Dentinal Hypersenstivity (DH) is a common dental problem which presents as a short, sharp, intense pain emanating from exposed dentinal tubules. This occurs due to response to stimuli which can be thermomechanical or chemical and is not attributable to any odontologic defect or pathology [1]. DH is closely related to exposed dentinal tubules [2]. The buccal surface of teeth is more commonly involved. DH often occurs in the maxillary canine and premolar teeth followed by incisors and molars [3-5]. Maxillary Canine and Premolar teeth are present at the corner of the mouth so they are more susceptible to abrasion due to tooth brushing and are prone to gingival recession and tooth defects [6]. Teeth with loss of gingiva, oral parafunctional habits, irregular teeth, poor oral hygiene, tooth brushing and erosion, occlusal problem, chronic periodontal diseases, age or a combination of these factors have increased frequency of DH [7]. A previous study described erosion as a major aetiological factor for DH [8]. Prevalence of DH ranges from 72.5% to 98% in patients suffering from periodontal diseases [9]. Patients with DH are more likely to be young with major aetiological factors associated as aggressive tooth brushing habit (15.1%), at home tooth whitening (16.6%), in-office tooth whitening (16.3%), gingival recession (17.1%) and occlusal trauma (11.1%). [10].
DH should be distinguished from other tooth sensitivity conditions like dental caries, traumatised tooth or fractured restoration [11]. The aetiology and mechanisms underlying the development of DH have not yet been well-explained, although many theories have been proposed for explaining generation of pain [12]. The transmission of stimuli from exposed dentin to the nerve endings may develop by means of the odontoblastic processes or through a hydrodynamic mechanism, the latter being considered the most plausible [13]. Brannstorm proposed the most accepted hydrodynamic theory [14]. This theory is based on the movement of fluid inside the dentinal tubule [15]. Sensitivity is further due to the thermal and physical changes as a result of formation of osmotic stimuli near the exposed dentin. Baroreceptors are stimulated by movement of fluid and leads to neural discharge [16,17]. Hydrodynamic process has been suggested to activate the Type A delta fibers responsible for dentinal sensitivity [18].
Laser is also a treatment option to reduce dentinal pain. In the last 15 years, dental lasers have shown to provide better results in cases of DH [21]. Diode, He-Ne are classified as low output lasers and Nd:YAG, CO2 are middle output lasers. All of them have been used for hypersensitivity treatment [22]. Low level lasers are known to possess anti-inflammatory properties [23]. Many clinical studies have reported the effectiveness of different wavelength diode lasers in cases of dentine hypersensitivity but the role of an innovative 980 nm Diode Laser with endodontic applications, compact size and versatility introduced in 2004 remains unclear and requires further studies. [18,24-26]. Although, the role of Nd:YAG, Er:YAg and 830 nm Diode Laser in treating DH has been proven in literature [26].
Thus, the quest to find out the ideal treatment for DH still remains as an enigma despite advances in Laser Dentistry and availability of newer generations of dentin bonding agents. Theoretically the most effective treatment for DH would be the one with long lasting prolonged effects, resistance to oral environment, have immediate postoperative results and comfort to the patient [27]. There is a paucity of comparative studies on evaluation of the effectiveness of HEMA based DA with 980 nm Diode Laser in treatment of DH could be found [28]. Thus, considering the lack of literature on the aforesaid subject this study was undertaken with an aim to evaluate the efficacy of HEMA based DA and 980 nm diode dental laser in treatment of DH.
Materials and Methods
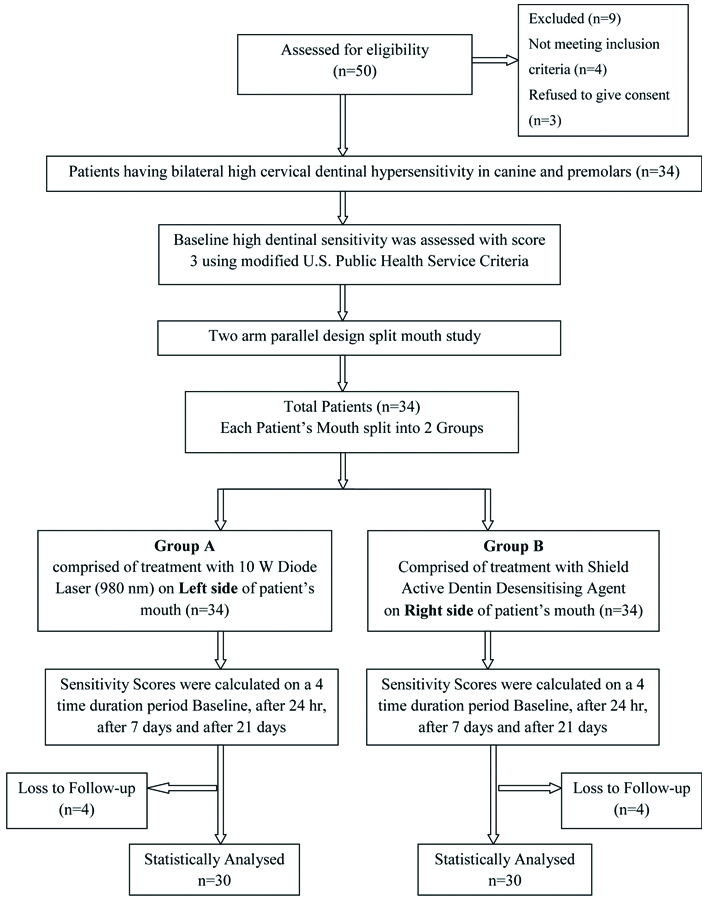
This was a two-arm parallel design split-mouth study conducted on 34 patients between the age group of 18 to 75 years attending the Dental Outpatient Clinic of Gandhi Medical College, Bhopal during the year December 2018 to January 2020. The ethical approval was obtained from the Institutional Ethical Committee (vide Letter No.38153-55/MC/IEC/2018 Bhopal Dated 11/12/2018) of Gandhi Medical College, Bhopal, Madhya Pradesh (MP) affiliated to MP State Medical State University, Jabalpur, M.P., India before commencement of the study. Study participants with bilateral maxillary canine pretreatment baseline sensitivity score Charlie=3 (High Sensitivity) were included in the study. Dentinal Hypersenstivity was assessed using Modified US Public Health Service Criteria for DH Assessment [29,30]. These criteria are a three-score system comprising of Alpha=0 (Absence of sensitivity to thermal and tactile stimuli), Bravo=2 (slight sensitivity to thermal and tactile stimuli) and Charlie=3 (high sensitivity to thermal and tactile stimuli). Teeth with caries, fracture, defective restoration, periodontal pockets, tooth mobility, having prosthodontic or orthodontic appliances, molars and incisor, patients with psychological disorders and craniofacial abnormalities were excluded from the study. Each study participant signed a written informed consent form pertaining to the study protocol drafted in accordance with the Helsinki Declaration of 1975 (Revised in 2013) for Medical Research.
Diode Laser (Model- FD10B, Faith Innovations, New Delhi, India)
[Table/Fig-1] depicts the Diode laser used in this study having wavelength of 980 nm with max power 10 W and pulse duration of 30 micro seconds to ten seconds and a repetition rate of 0.05 Hz to 20 KHz.
Diode Laser (Model- FD10B, Faith Innovations, New Delhi, India).

Desensitising Agent
[Table/Fig-2] depicts Shield Active Dentin Desensitiser manufactured by Prevest Denpro Limited, Jammu, India. It is a HEMA based DA with a chemical composition of 2-HEMA=45%, Glutaraldehyde=10% and Potassium Nitrate=2.5% and Ethanol.

Clinical evaluation parameter: Baseline and postoperative follow-up of DH was assessed using Modified U.S. Public Health Service Criteria for DH assessment as described above [29].
Each canine tooth received two stimuli: Clinical Probing and Air Blast. Clinical tactile stimulus by probing was performed by a dental explorer by running it along the cervical areas of the tooth under slight manual pressure in mesio-distal direction. Air blast stimulus was done by a three-way syringe connected to an air compressor at a standardised air pressure of 60 psi monitored through a pressure gauge fitted on the dental chair. Application of air blast was done for one second at distance of 1 cm from the tooth surface. The subjective experience of pain at baseline was recorded for each study participant bilaterally. Study participants with bilateral maxillary canine pre-treatment baseline sensitivity score Charlie=3 (High Sensitivity) were included in the study. After recording the pretreatment baseline scores, mouth of each sample subject was divided bilaterally using split-mouth technique into Group A and Group B. The left side of patient’s mouth was designated as Group A in which a 10 W Diode Laser (980 nm) [Table/Fig-1] was administered and right side of the patient’s mouth was classified as Group B, in which Shield Active DA [Table/Fig-2] was used. Sensitivity scores for each tooth in both Group A and B were calculated on a four time duration scale by assessing immediately after application, after 24 hours, after seven days and after 21 days.
Four patients were lost due to incomplete follow-up during the course of the study. Thus, application of statistical tests and subsequent analysis was done on a final sample size of 30 patients.
[Table/Fig-3] depicts the detailed study protocol showing the enrolment of subjects and review up to 21 days.
Flowchart of the study protocol showing the enrolment of subjects and review up to 21 days.
Procedure for Application of Dental Laser
After measuring the baseline sensitivity score Isolation of the tooth to be treated was done using rubber dam {Optradam by Ivoclar Vivadent, Schaan, Liechtenstein®.} followed by application of Diode laser at 2 Watt Power on repeat mode (T on 30 ms- T off 30 ms) for a total time period of 60 seconds [26]. The sensitivity score was measured immediately after application, after 24 hours, after seven days and after 21 days time interval. The individual scores were recorded in a tabulated data sheet.
Procedure for Application of Desensitising Agent
After measuring the baseline sensitivity score, isolation of the tooth to be treated was done using rubber dam (Optradam by Ivoclar Vivadent, Schaan, Liechtenstein®). The exposed dentin was cleaned and rinsed with water. The surface to be treated was left to dry. Minute quantity of DA was applied to the dentine surface in a thin layer with brush and left for 30 to 60 seconds to dry, subsequently a second layer application of the DA was also applied and the tooth was allowed to dry. Postapplication sensitivity scores were measured immediately after application, at 24 hour, after seven days and after 21 days time interval.
Statistical Analysis
The data obtained was subjected to statistical analysis with the consultation of a statistician. The data so obtained was compiled systematically. A master table was prepared, and the total data was subdivided and distributed meaningfully and presented as individual tables with graphs. Statistical Analysis was done by using Statistical Software for the Social Sciences (SPSS) software version 22.0. Student’s t-test was applied to compare mean sensitivity score between two groups. Repeated Measures of ANOVA Test was applied to find difference in mean score from baseline to 21 days. The p-value less than 0.05 was considered as significant.
Results
This split-mouth two-arm parallel design study was conducted on 30 patients with bilateral high DH scores of maxillary canine teeth. Out of 30 patients, 19 were males and 11 were females. Mean age of male patients was 50.94±13.62 years and of female patients was 55.18±10.28 years.
[Table/Fig-4,5] revealed comparative evaluation of sensitivity scores between Group A (Diode laser) and Group B (Desensitising agent) at Baseline (pre-treatment), immediately, after 24 hours, after seven days and after 21 days. Mean sensitivity scores were significantly less in Group A as compared to Group B immediately after treatment p=0.038, after 24 hours, seven days and 21 days p<0.001). Mean score was 0.13±0.50 and 0.53±0.90 immediately after treatment in Group A and Group B, respectively and after 21 days of follow-up it was increased to 1.03±1.06 and 2.53±0.50 in Group A and Group B, respectively. Thus, it can be inferred that 980 nm diode laser depicted high efficacy over HEMA based DA.
Comparative evaluation of sensitivity scores between Group A (Diode laser) and Group B (Desensitizing agent) at baseline, 24 hrs, 7 days and 21 days.
| Group | Sensitivity score |
|---|
| Immediately after application | 24 hours | 7 days | 21 days |
|---|
| Mean±SD | Mean±SD | Mean±SD | Mean±SD |
|---|
| Diode laser (N=30) | 0.13±0.50 | 0.27±0.69 | 0.53±0.90 | 1.03±1.06 |
| Desensitising agent (N=30) | 0.53±0.90 | 1.23±1.04 | 2.23±0.77 | 2.53±0.50 |
| Student ‘t’ test value | 2.121 | 4.239 | 7.847 | 6.958 |
| Significance ‘p’ value | 0.038 (S) | 0.001 (HS) | 0.001 (HS) | 0.001 (HS) |
S: Statistically significant HS: Highly significant
Comparative evaluation of sensitivity score between Group A (Diode Laser) and Group B (Desensitizing agent) at baseline, Immedietly after Treatment, 24 hrs, 7 days and 21 days.
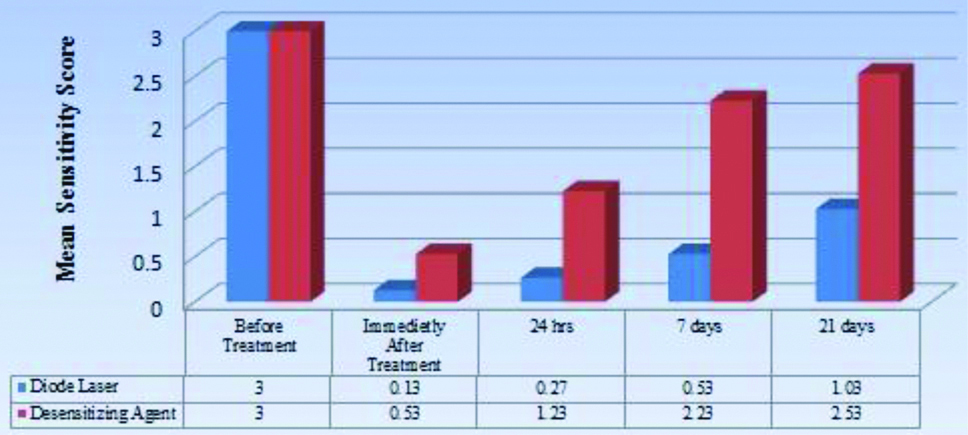
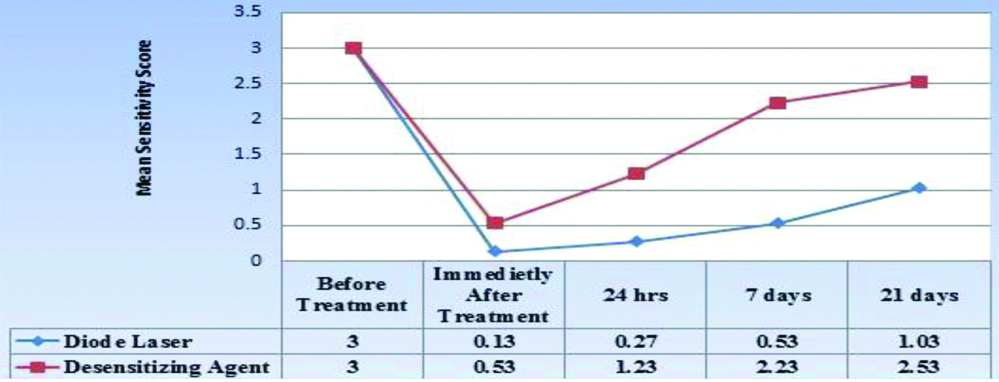
[Table/Fig-6,7] revealed evaluation of sensitivity scores from baseline to immediately after treatment upto 21 days within Group A and Group B. Repeated measures of ANOVA test applied through general linear model revealed highly significant differences in sensitivity scores from baseline, immediately after treatment to 21 days in both groups A and B, p<0.001.
Evaluation of sensitivity scores from baseline (PreTreatment) to 21 days within Group A (Diode Laser) and Group B (Desensitising Agent).
| Group | Sensitivity score | Repeated measure of ANOVA F value | Significance ‘p’ value |
|---|
| Baseline | Immediately after application | 24 hours | 7 days | 21 days |
|---|
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD |
|---|
| Diode laser | 3±0.00 | 0.13±0.50 | 0.27±0.69 | 0.53±0.90 | 1.03±1.06 | 13.514 | 0.001 (HS) |
| Desensitising agent | 3±0.00 | 0.53±0.90 | 1.23±1.04 | 2.23±0.77 | 2.53±0.50 | 70.601 | 0.001 (HS) |
S: Statistically significant; HS: Highly significant
Evaluation of sensitivity score from baseline to 21 days within Group A (Diode laser) and Group B (Desensitizing agent).
[Table/Fig-8] showed that immediately after application the results in Group A compared to baseline were statistically highly significant (p<0.001) and statistically significant in Group B (p<0.05). However, overall difference after 21 days compared to baseline were not significant in any group (p>0.05) depicting that the effect of both the desensitising therapies did not last beyond 21 days in both the groups and thus, illustrating that the highly significant results achieved were not permanent. p<0.05 statistically significant.
Comparison between Baseline Scores, Immediate post-treatment and final post-treatment sensitivity scores at 21 days in Group A and Group B.
| Baseline sensitivity score | Immediate post-treatment score from baseline | Significance ‘p’ value (Immediate post-treatment from baseline) | Post-treatment sensitivity score after 21 days from baseline | Significance ‘p’ value (Post-treatment after 21 days from baseline) |
|---|
| Group A | 3±0.00 | 0.13±0.50 | p<0.001 | 1.03±1.06 | p>0.05 |
| Group B | 3±0.00 | 0.53±0.90 | p<0.05 | 2.53±0.50 | p>0.05 |
Discussion
Dentinal Hypersensitivity is a chronic dental problem with different treatment modalities but not having a conclusive prognosis [31]. The treatment needs of a patient with DH depend on various parameters like the aetiological factors, degree of tolerance of pain and subjective perception of this sensation [32]. DH pain can be managed by blocking the nerve endings of odontoblastic processes and occluding or narrowing of tubules which may help in reducing fluid movement inside the dentine [31]. Kakaboura A et al., in their study stated that although there are many modalities for treatment of DH but there persists no modality that can resolve DH satisfactorily [33]. Abundant literature supports the use of DA in DH cases [3,14,33-36]. Although, Topical desensitising agents have few drawbacks such as repeated application, longer treatment time, and patient compliance but it still remains the most common method in treatment of DH [20]. Shield Active DA used in this study is a 2-HEMA (45%) based DA with Glutaraldehyde (10%). Ozlem K et al., claimed that HEMA polymerisation takes place, which leads to the formation of deep tags so that the dentinal tubules are completely or partially obliterated and the DH is consequently reduced [34]. HEMA is water soluble and its effects are reversible [35,36].
Glutaraldehyde which is another chemical component in Shield Active DA causes coagulation of amino acids and proteins in dentinal tubules and is effective in sealing them [35]. Potassium nitrate (KNO3), a minor chemical ingredient in Shield Active DA acts by lowering nerve sensitivity by reducing nerve excitation as the potassium ions block the synapse between the nerve cells [14]. Present study statistically demonstrated that topical application of DA reduced the preoperative high DH score (Charlie) from 3±0.00 to 0.53±0.90 immediately postapplication. However, this score gradually increased to 2.53±0.50 on the 21st day possibly due to limitation of water solubility and reversible effects of HEMA which is a major chemical component of Shield Active DA used in this study [35,36].
The results of this study were very similar to a clinical trial conducted by Tabatabaei MH who studied the efficacy of Nd:YAG laser, Diode Laser and Dentin Bonding agent (HEMA Based) in DH reduction on 135 teeth of 22 patients diagnosed with DH. The sensitivity scores in the Dentin Bonding agent group significantly reduced immediately (1.03±0.90; p<0.05) after treatment compared to baseline (2.46±0.69) but progressively increased (1.49±0.96) after one month and still further to a period of six months post-treatment (2.54±0.65; p>0.05). No precise cause for the observations made in the study have been discussed by the authors. However, the study states that the bonding agent forms resin tags on the surface and results in protein deposits in deeper layers of dentin causing alteration in intra-tubular fluid movement. This may explain the immediate temporary DH reduction [3]. The results of the present study are also in consonance to another research conducted in 2009 by Aranha AC et al., using GLUMA DA on 20 teeth which demonstrated significant improvements post treatment immediately, one week and four weeks from baseline [37].
Lasers are the newer treatment option for DH. The use of lasers has increased rapidly in the last few years [31,38]. In present study, we have used 980 nm 10 Watt diode lasers which is most commonly used wavelength in cases of endodontics and periodontics [10]. They can be modulated in continuous wave or pulsed mode [16]. A 980-nm diode laser acts by absorption of laser energy by the dentine inorganic component like carbonate and phosphates causing melting effect and crystalline arrangement [17,39].
Umberto R et al., conducted a clinical study in which they concluded Diode laser as a useful device for DH treatment similarly Bilichodmath R preferred diode laser for DH treatment [22,40].
Tabatabaei MH conducted a clinical trial to compare the efficacy of Diode Laser, Nd:YAG laser and HEMA based DA as a treatment for reduction of DH in 22 patients. The results in diode laser group illustrated statistically significant immediate post treatment reduction (1.18±0.91; p<0.05) in pain score from baseline (2.49±0.66). However, later during the study period the pain score demonstrated steady increase and was found to be statistically not significant (p>0.05) after 3 (1.84±0.60) and six months (2.13±0.62). Authors in this study explained the immediate effect of reduction in DH by laser attributed to the analgesic effect it creates which causes pain relief. The secondary/delayed effects of lasers are due to direct irradiation of the pulp which causes activation of odontoblast resulting in reparative dentin formation [3]. A period of three months or more is required for the reparative dentin to form so as to cause blockage of tubules post-irradiation by laser [3,18,41]. Present results exhibited steady increase in both Group A and Group B during the course of the study period of 21 days which may be explained by-1) The study conducted by Bechir A et al., on DA treated tooth reported that DA occluding dentinal tubules may get removed by daily tooth brushing activities, with usage of aerated acidic beverages or dissolution by salivary contents which leads to short-term desensitising effects and 2) water solubility of HEMA as explained by Schüpbach P [35,36].
Diode lasers may not be clinically effective as an desensitising therapy in one application was concluded by a randomised split-mouth clinical trial by Osmari D et al., who were assessing the effectiveness of four in-office desensitising therapies including Diode Laser after one single application [42].
Limitation(s)
A larger sample size and longer study time period for measuring the sensitivity score is recommended. In-vitro Scanning Electron Microscopic and thermal imaging studies may be done in future to view any microscopic changes on the tooth structure after application of laser therapy. Long-term comparative studies need to be done using different dental lasers at various wavelengths and power settings to make a statement regarding their effectiveness and proposing a conclusive treatment protocol for managing DH. Further, repeated multiple applications of desensitising therapy at regular time intervals are required for possible long-term effects in treatment of DH.
Conclusion(s)
Within the limits of this study, it can be concluded that both HEMA based DA and 980 nm Diode laser were effective desensitisation treatment modalities for achieving immediate reduction of high cervical dentin hypersensitivity from baseline. Further, 980 nm Diode laser was found to be more efficacious and effective treatment option than HEMA based DA for temporary resolution of DH after 24 hours lasting up to 21 days. However, for prolonged relief in DH better irradiation treatment options or combination modalities may be explored since results of sensitivity score in present study after 21 days from baseline did not demonstrate statistical significance in both the study groups.
S: Statistically significant HS: Highly significant
S: Statistically significant; HS: Highly significant