Introduction
The prognosis of root canal therapy depends on three dimensional hermetic seal and biomechanical preparation. Inability to locate root canal results in recurrent infection leading to failure of root canal therapy [1].
In a review of literature, it is stated that maxillary first premolars comprised of single root in 41.7% or two rooted in 56.6% and three rooted in 1.7%. Irrespective of number of roots, two root canals are presented in 86.6% and root canal configuration comprises of type IV (64.8%), type II (13.5%) and type I (11.4%) [2].
In a similar literature quoting clinical considerations in maxillary first molar stated the presence of three roots in 95.9%, two roots in 3.9%, fused two or three roots in 5.2% and rarely c-shaped roots (0.12%) [3]. Presence of variations in each root is also published as in mesiobucccal roots two canals in 56.8% and single canal in 43.1%, one distobuccal canal was contained in one root in 98.3% and palatal root has one canal in 99% cases [3].
Thews ME et al., reported two cases of two canal two roots, one root two canals fusing to a common foramina configuration [4]. Some of the authors also reported a single palatal root containing two separate orifices and root canals and also one orifice, a bifurcated canal, and two foramina [5,6]. Very few clinicians have reported presence of three palatal canals and its occurrence seems too rare [7,8].
Normal anatomy of mandibular first molar constitutes two roots with either three or four root canals [9]. Number of root canals are mostly three canals in 61.3%, four canals in 35.7%, and five canals in 1%. Canal configuration of the mesial root configuration showed two canals in 94.4%, three canals in 2.3% and comprised of Vertucci type IV (52.3%) and type II 35%) configuration. Distal Root canal configuration consisted of type I in 62.7%, types II (14.5%) and IV (12.4%) [9].
Because of the two dimensional nature of conventional radiography, it does not consistently reveal the actual number of canals present in teeth [10]. Root architecture and morphology can be visualised by three dimensional CBCT imaging in cases where conventional radiography fails to provide enough data [11].
This case series reports successful, non-surgical management of maxillary first premolar with three roots, and three root canals, three palatal canals in single palatal root canal anatomy of a maxillary molar, a mandibular first molar with three canals in distal root using CBCT.
Case Report 1
A 25-year-old male patient of Indian origin reported to the Department of Dentistry with a chief complaint of pain in left upper back tooth since few months. Pain was spontaneous, throbbing, localised, radiating pain aggravated on taking hot, cold and on sleeping, relieved after few hours automatically or on medication. It was not associated with any systemic signs and symptoms. Patient’s medical history, family history was non-contributory. There was no significant past dental history. Clinically, there was visible discoloration and deep cavity seen on the mesial surface of 26. Intraoral periapical radiograph revealed radiolucency on mesio-occlusal aspect of tooth involving pulp and there were no signs of periapical involvement suggestive of irreversible pulpitis in relation to 26 [Table/Fig-1a]. There was an exaggerated response to cold (ice piece), heat (gutta-percha stick), and electric pulp testing (Parkell Electronics Division, Farmingdale, NY) suggestive of acute pulpitis. Hence, it was diagnosed with acute irreversible pulpitis requiring endodontic therapy.
Preoperative radiograph of 26 [1a]; Modification of access cavity preparation 26 [1b]; CBCT image of 26 [1c] 1C1: Axial view -Cervical section, 1C2:Axial view -Middle section,1C3:Axial view -Apical section; CBCT image of 26 [1d]1D1: Coronal section,1D2: Saggital section,1D3: 3D-view; Radiograph of 26 for determination of working length showing 3 canals [1e]; Obturation radiograph of 26 [1f]; Postobturation clinical image of 26 [1g].
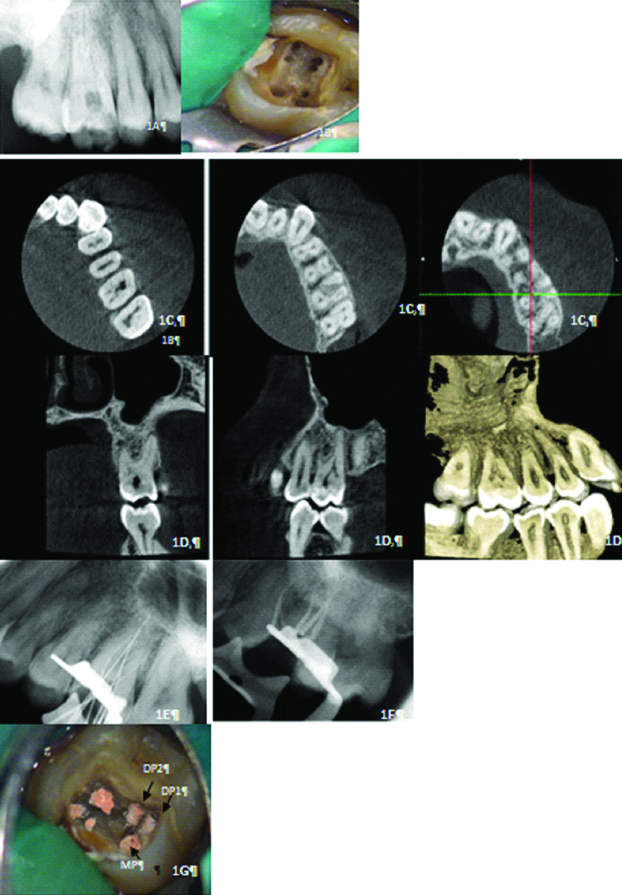
The patient was prepared for endodontic treatment of left maxillary first molar and received local anaesthesia of 2% lidocaine with 1:80,000 epinephrine. Rubber dam was used for isolation and a conventional endodontic access cavity opening was prepared. After extirpation of the coronal pulp, probing was done with a DG16 endodontic explorer. Three principal root canal orifices-mesiobuccal, distobuccal and palatal and also a small haemorrhagic point was noted adjacent to the large palatal orifice. The conventional access was slightly gauged palatally to additional canals, to get access to distopalatal 1 (DP1) and distopalatal 2 (DP2) [Table/Fig-1b]. The presence of extra canal in palatal root was suspected and hence CBCT was advised for confirmation. The CBCT confirmed the presence of extra canals in palatal root of Al-Quadah Awawdeh Type XXII canal configuration (3-2-1) [Table/Fig-1c,d]. The working length of each canal was estimated by using apex locator (Root ZX Mini, JMorita, Japan), and confirmed with intraoral periapical radiograph [Table/Fig-1e]. The canals were initially instrumented with #15 nickel-titanium files (Dentsply Maillefer) under irrigation with 5.25% sodium hypochlorite. Biomechanical preparation was performed using the crown-down technique with nickel-titanium rotary instruments (Protaper, Dentsply India Pvt., Ltd., Bengaluru, Karnataka, India). The mesiopalatal canal was enlarged till F2, 25.08% file. DP1, DP2, mesiobuccal, MB2 and, distobuccal enlarged till F1, 20.07%. Master cones were confirmed, sealing of root canal space was done with gutta-percha and AH plus resin sealer using lateral condensation technique and tooth was restored with a posterior composite filling [Table/Fig-1f,g]. Crown was placed within three days. The patient was asymptomatic when reviewed three months later. Pulp vitality tests were repeated at the review appointment, there was no response to it.
Case Report 2
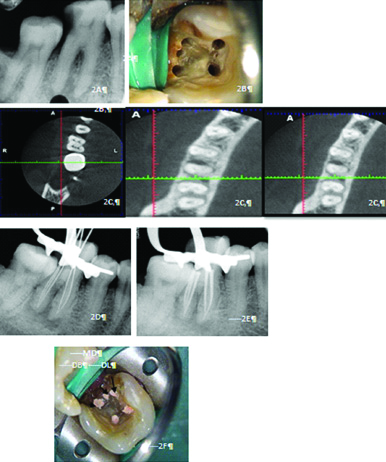
A 34-year-old female patient with a chief complaint of pain and swelling in her lower left back region of the jaw since few months, reported to Department of Conservative Dentistry and Endodontics. Pain was spontaneous, throbbing, localised, radiating pain aggravated on taking hot, cold and on sleeping, relieved after few hours automatically or on medication. Medical and family history was non-contributory. On clinical examination, a deep carious lesion associated with the mandibular left first molar 36 was found. On evaluation of the pulp status, tooth showed no response with cold (ice piece), heat (gutta-percha stick), and electric pulp testing (Parkell Electronics Division, Farmingdale, NY) revealed non-vital tooth with respect to 36 [Table/Fig-2a]. The patient was prepared for endodontic treatment of left mandibular first molar and received local anaesthesia of 2% lidocaine with 1:80,000 epinephrine. The tooth was isolated by rubber dam and a conventional endodontic access opening was made. After removing the coronal pulp and probing with a DG16 endodontic explorer, four principal root canal orifices-mesiobuccal, mesiolingual, distobuccal and distolingual and also a small haemorrhagic point was noted in between the two distal canals called to be middle distal canal. No modification was done to the conventional access cavity [Table/Fig-2b]. The presence of extra canal between two distal canals was confirmed by using CBCT and Gulabivwala k Type I (3-1) canal pattern was seen [Table/Fig-2c]. The working length of each canal was estimated by using apex locator (Root ZX Mini, JMorita, Japan), and confirmed with intraoral periapical radiograph [Table/Fig-2d]. The canals were initially instrumented with #15 nickel-titanium files (Dentsply Maillefer) under irrigation with 5.25% sodium hypochlorite. Biomechanical preparation was performed using the crown-down technique with nickel-titanium rotary instruments (Protaper, Dentsply India Pvt., Ltd., Bengaluru, Karnataka, India). The mesiobuccal, mesiolingual, distobuccal and distolingual till enlarged till F2, 25.08% file, and middle distal canal enlarged till F1 20.07%. Master cones were confirmed, sealing of root canal space was done with gutta-percha and AH plus resin sealer using lateral condensation technique and tooth was restored with a posterior composite filling [Table/Fig-2e,f]. Metal ceramic crown was placed to 36 after a week.
Preoperative radiograph of 36 [2a]; Access cavity preparation 36 [2b]; CBCT image of 36 [2c]; 2C1: Axial View-Cervical Section; 2c2: Axial View-Middle Section; 2c3: Axial View-Apical Section; Radiograph of 36 for determination of working length showing 3 canals [2d]; Postobturation radiograph of 36 [2e]; Postobturation image of 36 [2f]
Case Report 3
A 28-year-old male patient with a chief complaint of pain and swelling in his upper front right region of the jaw since one week reported to Department of Conservative Dentistry and Endodontics. Medical and family history was non-contributory. He had met with a road traffic accident few years back. Severe pain in 11, 12 was started seven months back forcing him to visit dentist. He was advised root canal treatment for 11, 12, and 13. He didn’t undergo any treatment as pain subsided with medication. Occasionally, he experienced dull localised pain in the same region making him to visit dentist. He reported to us in the Department of Dentistry. Thermal and electric pulp testing revealed no response with 11,12,13 and 14, radiographic examination showed large periapical radiolucency involving root apex of 11, 12, 13 and palatal 14 [Table/Fig-3a]. To determine extent of lesion, the patient was advised three dimensional radiographs. CBCT showed presence of three roots and three canals with tooth number 14 (vertucci type VIII) [Table/Fig-3b]. Patient was prepared for endodontic treatment of all the infected teeth and review for surgical excision of lesion.
Preoperative radiograph of 11, 12, 13, 14 [3a]; CBCT images of 14 [3b]; (3B1: Axial View -Cervical Section; 3B2: Axial View -Middle Section; 3B3: Axial View -Apical Section; 3B4: Coronal Section; 3B5: Saggital Section; 3B6: 3D VIEW); Radiograph of 14 for determination of working length showing 3 canals [3c]; Postobturation radiograph of 14 [3d].
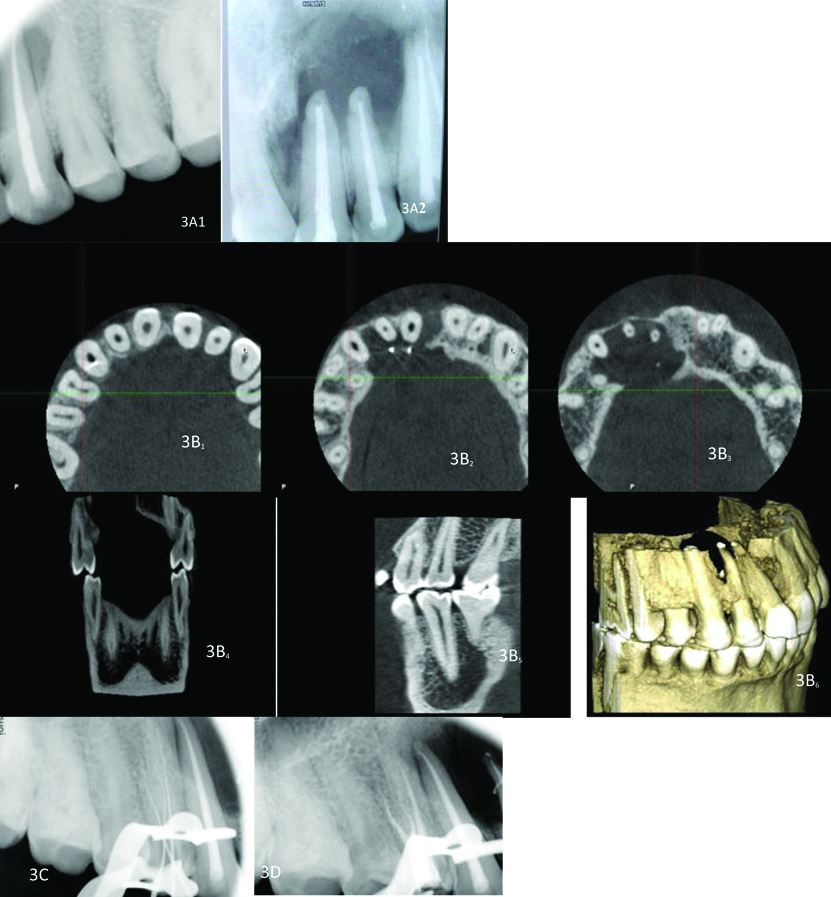
The patient was prepared for endodontic treatment of left maxillary first premolar and received local anaesthesia of 2% lidocaine with 1:80,000 epinephrine. A rubber dam was placed and a conventional endodontic access opening made. After removing the coronal pulp and probing with a DG16 endodontic explorer, two principal root canal orifices-buccal, palatal and; in addition, a small haemorrhagic point were noted adjacent to the buccal orifice. The conventional access was modified to a T-shape to improve access to additional canal. The working length of each canal was estimated by means of an apex locator (Root ZX Mini, J Morita, Japan), and confirmed with intraoral periapical radiograph [Table/Fig-3c]. The canals were initially instrumented with #15 nickel titanium files (Dentsply Maillefer) under irrigation with 5.25% sodium hypochlorite. Biomechanical preparation was performed using the crown-down technique with nickel-titanium rotary instruments (Protaper, Dentsply India Pvt., Ltd., Bengaluru, Karnataka, India). The palatal canal was enlarged till F2, 25.08% file, mesiobucal and, distobucal enlarged till F1, 20.07%. Master cones were confirmed, sealing of root canal space was done with gutta-percha and AH plus resin sealer using lateral condensation technique and tooth was restored with a posterior composite filling [Table/Fig-3d]. Patient was asked for review after one month or if he is symptomatic. After one month, patient was found to be asymptomatic hence, crowns were placed and patient was called after three months.
In all the three cases, patients were comfortable, well-tolerated the long procedure and there were no complications related to CBCT or the root canal treatment. No genetic analysis or significant genetic history was elucidated.
Discussion
Effective management of endodontic therapy requires good understanding, perceiving and recognising the morphology, anatomy of roots and root canal. The diagnosis and management of extra roots or root canals pose an endodontic challenge. Missing a canal and obturating it is the main cause for failure of endodontic treatment. It aggregates to 42% in the endodontic failure teeth [12]. Thus, a careful understanding and diagnosis of canal anatomy are of utmost importance for the successful management of such cases.
The management of these should start sequentially from preoperative clinical assessment, radiography and advanced radiography.
Clinical Assessment
Preoperative clinical assessment of the crown structure can hint the variations in root canal system. If the mesiodistal width of crown is more compared to buccolingual width; it may indicate presence of extra roots or root canals because dentinogenesis occurs around the canal [13]. If the tooth is carious and its structure is damaged the contralateral tooth might hint you the structure. Assessing the dentinal map, use of DG 16 in locating the orifice, laws of symmetry in canal orifice location and checking for sodium hypochlorite effervescence at the canal orifice are other clinical methods to check extra canals [1].
Radiographic Assessment
Preoperative radiographic evaluation is an important adjuvant to determine the number of roots and root canals. Preoperative intraoral periapical radiographs taken in paralleling technique with angulated radiographs mesial and distal can identify the number of roots.
According to Sieraski SM et al., if in a radiograph image mesiodistal dimension at the mid-root is more than mesiodistal dimensions of crown there can be a possibility of three-roots in maxillary premolars [14]. Researchers also stated that if in two consecutive X-rays a well-defined broad image of root canal fades off or narrows, it can be considered as a sign that there is deviation from normal anatomy and could be division of root [15,16]. Hence, accurate preoperative radiographs can hint the presence of variations.
If in a working length radiographic image with a smaller file and in distal projection taken after initial negotiation, if an endodontic file deviates from the centre of the root, an extra canal can be suspected [1].
Advanced Radiographic Imaging
Advanced radiography such as CT, Spiral CT, CBCT are of great importance in endodontics. CBCT imaging could be a part of daily endodontic practice starting from diagnosis to the management of endodontic lesions and its importance in determining the morphology and configuration of roots is invaluable [17,18].
In a conventional radiography, a three-dimensional structure is converted into two dimensional image leading to loss of information. CBCT overcomes the limitations of two-dimensional imaging by limiting unwanted shadows, geometric distortions, and superimpositions and also creating high-resolution 3D images root canal systems.
CBCT has a distinct advantage over conventional CT scans in limiting X-ray beam, rapid scan time and reduction of dose [18,19].
In an in-vitro study evaluating the efficacy of CBCT, spiral CT, peripheral Quantitative CT (pQCT) peripheral quantitative CT and digital radiographs were identification of root canal configuration, the percentage of evaluators failing to identify highest in digital radiography (23.8%) followed by contrast medium-enhanced digital radiographs (14.8%), spiral CT (15.58%), pQCT in (2.05%) and least was CBCT (0.29%.). It was concluded that the difference is mainly attributed to the slice thickness in CBCT which was least in CBCT followed by pQCT and spiral CT [20].
With all the advantages CBCT also has its limitations. Metallic restorations can create artifact-like images [21]. The duration of imaging is significantly more compared to the conventionally periapical radiography which could be difficult in geriatric, pediatric and patients with nervous disorders [22]. The dose of radiation is a concern addressed by The European Society of Endodontology stating the use of it only when additional information is required [23]. The cost is much more expensive compared to the conventional radiograph. Reliability of diagnostic value of CBCT is questioned by few researchers mainly in differentiating periapical pathologies comparing to histopathology [24]. Others stated it can differentiated based on positive and negative grey scale. However, it was questioned whether all CBCT can scan these as true lesions [24].
In the present case, CBCT scanning was used for a better understanding of the complex root canal anatomy. CBCT axial images confirmed the Gulabivwala k Type I (3-1) canal pattern in distal root of 36 and in palatal root of maxillary first molar Al- Quadah Awawdeh Type XXII (3-2-1) canal configuration [25,26]. CBCT axial images also confirmed three roots in maxillary first premolar with vertucci type VIII canal configuration. Tabulation of similar cases reported in the literature is presented in [Table/Fig-4,5 and 6] [7,8,27-35].
Review of case reports with three palatal canals in maxillary first molar in a single root [7,8].
| Author | Side | No. of roots | Number of palatal canals | Canals | Apical foramina |
|---|
| Wong M [7] | Right | 1 | 3 | DP1, DP2, MP | 3 |
| Maggiore F et al., [8] | Left | 1 | 3 | DP1, DP2, MP | 3 |
| Present case series | Left | 1 | 3 | DP1, DP2, MP | 3 |
Review of case reports with three distal canals in mandibular first molar in a single root [27-30].
| Author | Side | No. of roots | Number of distal canals | Distal root configuration |
|---|
| Reeh ES [27] | Left | 1 | 3 | MD, DL, DB |
| Chandra SS et al., [28] | Right | 1 | 3 | MD, DL, DB |
| Jain S [29] | Right | 1 | 3 | MD, DL, DB |
| Kottoor J et al., [30] | Right | 1 | 3 | MD, DL, DB |
| Present case series | Left | 1 | 3 | MD, DL, DB |
Review of case reports with three roots and three canals in maxillary first premolar [31-35].
| Author | Tooth number | No. of roots | Canal configuration | Population |
|---|
| Praveen R et al., [31] | 14 | 3 | MB, DB, P | Indian |
| Mathew J et al., [32] | 14 | 3 | MB, DB, P | Indian |
| Sathyanarayana K et al., [33] | 14 | 3 | MB, DB, P | Indian |
| Theruvil R et al., [34] | 24 | 3 | MB, D, MP | Indian |
| Agarwal PM and Taneja S [35] | 14 | 3 | MB, DB, P | Indian |
| Present case series | 14 | 3 | MB, DB, P | Indian |
This case series describes and strengthens the role of CBCT in patients where 2D radiographs questions or doesn’t clearly demarcate the association of lesion with the tooth just as in case report three. It also stresses on importance of CBCT not only in detection of variations in root canal architecture and but also to track down the anatomy from cervical to apical in various sections [36]. But, it has its own limitations such as the final outcome of treatment should be assessed for at least four years, meaningfully disappearance of lesion completely [37]. Though CBCT has help in determination, buying the equipment and its maintenance is too expensive at the clinical level. Hence, patient is referred to a diagnostic centre which is time-consuming. The radiation dose is less compared to conventional CT but it is higher than periapical radiograph. Hence, the guidelines states that it should be used in cases where only benefits overweigh risks. Therefore, alternative to CBCT in terms of dose has to be focused [23].
Conclusion(s)
Precise diagnosis, treatment planning, and knowledge of the root canal anatomy aids in successful endodontic treatment. Advanced imaging techniques such as CBCT is a valuable adjuvant diagnostic, imaging, in managing cases with variations. The present case series re-emphasises the role of CBCT in treating variations in root canal anatomy. Hence, it should recommended according to the literature CBCT studies and guidelines, cost aspects to restrict its use in cases where there is a deviation from the normal anatomy.
[1]. Cantatore G, Berutti E, Castellucci A, Missed anatomy: Frequency and clinical impactEndod Topics 2006 15(1):03-31.10.1111/j.1601-1546.2009.00240.x [Google Scholar] [CrossRef]
[2]. Ahmad IA, Alenezi MA, Root and root canal morphology of maxillary first premolars: A literature review and clinical considerationsJ Endod 2016 42(6):861-72.10.1016/j.joen.2016.02.01727106718 [Google Scholar] [CrossRef] [PubMed]
[3]. Cleghorn BM, Christie WH, Dong CC, Root and root canal morphology of the human permanent maxillary first molar: A literature reviewJ Endod 2006 32(9):813-21.10.1016/j.joen.2006.04.01416934622 [Google Scholar] [CrossRef] [PubMed]
[4]. Thews ME, Kemp WB, Jones CR, Aberrations in palatal root and root canal morphology of two maxillary first molarsJ Endod 1979 5(3):94-96.10.1016/S0099-2399(79)80156-9 [Google Scholar] [CrossRef]
[5]. Sert S, Bayirli GS, Evaluation of the root canal configurations of the mandibular and maxillary permanent teeth by gender in the Turkish populationJ Endod 2004 30(6):391-98.10.1097/00004770-200406000-0000415167464 [Google Scholar] [CrossRef] [PubMed]
[6]. Stone LH, Stroner WF, Maxillary molars demonstrating more than one palatal root canalOral Surg Oral Med Oral Pathol 1981 51(6):649-52.10.1016/S0030-4220(81)80017-5 [Google Scholar] [CrossRef]
[7]. Wong M, Maxillary first molar with three palatal canalsJ Endod 1991 17(6):298-99.10.1016/S0099-2399(06)81871-6 [Google Scholar] [CrossRef]
[8]. Maggiore F, Jou YT, Kim S, A six-canal maxillary first molar: Case reportInt Endod J 2002 35(5):486-91.10.1046/j.1365-2591.2002.00533.x12059922 [Google Scholar] [CrossRef] [PubMed]
[9]. de Pablo OV, Estevez R, Péix Sánchez M, Heilborn C, Cohenca N, Root anatomy and canal configuration of the permanent mandibular first molar: A systematic reviewJ Endod 2010 36(12):1919-31.10.1016/j.joen.2010.08.05521092807 [Google Scholar] [CrossRef] [PubMed]
[10]. Bauman R, Scarfe W, Clark S, Morelli J, Scheetz J, Farman A, Ex vivo detection of mesiobuccal canals in maxillary molars using CBCT at four different isotropic voxel dimensionsInt Endod J 2011 44(8):752-58.10.1111/j.1365-2591.2011.01882.x21470249 [Google Scholar] [CrossRef] [PubMed]
[11]. Venskutonis T, Plotino G, Juodzbalys G, Mickevičiene L, The importance of cone-beam computed tomography in the management of endodontic problems: A review of the literatureJ Endod 2014 40(12):1895-901.10.1016/j.joen.2014.05.00925287321 [Google Scholar] [CrossRef] [PubMed]
[12]. Hoen MM, Pink FE, Contemporary endodontic retreatments: An analysis based on clinical treatment findingsJ Endod 2002 28(12):834-36.10.1097/00004770-200212000-0001012489654 [Google Scholar] [CrossRef] [PubMed]
[13]. Krasner P, Rankow HJ, Anatomy of the pulp-chamber floorJ Endod 2004 30(1):05-16.10.1097/00004770-200401000-0000214760900 [Google Scholar] [CrossRef] [PubMed]
[14]. Sieraski SM, Taylor GN, Kohn RA, Identification and endodontic management of three-canalled maxillary premolarsJ Endod 1989 15(1):29-32.10.1016/S0099-2399(89)80095-0 [Google Scholar] [CrossRef]
[15]. Bellizzi R, Hartwell G, Radiographic evaluation of root canal anatomy of in vivo endodontically treated maxillary premolarsJ Endod 1985 11(1):37-39.10.1016/S0099-2399(85)80104-7 [Google Scholar] [CrossRef]
[16]. Balthazard R, Corne P, Vincent M, Mortier E, Methodological approach to the endodontic treatment of first premolars with three root canals: Two case reportsJ Contemp Dent Pract 2019 20(2):263-69.10.5005/jp-journals-10024-250731058645 [Google Scholar] [CrossRef] [PubMed]
[17]. Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG, Endodontic applications of cone-beam volumetric tomographyJ Endod 2007 33(9):1121-32.10.1016/j.joen.2007.06.01117931947 [Google Scholar] [CrossRef] [PubMed]
[18]. Patel S, Dawood A, Ford TP, Whaites E, The potential applications of cone beam computed tomography in the management of endodontic problemsInt Endod J 2007 40(10):818-30.10.1111/j.1365-2591.2007.01299.x17697108 [Google Scholar] [CrossRef] [PubMed]
[19]. Gijbels F, Jacobs R, Bogaerts R, Debaveye D, Verlinden S, Sanderink G, Dosimetry of digital panoramic imaging. Part I: Patient exposureDentomaxillofac Radiol 2005 34(3):145-49.10.1259/dmfr/2810746015897284 [Google Scholar] [CrossRef] [PubMed]
[20]. Neelakantan P, Subbarao C, Subbarao CV, Comparative evaluation of modified canal staining and clearing technique, cone-beam computed tomography, peripheral quantitative computed tomography, spiral computed tomography, and plain and contrast medium-enhanced digital radiography in studying root canal morphologyJ Endod 2010 36(9):1547-51.10.1016/j.joen.2010.05.00820728725 [Google Scholar] [CrossRef] [PubMed]
[21]. Scarfe WC, Farman AG, What is cone-beam CT and how does it workDent Clin North Am 2008 52(4):707-30.10.1016/j.cden.2008.05.00518805225 [Google Scholar] [CrossRef] [PubMed]
[22]. Scarfe WC, Levin MD, Gane D, Farman AG, Use of cone beam computed tomography in endodonticsInt J Dent 2009 2009:63456710.1155/2009/63456720379362 [Google Scholar] [CrossRef] [PubMed]
[23]. Patel S, Durack C, Abella F, Roig M, Shemesh H, Lambrechts P, European Society of Endodontology position statement: The use of CBCT in endodonticsInt Endod J 2014 47(6):502-04.10.1111/iej.1226724815882 [Google Scholar] [CrossRef] [PubMed]
[24]. Rosenberg PA, Frisbie J, Lee J, Lee K, Frommer H, Kottal S, Evaluation of pathologists (histopathology) and radiologists (cone beam computed tomography) differentiating radicular cysts from granulomasJ Endod 2010 36(3):423-28.10.1016/j.joen.2009.11.00520171356 [Google Scholar] [CrossRef] [PubMed]
[25]. Gulabivala K, Aung TH, Alavi A, Ng YL, Root and canal morphology of Burmese mandibular molarsInt Endod J 2001 34(5):359-70.10.1046/j.1365-2591.2001.00399.x11482719 [Google Scholar] [CrossRef] [PubMed]
[26]. Al-Qudah AA, Awawdeh LA, Root and canal morphology of mandibular first and second molar teeth in a Jordanian populationInt Endod J 2009 42(9):775-84.10.1111/j.1365-2591.2009.01578.x19549153 [Google Scholar] [CrossRef] [PubMed]
[27]. Reeh ES, Seven canals in a lower first molarJ Endod 1998 24(7):497-99.10.1016/S0099-2399(98)80055-1 [Google Scholar] [CrossRef]
[28]. Chandra SS, Rajasekaran M, Shankar P, Indira R, Endodontic management of a mandibular first molar with three distal canals confirmed with the aid of spiral computerized tomography: A case reportOral Surg Oral Med Oral Pathol Oral Radiol Endod 2009 Oct 108(4):e77-81.10.1016/j.tripleo.2009.06.01719778737 [Google Scholar] [CrossRef] [PubMed]
[29]. Jain S, Mandibular first molar with three distal canalsJ Conserv Dent 2011 Oct 14(4):438-39.10.4103/0972-0707.8722322144821 [Google Scholar] [CrossRef] [PubMed]
[30]. Kottoor J, Sudha R, Velmurugan N, Middle distal canal of the mandibular first molar: A case report and literature reviewInt Endod J 2010 Aug 43(8):714-22.10.1111/j.1365-2591.2010.01737.x20491988 [Google Scholar] [CrossRef] [PubMed]
[31]. Praveen R, Thakur S, Kirthiga M, Shankar S, Nair VS, Manghani P, The radiculous’ premolars: Case reports of a maxillary and mandibular premolar with three canalsJ Nat Sci Biol Med 2015 Jul-Dec 6(2):442-45.10.4103/0976-9668.16003226283848 [Google Scholar] [CrossRef] [PubMed]
[32]. Mathew J, Devadathan A, Syriac G, Shamini S, Root canal treatment of a maxillary first premolar with three rootsJ Pharm Bioallied Sci 2015 Aug 7(Suppl 2):S746-48.10.4103/0975-7406.16353126538958 [Google Scholar] [CrossRef] [PubMed]
[33]. Sathyanarayanan K, Srinivasan MR, Balagopal S, Poornima L, Report of occurrence and endodontic management of three-rooted maxillary first and second premolars in the same individualIndian J Dent Res 2017 28(3):337-40.10.4103/ijdr.IJDR_65_1628722002 [Google Scholar] [CrossRef] [PubMed]
[34]. Theruvil R, Ganesh C, George AC, Endodontic management of a maxillary first and second premolar with three canalsJ Conserv Dent 2014 17(1):88-91.10.4103/0972-0707.12416624554870 [Google Scholar] [CrossRef] [PubMed]
[35]. Agarwal PM, Taneja S, Root Canal treatment of three rooted maxillary first and second premolar using CBCT: A case reportJCDR 2018 12(4):ZD06-08.10.7860/JCDR/2018/35190.11449 [Google Scholar] [CrossRef]
[36]. Tyndall DA, Rathore S, Cone-beam CT diagnostic applications: Caries, periodontal bone assessment, and endodontic applicationsDent Clin North Am 2008 52(4):825-41.10.1016/j.cden.2008.05.00218805231 [Google Scholar] [CrossRef] [PubMed]
[37]. Shekhar V, Shashikala K, Cone beam computed tomography evaluation of the diagnosis, treatment planning, and long-term follow-up of large periapical lesions treated by endodontic surgery: Two case reportsCase Rep Dent 2013 2013:56439210.1155/2013/56439223762646 [Google Scholar] [CrossRef] [PubMed]