2 Postgraduate, Department of Medicine, Maulana Azad Medical College, Delhi, India.
3 Professor, Department of Medicine, Maulana Azad Medical College, Delhi, India.
4 Director Professor, Department of Medicine, Maulana Azad Medical College, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dharam Pal Bhadoria, Room No. 114, Old Resident Doctors Hostel, Lok Nayak Hospital, Delhi-110002, India.
E-mail: kalani.karan1993@gmail.com
Hypercalcaemia is rare in pregnancy and is under diagnosed owing to its non-specific presentation which is frequently attributed to the pregnancy itself. Severe hypercalcaemia presents a therapeutic challenge, especially during pregnancy. The present case of a 26-year-old primigravida who presented with acute pancreatitis is described here. The pancreatitis was found to be secondary to parathyroid adenoma- induced hypercalcaemia. After initial conservative medical management with subcutaneous and intranasal calcitonin, she underwent a small-incision adenoma excision. This unusual cause and presentation of hypercalcaemia and its management is reviewed thereof.
Bisphosphonates, Calcitonin, Cinacalcet, Hypercalcaemia, Parathyroid adenoma, Primary hyperparathyroidism
Case Report
A 26-year-old primigravida, who was recently diagnosed to be hypothyroid, presented to the Medicine Department of our hospital in the 14th week of her pregnancy with complains of abdominal pain which was aggravated by meals and vomiting for the last four days. Past history was significant for nephrolithiasis four years back which was managed conservatively. Her medications included tablet Levothyroxine 12.5 mcg for Hypothyroidism diagnosed two months ago. On examination, her blood pressure was 96/70 mm Hg with a heart rate of 102 beats per minute. Temperature was 100.1°F with a respiratory rate of 20 breaths per minute. She had epigastric tenderness on gentle palpation. All other examination findings were normal.
[Table/Fig-1] shows relevant laboratory investigations at presentation and during further stay. An ultrasonogram of the abdomen showed a bulky pancreas suggestive of acute pancreatitis. It also confirmed a foetus appropriate for gestational age with normal cardiac activity. The pancreatitis was classified as mild as per Revised Atlanta scoring [1]. A 25-Hydroxy Vitamin D levels were borderline low (29 ng/mL) while the 24-hour urinary calcium levels were in the normal range (148 mg/day).
Showing laboratory investigation.
| Investigations | Day 1 | Day 8 | Day 15 (Discharge) |
|---|
| Haemoglobin (g/dL) | 9.2 | 9.1 | 9.5 |
| Leukocyte count (/cu.mm) | 7800 | 8400 | 6900 |
| Serum creatinine (mg/dL) | 0.9 | 0.7 | 0.7 |
| Serum amylase (mg/dL) | 431 | 126 | 74 |
| Serum lipase (mg/dL) | 501 | 240 | 45 |
| Serum calcium (mg/dL) | 14 | 12.9 | 9 |
| Serum PTH (pg/mL) | 114.3 | - | 20 |
| Random blood sugar (mg/dL) | 112 | - | 82 |
g/dL: Grams/deciliter, cu.mm: Cubic millimeters, mg/dL: Milligrams/deciliter, pg/mL: Picograms/milliliter, PTH: Parathyroid hormone
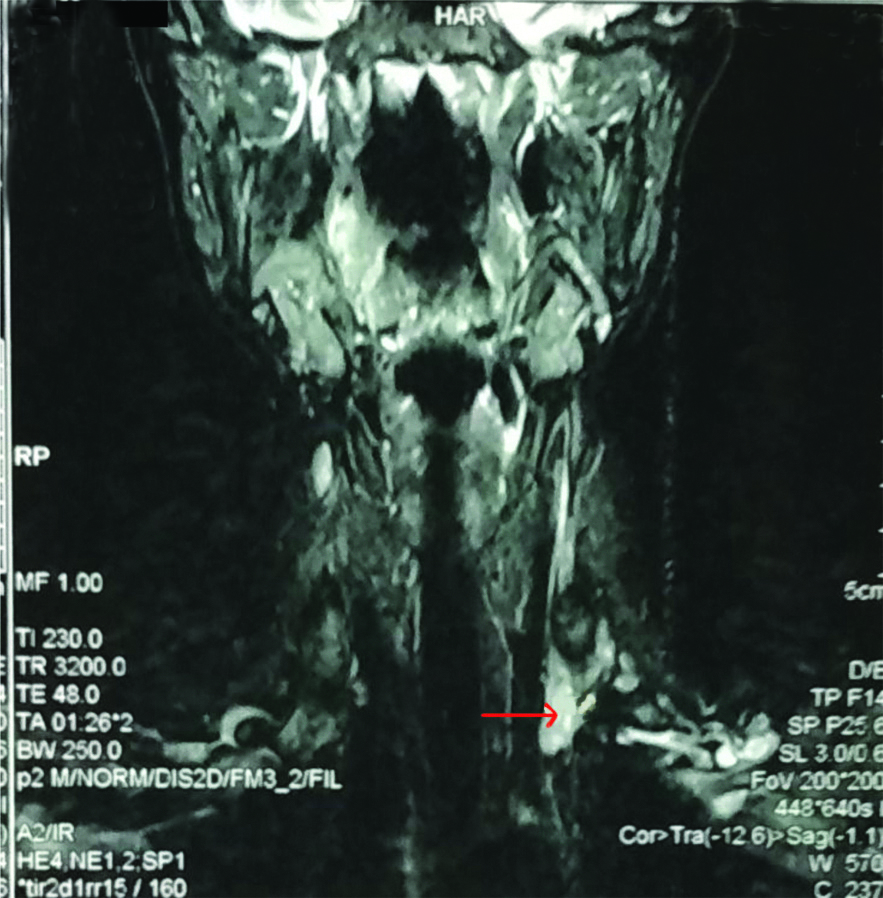
Subsequently, an ultrasonography of the neck was done which revealed a hypoechoic lesion in the inferior aspect of the left side of the thyroid in the tracheo-esophageal groove measuring 6×5.5×24 mm with significant internal vascularity, likely suggestive of a Parathyroid adenoma. The Magnetic Resonance Imaging (MRI) of the Neck corroborated these findings [Table/Fig-2]. Other differential on imaging was thyroid nodule which did not correspond with the clinical picture.
MRI of the neck revealing a soft tissue lesion in the lower pole of the left thyroid (red arrow) likely suggestive of a parathyroid adenoma.
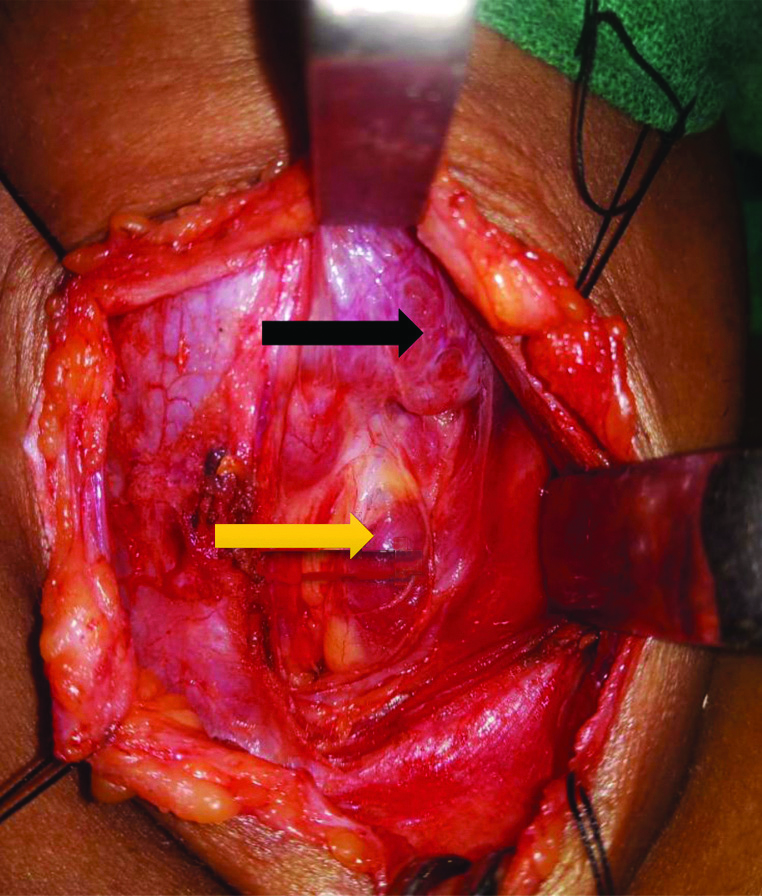
Meanwhile, the hypercalcaemia was managed with normal saline and intravenous torsemide at 20 mg/day. Subcutaneous Calcitonin was given 12 hourly for two days for a cumulative dose of 1000 IU. Serum calcium levels were monitored daily, and showed response to the above therapy (corrected serum calcium 10.9 mg/dL on day 4 of admission). The response, however, was temporary and the calcium levels began to rise again (corrected calcium 14.3 mg/dL on day 7 of admission). In view of persistent hypercalcaemia, surgical management was planned in consultation with the Otorhinolaryngology Department. For two days preoperatively, she was given intranasal calcitonin (one puff of 200 IU/day in alternate nostrils). She underwent an uneventful small-incision parathyroid excision of the adenoma under general anaesthesia [Table/Fig-3,4]. Intraoperative and postoperative Parathyroid Hormone (PTH) levels were 19 pg/mL and 20 pg/mL, respectively, thus fulfilling the Miami criteria (50% decline from the highest pre-excision PTH level obtained 10 minutes after excision of the hypersecreting parathyroid gland).
Intraoperative picture showing a normal thyroid gland (black arrow) and the parathyroid adenoma (yellow arrow).
Showing the excised adenoma.

There were no foetal or maternal complications during or post-surgery. The patient underwent an uneventful recovery. Postoperative corrected serum calcium levels were 9 mg/dL. Patient was discharged on calcium and vitamin D supplements. She had an uneventful antenatal course beyond this point. She underwent a full term, normal vaginal delivery six months later and delivered a healthy baby with normal neonatal calcium levels. Patient is currently on routine calcium supplementation with normal calcium levels.
Discussion
Pregnancy associated pancreatitis is rare, with a recent study showing a prevalence of 0.001%, with gallstones accounting for more than 70% of cases [2]. Hyperparathyroidism was seen in only 1 (3%) of these cases. The incidence increases with gestational age. Ultrasound remains the diagnostic modality of choice owing to its safety and sensitivity. In a previous retrospective study involving 101 patients, there were no maternal mortalities whereas the perinatal mortality rate was 3.6% [3]. First trimester patients tend to have a higher risk of foetal loss, preterm delivery and a lower chance of attaining term pregnancy [4]. The aetiological profile and management remain fairly similar to non-pregnant female patients. This includes fasting, hydration, analgesics and nutritional support. Role of prophylactic antibiotics is limited to severe acute pancreatitis and necrotising pancreatitis [5]. However, biliary pancreatitis has a higher recurrence rate in pregnancy than in the general population, and may necessitate early surgery [6].
Normal calcium metabolism undergoes the following changes in pregnancy [Table/Fig-5] [7].
Physiological changes in calcium metabolism during pregnancy.
| Variable | Physiological changes |
|---|
| Total serum calcium | Decreased |
| Serum ionised calcium | Unchanged |
| Urinary calcium | Increased |
| Serum PTH | Unchanged (maybe decreased in the third trimester) |
| PTHrP | Progressively increases |
| 25-Vitamin D | Unchanged |
| 1,25-Dihydroxyvitamin D | Progressively increases upto 100% |
| Intestinal absorption of calcium | Increases by 100% |
| 1-Alpha hydroxylase activity | Increased |
| Calcitonin | Increases by 20% |
PTH: Parathyroid hormone; PTHrP: PTH related peptide
Hypercalcaemia is uncommon in pregnancy, occurring in about 0.03% of pregnancies [8]. Maternal symptoms and complications may include: fatigue, nausea, vomiting, confusion, constipation, hypertension, pancreatitis, recurrent miscarriages, nephrolithiasis, renal insufficiency among others. Foetal complications include intrauterine growth retardation, early or late demise, neonatal death, neonatal hypocalcaemia with tetany and permanent hypoparathyroidism. Among these, index patient manifested nausea, vomiting, pancreatitis, nephrolithiasis without any foetal complications. The diagnostic approach to hypercalcaemia in pregnancy remains essentially the same as a non-pregnant female. Rise in PTH levels with normal urinary calcium excretion points to hyperparathyroidism as the primary cause. Primary Hyperparathyroidism (PHPT) is the most common cause of hypercalcaemia in pregnancy, albeit very rare in itself with a reported incidence of 1% [9]. The most common cause is a single parathyroid adenoma. Other causes include humoral hypercalcaemia of malignancy, familial hypocalciuric hypercalcaemia, vitamin D intoxication, acute or chronic renal failure, granulomatous diseases, hyperthyroidism. Of note, excessive production of PTH related peptide (PTHrP) secondary to malignancies, benign tumours and placental excretion may also cause hypercalcaemia [10]. Thus, if no significant changes are seen in the PTH levels, PTHrP measurement is warranted.
Nuclear scintigraphy of the parathyroid via sestamibi scanning is contraindicated in pregnancy. Although ultrasonography has been reported to have varying degrees of sensitivity, it remains the modality of choice for imaging of the parathyroid [11]. Most of the non-pharmacological and pharmacological modalities for treatment of hypercalcaemia in non-pregnant females apply to pregnancy as well. However, there is concern regarding safety of certain drugs. Cinacalcet is a calcimimetic agent which activates the Calcium Sensing Receptor (CaSR) and decreases PTH levels. Its use in pregnancy has been reported in only a few cases, albeit with good results. One case reported a woman with metastatic parathyroid carcinoma who used it in the second and third trimester in one pregnancy and throughout a second pregnancy [12]. Calcitonin results in a modest calcium decrease. It may act as a bridging therapy to parathyroidectomy when rapid fall in calcium is required but its use is limited due to tachyphylaxis. Bisphosphonates cross the placenta and are retained in the skeleton for a long period. Indeed, a study among pregnant patients with autoimmune diseases exposed to bisphosphonates observed a 20% rate of congenital malformations [13].
Excision of the adenoma via small-incision parathyroid excision remains the modality of choice. Owing to the teratogenicity risks in the first trimester and the risk of preterm delivery in the third, surgery is preferred during the 2nd trimester [9,14]. One of the largest studies on PHPT in pregnancy included 109 patients and found reduced foetal complications with parathyroidectomy [15]. Multiple case reports have also documented the safety of surgery during the 3rd trimester [16].
Conclusion(s)
Hypercalcaemia in pregnancy can cause serious maternal, foetal, and neonatal complications. Early detection and diagnosis is a key for preventing complications. Mild, asymptomatic hypercalcaemia may be managed conservatively, albeit with close monitoring. However, for moderate to severe hypercalcaemia or symptoms, surgery is the modality of choice. When surgery is relatively contraindicated or difficult, it may be necessary to consider therapies not thoroughly studied during pregnancy.
g/dL: Grams/deciliter, cu.mm: Cubic millimeters, mg/dL: Milligrams/deciliter, pg/mL: Picograms/milliliter, PTH: Parathyroid hormone
PTH: Parathyroid hormone; PTHrP: PTH related peptide
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 04, 2020
Manual Googling: Oct 12, 2020
iThenticate Software: Nov 17, 2020 (5%)
[1]. Foster BR, Jensen KK, Bakis G, Shaaban AM, Coakley FV, Revised atlanta classification for acute pancreatitis: A pictorial essayRadioGraphics 2016 36(3):675-87.10.1148/rg.201615009727163588 [Google Scholar] [CrossRef] [PubMed]
[2]. Igbinosa O, Poddar S, Pitchumoni C, Pregnancy associated pancreatitis revisitedClinics and Research in Hepatology and Gastroenterology 2013 37(2):177-81.10.1016/j.clinre.2012.07.01122959401 [Google Scholar] [CrossRef] [PubMed]
[3]. Eddy JJ, Gideonsen MD, Song JY, Grobman WA, O’Halloran P, Pancreatitis in pregnancyObstet Gynecol 2008 112(5):1075-81.10.1097/AOG.0b013e318185a03218978108 [Google Scholar] [CrossRef] [PubMed]
[4]. Tang SJ, Rodriguez-Frias E, Singh S, Mayo MJ, Jazrawi SF, Sreenarasimhaiah J, Acute pancreatitis during pregnancyClin Gastroenterol Hepatol 2010 8(1):85-90.10.1016/j.cgh.2009.08.03519747985 [Google Scholar] [CrossRef] [PubMed]
[5]. Lim CL, Lee W, Liew YX, Tang SS, Chlebicki MP, Kwa AL, Role of antibiotic prophylaxis in necrotising pancreatitis: A meta-analysisJ Gastrointest Surg 2015 19(3):480-91.10.1007/s11605-014-2662-625608671 [Google Scholar] [CrossRef] [PubMed]
[6]. Ducarme G, Maire F, Chatel P, Luton D, Hammel P, Acute pancreatitis during pregnancy: A reviewJ Perinatol 2014 34(2):87-94.10.1038/jp.2013.16124355941 [Google Scholar] [CrossRef] [PubMed]
[7]. Kovacs CS, Calcium and bone metabolism in pregnancy and lactationJ Clin Endocrinol Metab 2001 86(6):2344-48.10.1210/jcem.86.6.757511397820 [Google Scholar] [CrossRef] [PubMed]
[8]. Hirsch D, Kopel V, Nadler V, Levy S, Toledano Y, Tsvetov G, Pregnancy outcomes in women with primary hyperparathyroidismJ Clin Endocrinol Metab 2015 100(5):2115-22.10.1210/jc.2015-111025751112 [Google Scholar] [CrossRef] [PubMed]
[9]. McCarthy A, Howarth S, Khoo S, Hale J, Oddy S, Halsall D, Management of primary hyperparathyroidism in pregnancy: A case seriesEndocrinology, Diabetes & Metabolism Case Reports 2019 2019(1):19-0039.10.1530/EDM-19-003931096181 [Google Scholar] [CrossRef] [PubMed]
[10]. Rey E, Jacob CE, Koolian M, Morin F, Hypercalcaemia in pregnancy- A multifaceted challenge: Case reports and literature reviewClin Case Rep 2016 4(10):1001-08.10.1002/ccr3.64627761256 [Google Scholar] [CrossRef] [PubMed]
[11]. Ginhoven TM van, Morks AN, Schepers T, Graaf PW de, Smit PC, Surgeon-performed ultrasound as preoperative localization study in patients with primary hyperparathyroidismEur Surg Res 2011 47(2):70-74.10.1159/00032796921701177 [Google Scholar] [CrossRef] [PubMed]
[12]. Nadarasa K, Bailey M, Chahal H, Raja O, Bhat R, Gayle C, The use of cinacalcet in pregnancy to treat a complex case of parathyroid carcinomaEndocrinology, Diabetes & Metabolism Case Reports 2014 2014:14005610.1530/EDM-14-005625298882 [Google Scholar] [CrossRef] [PubMed]
[13]. Losada I, Sartori L, Di Gianantonio E, Zen M, Clementi M, Doria A, Bisphosphonates in patients with autoimmune rheumatic diseases: Can they be used in women of childbearing age?Autoimmun Rev 2010 9(8):547-52.10.1016/j.autrev.2010.03.00220307690 [Google Scholar] [CrossRef] [PubMed]
[14]. Aggarwal A, Wadhwa R, Aggarwal V, Pande A, Singh SK, Gahlot A, Primary hyperparathyroidism in pregnancy: A multicenter case series of 4 patients from Northern IndiaJ Obstet Gynaecol India 2019 69(Suppl 1):31-35.10.1007/s13224-018-1148-y30956488 [Google Scholar] [CrossRef] [PubMed]
[15]. Kelly TR, Primary hyperparathyroidism during pregnancySurgery 1991 110(6):1028-33.discussion 1033-4 [Google Scholar]
[16]. Schnatz PF, Thaxton S, Parathyroidectomy in the third trimester of pregnancyObstet Gynecol Surv 2005 60(10):672-82.10.1097/01.ogx.0000180889.23678.fb16186784 [Google Scholar] [CrossRef] [PubMed]